A novel management of post-oesophagectomy gastro-pleural fistula
Introduction
Mega stents: conventional oesophageal stents carry the risk of migration or inability to cover the entire length of an oesophageal leak due to oesophagectomy. Several types of mega stents are routinely used in patients who have developed broncho-pleural complications secondary to sleeve gastrectomy. Their use in post-oesophagectomy gastro-pleural fistula has not been recorded in the literature before.
Case presentation
A 73-year-old male was diagnosed with moderately differentiated adenocarcinoma (T3N0M0) of the distal oesophagus. At the time of the diagnosis, the tumour had extended beyond the oesophago-gastric junction. Neo-adjuvant chemotherapy followed by laparoscopic oesophagectomy and gastric pull-up operation were carried out. The operation was challenging due to the presence of abdominal wall adhesions secondary to previous cholecystectomy and radiotherapy for Hodgkin’s disease administered 6 years ago. The oesophagectomy was complicated by anastomosis leak resulting into a gastro-pleural fistula and empyema of the right lung.
These complications were initially addressed with antibiotics, keeping the patient nil by mouth and feeding him through a nasojejunal tube. The patient also required repeated chest tube insertions to drain the empyema. Despite these measures, the fistulous tract failed to heal and resulted into a chronic empyema. A covered oesophageal self-expanding metal stent (SEMS) was then inserted to prevent the leak. The stenting helped stopping the leakage and improvement in patient’s general condition. The oral feed was recommenced and he was discharged from the hospital.
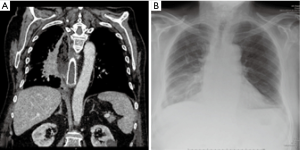
One month later, the patient was re-admitted with dyspnoea, high grade fevers and weight loss. A contrast computerised tomography (CT) scan revealed a large collection in the right pleural space (Figure 1). The needle aspiration of the collection sample confirmed this as an empyema.
The culture examination of the pus from the empyema revealed poly-microbial growth including Escherichia coli, Klebsiella pneumoniae, Enterococcus faecium and Candida glabrata.
Antibiotic and antifungal treatment was recommenced, and a new chest tube was inserted to drain the empyema. Patient’s oral feeding was stopped and he was given total parenteral nutrition. These measures failed to resolve the empyema over the next 2 weeks.
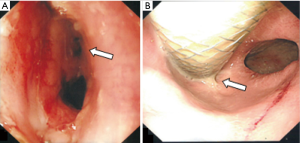
At this point, an oesophago-gastroduodenoscopy (OGD) was performed to deploy an additional oesophageal stent to cover the fistula tract. The OGD revealed that the previously deployed stent had displaced proximally. This exposed a large defect at the anastomosis site which resulted into the gastro-oesophageal leak and the gastro-pleural empyema (Figure 2). Due to the changed oesophago-gastric anatomy secondary to the surgery and a potential risk of stent migration, insertion of the additional stent deemed unreasonable.
In order to consider a possible surgical repair of the defect at the anastomosis site, the case was re-discussed in the multidisciplinary meeting. Due to his poor general health, history of non-Hodgkin’s lymphoma and exposure to radiotherapy in the past, the patient was deemed a high risk for surgery and was considered for palliative treatment only.
The patient’s general condition was rapidly deteriorating because of the persistent anastomotic leak and non-resolving empyema.
At this point, in order to cover the anastomotic fistula and to avoid the potential risk of stent migration, we adopted a novel approach to insert a mega stent.
A 20 French 22 mm × 230 mm covered SEM MegaTM stent (Taewoong Medical Niti-S oesophageal covered metal stent) (Figure 3) was endoscopically placed by our gastroenterology team. Utilizing conscious sedation and fluoroscopy the mega stent was deployed over the wire and through the existing oesophageal stent. The mega stent covered the entire fistulous tract, with its proximal end lying at the lower end of the previously deployed oesophageal stent and its distal end beyond the pyloric orifice.
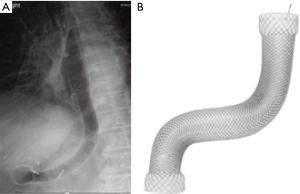
An oral gastrografin contrast X-ray of the chest and abdomen was performed after the stent insertion. The contrast flowed freely through the stent from the oesophagus into the duodenum, with no evidence of leakage into the surrounding tissues (Figure 4A-C).

After the successful deployment of the mega stent and the post-stenting encouraging results of the oral contrast test, the patient’s parenteral nutrition was switched to oral feed. Over the next few days his chest symptoms and general health considerably improved. The antibiotics were switched from intravenous to per oral route, and he was discharged home with a plan to be reviewed in the out-patient clinic. At follow up the patient’s general condition and respiratory symptoms remained stable, and a repeat chest X-ray did not show any worsening of the empyema (Figure 4D). He was then discharged from hospital care to the community-based palliative treatment.
Discussion
Oesophageal anastomotic leak and fistula are major and life-threatening complications of oesophagectomy. The rate of anastomotic leakage varies between 4% and 30% (1). Surgical re-exploration after the oesophagectomy is not always an option as the mortality rate with surgical treatment varies between 12% and 50% (2,3).
Isolated anastomotic leaks can be successfully managed with non-operative treatment, including antibiotics, nil by mouth, nasojejunal tube or parenteral feeding. This may also require an active drainage of empyema. In few selective cases the more extensive leaks require revisional surgery which carries a high mortality rate, up to 30% in some case series (4).
The endoscopic insertion of self-expandable covered stents for oesophageal perforation, leak or fistula is a safe and well-established therapeutic technique. The overall procedure-related mortality is about 2.2% (5). Stent migration is the potential associated complication, which can be as high as 26% (6). In order to minimize stent migration, using larger stents is a viable option (7). The patient described in this case report developed multiple and serious complications; including anastomotic leak, chronic empyema and a poor quality of life after the oesophagectomy and gastric pull up operation for his oesophageal cancer. The conventional therapeutic measures including antibiotics, parenteral nutrition and smaller oesophageal stent failed to resolve these issues. Moreover, the patient had already developed advanced fibrosis of the lungs due to chemo-radiotherapy for Hodgkin’s disease in the past. These adverse factors turned the patient into a high risk candidate for surgical re-exploration of the anastomotic leak, and left him with palliation as the only reasonable treatment option. To address these issues and complications and to keep the intervention at minimum, we adopted a novel approach to deploy a very large (MegaTM) stent. The larger stent completely covered the fistula and resulted into the cessation of the anastomotic leak. The patient was then able to re-start his oral feed and was discharged home with improved quality of life. This also allowed him to spend the last few months of his terminal disease with his family.
To our knowledge, this is the first reported case in the United Kingdom of the use of a mega stent for a gastro-pleural fistula developed as a result of oesophagectomy and gastric pull-up operation for oesophageal cancer. These mega stents are safe, easy to deploy and do not carry the risk of migration.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Leenders BJ, Stronkhorst A, Smulders FJ, et al. Removable and repositionable covered metal self-expandable stents for leaks after upper gastrointestinal surgery: experiences in a tertiary referral hospital. Surg Endosc 2013;27:2751-9. [Crossref] [PubMed]
- Kassis ES, Kosinski AS, Ross P Jr, et al. Predictors of anastomotic leak after esophagectomy: an analysis of the society of thoracic surgeons general thoracic database. Ann Thorac Surg 2013;96:1919-26. [Crossref] [PubMed]
- Salminen P, Gullichsen R, Laine S. Use of self-expandable metal stents for the treatment of esophageal perforations and anastomotic leaks. Surg Endosc 2009;23:1526-30. [Crossref] [PubMed]
- Turkyilmaz A, Eroglu A, Aydin Y, et al. The management of esophagogastric anastomotic leak after esophagectomy for esophageal carcinoma. Dis Esophagus 2009;22:119-26. [Crossref] [PubMed]
- Simmons DT, Baron TH. Endoluminal palliation. Gastrointest Endosc Clin N Am 2005;15:467-84. viii. [Crossref] [PubMed]
- van Boeckel PG, Sijbring A, Vleggaar FP, et al. Systematic review: temporary stent placement for benign rupture or anastomotic leak of the oesophagus. Aliment Pharmacol Ther 2011;33:1292-301. [Crossref] [PubMed]
- Baron TH. Minimizing endoscopic complications: endoluminal stents. Gastrointest Endosc Clin N Am 2007;17:83-104. vii. [Crossref] [PubMed]


