Mucinous adenocarcinoma of the appendix presenting as intussusception in 27 year old female
Introduction
While intussusception is commonly reported in children, it is quite unusual in adults almost always reported secondary to a definable lesion (1). Incidence secondary to adult intussusception has been estimated to range from 0.003% to 0.02% (2). Rarely, as in our case, the appendix may be the lead point for intussusception (3). Appendiceal intussusception may occur secondary to a number of etiologies including: villous adenoma, mucinous cystadenoma, endometriosis, and adenocarcinoma of the appendix (4-6). The incidence of epithelial malignancies of the appendix has been estimated to be 0.12 per 1 million persons per year (7). 5% of the total cases of intussusception (adults and children) have been reported in adults. Intussusception is reported as the underlying cause of 1-5% of adult cases of bowel obstruction (8). We will discuss our case, a 27 year female presenting with abdominal pain and a palpable abdominal mass, as well as briefly review the topic of appendiceal carcinoma.
Case presentation
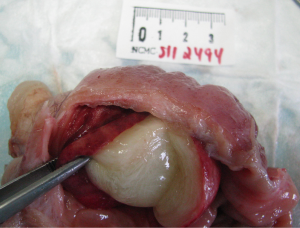
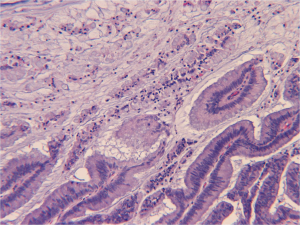
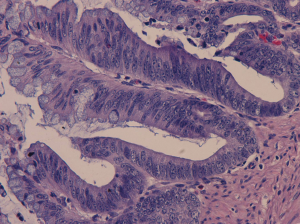
A 27 year-old Hispanic female G1P0202 presented to the emergency room with severe abdominal pain. She described a 2 day history of worsening intermittent “crampy” pain located in the periumbilical region that was exacerbated with touch. She also reported 3 episode of non-bloody vomiting earlier that day. Review of systems was unremarkable. Past medical and surgical histories revealed a caesarean section of twins one month prior for premature rupture of membranes at 35 weeks. She denied any social or family histories. Vitals were within normal limits. The abdomen was soft with normal bowel sounds and focal tenderness elicited on palpation of the right lower quadrant. On deep palpation a 3 cm hardened mass was found in the right periumbilical area. Laboratory findings revealed leukocytosis of 11.9 K (4.5-11.0 k/mm3). Complete blood count, coagulation profile, urine pregnancy, and basic metabolic panel were unremarkable. Liver related tests were mildly elevated: ALT-113 (0-31 U/L), AST-76 (0-32 U/L), alkaline phosphatase of 124 (39-117 U/L), total bilirubin of 1.2 (0.0-1.0 mg/dL). A CT of the abdomen/pelvis with oral and IV contrast revealed possible volvulus. A repeat CT of the abdomen/pelvis with rectal contrast was then ordered for further characterization demonstrating a suspicious rounded area of low attenuation with peripheral high density (appendix) as a lead point consistent with an intussusception (Figures 1,2). The patient was taken to the operating room where an exploratory laparotomy was performed urgently to relieve the intussusception. A midline excision was made extending from the xiphoid to the pubic symphysis. The uterus, fallopian tubes, and ovaries appeared grossly normal. On exploration of the abdomen intussusception was confirmed extending from the ileocecal region to the hepatic flexure. During reduction of the intussusception a 3.5 to 4.5 cm mass was uncovered in the appendix (Figure 3). Subsequently a right hemicolectomy was performed, containing 15 cm of the right colon in continuity with 3.5 cm of the terminal ileum (Figure 4). An end-to-end ileocolonic anastomosis was performed prior to closure. Macroscopically the surgical specimen revealed a smooth tan bulging 4.5 cm × 4.5 cm × 3.7 cm mass located in the appendix. There were multiple pink tan lymph nodes dissected ranging from 0.3 cm to 1.7 cm. Microscopically, the mass was found to be a mucinous (colloid) adenocarcinoma (Figures 5,6), histologically grade 1 (well differentiated). No lymphovascular or perineural invasion was found, with all margins free of tumor: AJCC tumor stage pTispN0Mx.



On post-operative day 3 she was started on a clear liquid diet and advanced to a full diet on the day of discharge, post-operative day 5. The patient followed up 1 week later in the outpatient surgical clinic with no reported post-operative complications and was discharged from the clinic.
Discussion
There are two types of primary carcinoma of the appendix, adenocarcinoma (epithelial origin) and neuroendocrine tumor (neuroendocrine origin, formerly called “carcinoid”). The adenocarcinoma type can further be broken down into mucinous and non-mucinous (colonic), while the neuroendocrine tumors can be broken down into signet, malignant, and goblet subtype. Adenocarcinoma of the appendix is estimated at around 0.2/100,000 per year, whereas neuroendocrine tumors are estimated around 0.075/100,00 per year (9,10). Tumors of the appendix are found in approximately 1% of appendiceal specimens submitted for pathologic examination (11). The National Cancer Institute’s Surveillance, Epidemiology and End-Results (Seer) program analyzed 1,645 appendiceal malignancy cases from 1973-1998. 37.2% of the cases were identified as mucinous adenocarcinoma, 24.9%, “colonic type”, 19.6% “malignant carcinoid”, 13.7% “goblet carcinoid”, and 4.3% “signet ring cell” carcinoma (12). Connor et al. reviewed a database of 7,970 appendectomies and found 74 patients with appendiceal tumors: 42 carcinoid, 12 benign, and 20 malignant (13).
Less than one third of mucinous appendiceal adenocarcinomas manifest as acute appendicitis, more commonly they are found incidentally on imaging studies as a cystic right lower quadrant mass or in a patient with increasing abdominal girth secondary to pseudomyxoma peritonei (11). CT is a sensitive technique for detecting the presence of an underlying appendiceal neoplasm. Changes such as the presence of cystic dilation of the appendix or a focal soft-tissue mass are present in the majority of cases (14). An appendiceal diameter greater than 15 mm is not specific, but this finding should be viewed with extreme suspicion of appendiceal malignancy. Although ultrasound (US) can be used to evaluate an abdominal mass CT is superior to US in regards to anatomical topography of an appendiceal adenocarcinoma with the ability to distinguish between cecum and mucocele, as well as the ability to detect mural calcifications within the neoplasm (15). The optimal treatment of any adenocarcinoma of the appendix is right hemicolectomy, either as a primary operation or as a secondary operation after adenocarcinoma of the appendix is noted on microscopic exam (11). When appendiceal mucocele is suspected controversy surrounds the topic of open versus laparoscopic appendectomy (16). Gonzales et al. (17) reported dissemination of the mucocele after laparoscopic approach suggesting open appendectomy as the procedure of choice. Rupture of an appendiceal mucocele can result in dissemination of the epithelial cells into the peritoneal cavity and incite pseudomyxoma peritonei a catastrophic complication (18). Care must be taken regardless of the approach when handling this neoplasm. Patients with appendiceal adenocarcinomas have a significant risk of synchronous and metachronous neoplasm, which often originate from the gastrointestinal tract (4).
Grading of appendiceal adenocarcinoma is the same as in the large intestines. Similar to the colon an adenoma-carcinoma sequence is assumed to occur in the appendix (19). In our patient there was no sign of adenoma and the adenocarcinoma was thought to be de nova. In comparison with colonic adenomas, adenomas of the appendix are more like to be serrated or villous (20). Staging for appendiceal adenocarcinoma uses the tumor-node-metastasis classification similar to colonic adenocarcinoma, however should be viewed differently secondary to the unique nature of appendiceal pseudomyxoma peritonei (M1/stage 4) in which malignant cells maybe noninvasive eluding to a worse prognosis than the same staged colonic induced pseudomyxoma peritonei that carries a worse prognosis (20). Misdraji et al. found patients with low-grade neoplasms confined to the appendix had a 100% survival at a median survival time of 6 years. Those with extra-appendiceal spread had a survival at 86% at 5 years. Those diagnosed with mucinous adenocarcinomas had a 5-year survival of 44% (21). SEER data 5-year survival for localized adenocarcinoma was 95%, and 80% in mucinous or cystadenocarcinomas (9). Right hemicolectomy with appropriate adjuvant therapy is recommended for both mucinous and nonmucinous carcinomas (21).
Conclusions
Mucinous adenocarcinoma of the appendix is a rare entity that in most cases is found incidentally. It is estimated that general surgeons may only see one or two cases of adult intussusception during their career (7). When intussusception is found in an adult a clinician should have malignancy high on their differential. We would like to impress the importance of pursuing the underlying etiology behind intussusception so appropriate treatment may be given prior to a malignancy becoming inoperable or untreatable if not diagnosed on initial presentation.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Begos DG, Sandor A, Modlin IM. The diagnosis and management of adult intussusception. Am J Surg 1997;173:88-94. [PubMed]
- Alexander R, Traverso P, Bolorunduro OB, et al. Profiling adult intussusception patients: comparing colonic versus enteric intussusception. Am J Surg 2011;202:487-91. [PubMed]
- Takahashi M, Sawada T, Fukuda T, et al. Complete appendiceal intussusception induced by primary appendiceal adenocarcinoma in tubular adenoma: a case report. Jpn J Clin Oncol 2003;33:413-5. [PubMed]
- Jevon GP, Daya D, Qizilbash AH. Intussusception of the appendix. A report of four cases and review of the literature. Arch Pathol Lab Med 1992;116:960-4. [PubMed]
- Guerra VJ, Lee BY. Intussusception in Adults. Contemporary Surg for Residents 1994;2:7-11.
- Chetty R, Daniel WJ. Mucinous cystadenoma of the appendix: an unusual cause of recurrent intussusception in an adult. Aust N Z J Surg 1992;62:670-1. [PubMed]
- McCusker ME, Coté TR, Clegg LX, et al. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer 2002;94:3307-12. [PubMed]
- Marinis A, Yiallourou A, Samanides L, et al. Intussusception of the bowel in adults: a review. World J Gastroenterol 2009;15:407-11. [PubMed]
- Thomas RM, Sobin LH. Gastrointestinal cancer. Cancer 1995;75:154-70. [PubMed]
- Modlin IM, Sandor A. An analysis of 8305 cases of carcinoid tumors. Cancer 1997;79:813-29. [PubMed]
- Ben-David K, Sarosi Jr G. “Appendicitis,” in Seisenger & Fordtran’s Gastrointestinal and Liver Disease. Feldman M, Friedman LS, Brandt L, pp.2069-2070, Saunders, Philadelphia, Pa, USA, 9th edition, 2010.
- McCusker ME, Coté TR, Clegg LX, et al. Primary malignant neoplasms of the appendix: a population-based study from the surveillance, epidemiology and end-results program, 1973-1998. Cancer 2002;94:3307-12. [PubMed]
- Connor SJ, Hanna GB, Frizelle FA. Appendiceal tumors: retrospective clinicopathologic analysis of appendiceal tumors from 7,970 appendectomies. Dis Colon Rectum 1998;41:75-80. [PubMed]
- Pickhardt PJ, Levy AD, Rohrmann CA Jr, et al. Primary neoplasms of the appendix manifesting as acute appendicitis: CT findings with pathologic comparison. Radiology 2002;224:775-81. [PubMed]
- Krieg A, Esch JS 2nd, Poll LW, et al. Mucinous cystadenoma of the appendix misdiagnosed as cystic hydatid disease of the liver: a case report. J Med Case Rep 2008;2:218. [PubMed]
- Palanivelu C, Rangarajan M, John SJ, et al. Laparoscopic right hemicolectomy for mucocele due to a low-grade appendiceal mucinous neoplasm. JSLS 2008;12:194-7. [PubMed]
- González Moreno S, Shmookler BM, Sugarbaker PH. Appendiceal mucocele. Contraindication to laparoscopic appendectomy. Surg Endosc 1998;12:1177-9. [PubMed]
- Liberale G, Lemaitre P, Noterman D, et al. How should we treat mucinous appendiceal neoplasm? By laparoscopy or laparotomy? A case report. Acta Chir Belg 2010;110:203-7. [PubMed]
- Qizilbash AH. Mucoceles of the appendix. Their relationship to hyperplastic polyps, mucinous cystadenomas, and cystadenocarcinomas. Arch Pathol 1975;99:548-55. [PubMed]
- Carr NJ, McCarthy WF, Sobin LH. Epithelial noncarcinoid tumors and tumor-like lesions of the appendix. A clinicopathologic study of 184 patients with a multivariate analysis of prognostic factors. Cancer 1995;76:757-68. [PubMed]
- Misdraji J, Yantiss RK, Graeme-Cook FM, et al. Appendiceal mucinous neoplasms: a clinicopathologic analysis of 107 cases. Am J Surg Pathol 2003;27:1089-103. [PubMed]