Palliative radiotherapy for hepatobiliary obstruction caused by colorectal metastases
Introduction
Liver metastases from colorectal cancer can lead to biliary obstruction, and in certain cases, hyperbilirubinemia may persist even after appropriate biliary stenting. While palliative radiotherapy (RT) is a treatment option for these patients, its efficacy in relieving hyperbilirubinemia that is not responsive to biliary stenting is not well-established in the literature. Here, we describe a patient with metastatic colorectal cancer with severe hyperbilirubinemia, unrelieved by biliary stent but successfully relieved with palliative RT.
Case presentation
A 75-year-old woman was referred to the radiation oncology department in November 2018 for progressive colorectal metastases in segment 5 of the liver with persistent biliary obstruction despite appropriate stent placement. The patient was initially diagnosed in 2011 with Stage III rectal adenocarcinoma. She was treated with resection plus adjuvant pelvic chemoradiation followed by FOLFOX alone. In 2015, surveillance imaging revealed new hepatic lesions, which were subsequently biopsy-confirmed as rectal adenocarcinoma metastases.
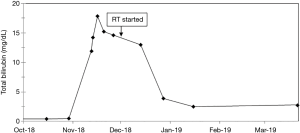
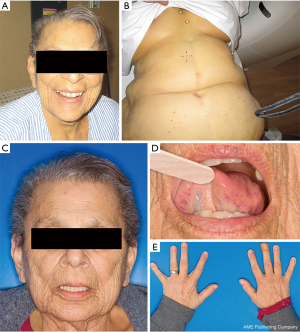
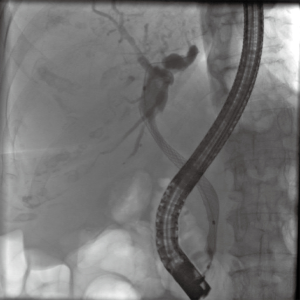
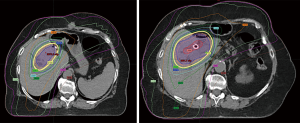
The patient was treated with FOLFIRI and bevacizumab and underwent a left hepatectomy, cholecystectomy, and partial hepatectomy of segment 5 of the liver. Subsequent CT imaging revealed no evidence of disease. However, in 2016, the patient’s metastatic disease progressed with new hepatic metastases. She underwent multiple rounds of chemotherapy, including FOLFIRI plus bevacizumab, then FOLFOX and bevacizumab, and subsequently cetuximab. In November 2018 her total bilirubin rose to 11.9 mg/dL. An abdominal CT without contrast showed new biliary dilatation, and the patient underwent an endoscopic retrograde cholangiopancreatogram (ERCP) with stent placement (Figure 1). One uncovered, self-expanding, metallic stent was placed into the common hepatic duct, and bile flowed through the stent at the time of placement. Intra-procedural imaging was used to verify stent placement and position, and follow-up CT abdomen showed decompressed central bile ducts. Shortly following the stent placement, total bilirubin continued to rise to 17.8 mg/dL (Figure 2). Limitation in the ERCP-directed stenting was attributed to existing portal caval lymphadenopathy. Prior to RT, the patient experienced fatigue, diarrhea, nausea, vomiting, and severe jaundice (Figure 3). After a multidisciplinary discussion, the patient commenced palliative RT, in an attempt to relieve her biliary obstructive symptoms clinically. The patient received 37.5 Gy in 15 fractions (once daily) to the tumor surrounding the right hepatic bile duct, with microscopic and setup margins around the gross tumor volume (Figure 4). She previously had not received any liver-directed radiotherapy before. At the end of RT, the patient’s total bilirubin decreased to 3.9 mg/dL (Figure 2). Her symptoms including jaundice and pruritus had resolved (Figure 3). She tolerated RT without significant treatment-related toxicities.
One month following RT, the patient’s total bilirubin further improved to 2.5 mg/dL. Two months following RT, she was hospitalized at an outside institution for sepsis. At the onset of sepsis, total bilirubin remained at 2.5 mg/dL and was not clinically considered to be related to the septic event. At last clinical follow-up being three months following RT, total bilirubin was 2.8 mg/dL, and the patient pursued hospice care and died from her underlying extrahepatic disease shortly thereafter. At the time of her death, she remained symptom-free from hepatobiliary obstruction.
Discussion
The liver is the most frequent site for distant metastases from lung, breast, and colorectal cancers. Liver metastases occur in more than 50% of colorectal cancer patients and result in death in about two thirds of this population (1,2). Hepatic tumor burden may lead to severe hyperbilirubinemia and intrahepatic bile duct obstruction. Biliary decompression can be difficult in many cases. For patients with persistent jaundice who do not obtain adequate symptomatic relief even with appropriate stent placement in the context of liver metastases, palliative RT may be effective for reducing symptoms as an additional treatment.
In metastatic colorectal cancer, the onset of jaundice is associated with very poor median survival of 1.5 months (3). Physiologically, severe jaundice is incompatible with life, and often precludes further treatment such as meaningful systemic therapy administration. Successful biliary drainage has been shown to be a significant prognostic factor in malignant obstructive jaundice (4,5). Unfortunately, attempts at relieving jaundice in the setting of metastatic colorectal cancer are often ineffective, with less than one fifth of patients being able to receive further chemotherapy (3).
Various palliative treatments are available to relieve malignant biliary obstruction including stent placement during an ERCP. However, biliary obstruction may persist due to various factors, such as biliary sludge formation, tumor ingrowth/overgrowth, or stent migration/obstruction. Another palliative treatment is percutaneous transhepatic biliary drainage (PTBD) with self-expandable stents, but many patients experience recurrent jaundice and cholangitis. Surgery is another palliative approach that can result in long-term patency but has high rates of morbidity and postoperative mortality (6). Additionally, most of these patients are near end of life and do not have the physiologic reserve to be surgical candidates; furthermore, they may not desire aggressive interventions. In cases with inoperable biliary obstruction or debilitated patients who cannot withstand further systemic therapies due to severe hyperbilirubinemia, RT is an alternative and often suitable treatment option which is currently underutilized in radiation oncology clinics.
RT has demonstrated efficacy in relieving jaundice from biliary cancers. Ohnishi et al. (7) demonstrated that 50–60 Gy of conventionally fractionated external beam RT and PTBD improved serum total bilirubin levels to normal in 10 (91%) of 11 patients with obstructive jaundice secondary to hilar cholangiocarcinoma (Table 1). Kuvshinoff et al. (8) showed that jaundice was relieved in 10 (83%) of 12 patients with unresectable hilar cholangiocarcinoma treated with internal biliary drainage in conjunction with RT (Table 1). In highly selected patients, RT may have a role in prolonging survivals; patients with unresectable bile duct tumors who received intraluminal therapy with external beam RT had a median survival of 6.5 months, while patients who received intraluminal therapy alone had a median survival of 4.5 months (Table 1) (9). In a more recent study (11), patients with hilar cholangiocarcinoma who received external beam RT and intraluminal therapy had an overall survival of 22.1 months, compared with patients who received best supportive care alone (5.7 months). Finally, RT has also been shown to increase stent patency in patients with inoperable biliary cancers, when compared to patients receiving best supportive care only (12).
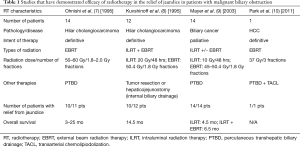
Full table
Hepatobiliary obstruction caused by liver metastases is challenging from a surgical perspective. Moreover, drainage by interventional radiology-guided procedures may be difficult (13). In addition, such treatments may become ineffective for patients with multiple sites of biliary obstruction or diffusely metastatic diseases within the liver. In this case study, we demonstrated that palliative RT can be a successful treatment option for stent-intolerant biliary obstruction, and our patient obtained significant and complete symptomatic relief which happened shortly during and after her completion of RT. Clinically, patency and force of the self-expanding stent as applied radially may have also contributed to further decrease of the patient’s bilirubin level one month following RT. Further studies are needed to evaluate the efficacy of RT for palliating biliary obstruction for liver metastases, an often challenging scenario that deserves our attention clinically.
Acknowledgments
None.
Footnote
Conflicts of Interest: Terence T. Sio provides strategic and scientific recommendations as a member of the Advisory Board and speaker for Novocure, Inc., which is not in any way associated with the content or disease site as presented in this manuscript. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Tomlinson JS, Jarnagin WR, DeMatteo RP, et al. Actual 10-Year Survival After Resection of Colorectal Liver Metastases Defines Cure. J Clin Oncol 2007;25:4575-80. [Crossref] [PubMed]
- House MG, Kemeny NE, Gönen M, et al. Comparison of Adjuvant Systemic Chemotherapy With or Without Hepatic Arterial Infusional Chemotherapy After Hepatic Resection for Metastatic Colorectal Cancer. Ann Surg 2011;254:851-6. [Crossref] [PubMed]
- Nichols SD, Albert S, Shirley L, et al. Outcomes in patients with obstructive jaundice from metastatic colorectal cancer and implications for management. J Gastrointest Surg 2014;18:2186-91. [Crossref] [PubMed]
- Kurniawan J, Hasan I, Gani RA, et al. Mortality-related Factors in Patients with Malignant Obstructive Jaundice. Acta Med Indones 2016;48:282-8. [PubMed]
- Suh YG, Kim DY, Han KH, et al. Effective biliary drainage and proper treatment improve outcomes of hepatocellular carcinoma with obstructive jaundice. Gut Liver 2014;8:526-35. [Crossref] [PubMed]
- Giovannini M, Dotti M, Bories E, et al. Hepaticogastrostomy by Echo-Endoscopy as a Palliative Treatment in a Patient with Metastatic Biliary Obstruction. Endoscopy 2003;35:1076-8. [Crossref] [PubMed]
- Ohnishi H, Asada M, Shichijo Y, et al. External radiotherapy for biliary decompression of hilar cholangiocarcinoma. Hepatogastroenterology 1995;42:265-8. [PubMed]
- Kuvshinoff BW, Armstrong JG, Fong Y, et al. Palliation of irresectable hilar cholangiocarcinoma with biliary drainage and radiotherapy. Br J Surg 1995;82:1522-5. [Crossref] [PubMed]
- Mayer R, Stranzl H, Prettenhofer U, et al. Palliative treatment of unresectable bile duct tumours. Acta Med Austriaca 2003;30:10-2. [Crossref] [PubMed]
- Park CK, Bae SH, Yang HJ, et al. Successful treatment of stereotactic body radiation therapy combined with transarterial chemolipiodolization for hepatocellular carcinoma with biliary obstruction. Korean J Intern Med 2011;26:94-8. [Crossref] [PubMed]
- Isayama H, Tsujino T, Nakai Y, et al. Clinical benefit of radiation therapy and metallic stenting for unresectable hilar cholangiocarcinoma. World J Gastroenterol 2012;18:2364-70. [Crossref] [PubMed]
- Johnson DW, Safai C, Goffinet DR. Malignant obstructive jaundice: Treatment with external-beam and intracavitary radiotherapy. Int J Radiat Oncol Biol Phys 1985;11:411-6. [Crossref] [PubMed]
- Liu F, Zhang CQ, Wang GC, et al. Percutaneous Biliary Stent Placement in Palliation of Malignant Bile Duct Obstruction. Gastroenterology Res 2009;2:289-94. [PubMed]