
Colon cancer laterality is associated with atherosclerosis and coronary artery disease
Introduction
Cardiovascular disease (CAD) is the leading cause of death in the United States accounting for 836,546 deaths annually, and 92.1 million adults are currently living with the disease (1). Despite a decline in mortality due to coronary heart disease over the last 10 years in US, coronary heart disease remains a source of high morbidity and mortality with $329.7 billion in health care expenditures (1). Malignancy is the second leading cause of death, with colon cancer being the third cause of malignancy-related deaths. There were an estimated 95,520 new cases of colon cancer in 2017 in the United States (2). There has been increasing evidence of an association between cardiovascular disease and cancer, which is based on shared pathophysiology of inflammation promoting both atherosclerosis and carcinogenesis (3,4). Both malignancy and coronary heart disease share common risk factors such as obesity, hyperglycemia, hypertension, tobacco use, hyperlipidemia (5), and cancer survivors have an overall higher incidence of cardiovascular disease compared to patients without cancer (6). In addition, patients diagnosed with CAD have a higher prevalence of colorectal neoplasms compared to patients without CAD (7-9). Extensive studies have shown that compared to left-sided colon cancer (LCC), those with right-sided colon cancer (RCC) have lower overall survival (10). However, the exact cause or biomechanistic rationale for this difference is yet to be understood. There have not been prior studies evaluating the association between cardiovascular disease and atherosclerosis burden with colon cancer laterality. The goal of the present study was to compare the prevalence of CAD and distribution of coronary and vascular calcific atherosclerosis between patients with RCC and LCC.
Methods
This is a single-center retrospective cross-sectional study of consecutive patients diagnosed with colon cancer at Albany Medical Center between January 2005 and December 2014. The study was reviewed and approved by Institutional Review Board. Overall, 583 patients met the following inclusion criteria: (I) primary diagnosis of colon cancer; (II) primary cancer involvement from cecum to sigmoid colon; (III) patients followed at Albany Medical Center or New York Hematology-Oncology PC for care. Initial patient data was obtained from the Institutional Cancer Registry. Patients with unavailable or incomplete medical records were excluded (n=37). As a result, a total 546 patients were included in the study, of which 261 patients were found to have RCC and 285 patients were found to have LCC.
Demographic characteristics were collected including age at the time of cancer diagnosis, ethnicity, and gender. Medical comorbidities were recorded including: hypertension, diabetes mellitus, hyperlipidemia, history of myocardial infarction, history of percutaneous coronary intervention (PCI) and coronary artery bypass grafting (CABG), hypothyroidism, congestive heart failure, chronic kidney disease, atrial fibrillation, and current or prior smoking and alcohol use histories. Clinical CAD was defined as patients who had prior documented CAD in their medical history, myocardial infarction, and/or PCI or CABG. Cancer characteristics that were collected included stage at the time of initial diagnosis and laterality, which was determined based on operative and/or colonoscopy report. RCC was defined as the cecum, ascending, and transverse colon, whereas the descending and sigmoid colon were defined as LCC (11).
Computed tomography (CT) imaging of the chest, abdomen, and pelvis was obtained for staging within 1 year before or after initial cancer diagnosis in 486 patients. Two radiology residents reviewed the CT scans for the presence of atherosclerotic calcifications in the coronary arteries, thoracic aorta, and abdominal aorta. These findings were confirmed by a board-certified cardiothoracic radiologist with nine years post-fellowship experience. A novel semi-quantitative scoring system was designed for grading the extent of calcifications. The extent of calcifications was categorized based on the number of vascular territories affected, ranging from 0 (no calcifications) to 3 (presence of calcifications in the coronary, thoracic, and abdominal aorta).
Quantitative statistics were used to compare differences between RCC and LCC. Continuous variables such as age are expressed as mean ± standard deviation, and compared with two-tailed student’s t-test. Categorical variables are expressed as percentages and compared with Chi-square test. To assess the association between clinical CAD and laterality, we used univariate and multivariate Poisson regression models to calculate relative risk ratio with 95% confidence interval. Model covariates included common CAD risk factors and factors that were significantly different between the groups (age, sex, current and history of smoking, hypertension, diabetes mellitus, hyperlipidemia and hypothyroidism). Additional analysis performed with Kaplan-Meyer method comparing survival between right and left sided CRC. All statistical analyses were performed using Stata software, version 14.0 (Stata Corp). A two-tailed P of 0.05 was considered as statistically significant.
Results
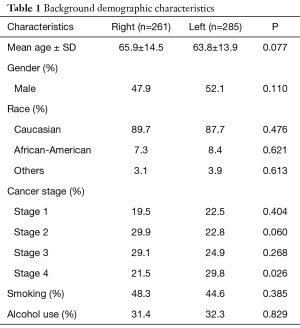
Of the 546 patients, 261 (47.8%) had RCC and 285 (52.2%) had LCC. The baseline characteristics including age, gender, ethnicity, and cancer staging were similar between the two groups (Table 1). Most of the patients were males (51.5%), Caucasian (88.6%), and the mean age was 64.8±14.2 years. The prevalence of modifiable risk factors including tobacco use (current and former) and alcohol use were also similar between the 2 groups and were not statistically significant. Overall, 21.1% had stage 1 colon cancer, 26.2% had stage 2, 26.9% had stage 3, and 25.8% had stage 4. Distribution by colon cancer stages was similar between both groups, except for stage 4, which was more prevalent in patients with LCC.
Full table
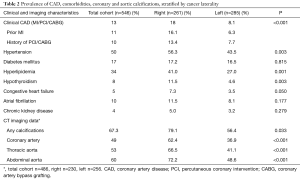
As shown in Table 2, a diagnosis of hypertension was present in 50% of patients, hyperlipidemia in 34% and clinical CAD in 13% of total cohort. Compared to patients with LCC, those with RCC had a higher prevalence of hypertension, hyperlipidemia, history of myocardial infarction, prior revascularization with percutaneous coronary intervention and/or CABG, and hypothyroidism. Similarly, clinical CAD was significantly more prevalent in patients with RCC than LCC. The prevalence of other comorbidities including congestive heart failure, diabetes mellitus, chronic kidney disease, and atrial fibrillation was not statistically significantly different between the two groups, although there were trends for a higher prevalence of each these conditions in patients with RCC (Table 2).
Full table
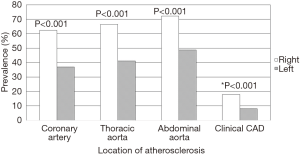
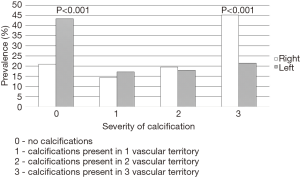
Among the 486 patients who had CT scans performed and available for review, vascular calcifications were present in 67.3% of all patients with colon cancer (79.1% of patients with RCC and 56.4% in LCC). Patients with RCC had higher prevalence of coronary, thoracic, and abdominal aortic calcifications, as shown in Table 2 and Figure 1. Calcification severity scoring demonstrated that patients with RCC tended to have more widespread calcification (score 3), while LCC patients had higher prevalence of less extensive calcification or no disease (score 1 or 0). Statistically significant differences were noted for patients with no disease (score 0) and severe disease (score 3) (Figure 2).
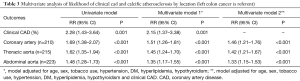
As depicted in Table 3, regression analysis demonstrated that patients with RCC were more likely to have clinical CAD and calcifications in coronary arteries, thoracic aorta, and abdominal aorta by both univariate and multivariate analysis. Furthermore, RCC was associated with a higher likelihood of calcific atherosclerosis in each individual territory, even after adjusting for the prevalence of clinical CAD (Table 3). Overall mortality rate for the total cohort was 0.07 (95% CI, 0.048–0.093) at 6 months, 0.12 (95% CI, 0.092–0.147) at 12 months, 0.18 (95% CI, 0.150–0.216) at 24 months, and 0.24 (95% CI, 0.208–0.281) at 36 months. Kaplan-Meier analysis of survival between RCC and LCC was not significantly different with hazard ratio (HR) of 0.982 (95% CI, 0.740–2.304, P=0.901).
Full table
Discussion
We observed a higher prevalence of clinical CAD and cardiovascular risk factors in patients with RCC compared with LCC. We also found that approximately two thirds of the overall cohort had calcific atherosclerosis, and that RCC was associated with a higher burden of calcific atherosclerosis in the coronaries and aorta compared with LCC. After adjusting for covariates, we observed that RCC was an independent predictor of clinical CAD and coronary and aortic calcifications. These observations highlight the importance of early identification and treatment with primary or secondary prevention strategies including lifestyle modifications for cardiovascular conditions in patients with colon cancer, especially in patients with right-sided colon cancer.
Several studies have reported increased prevalence of colorectal neoplasms among patients with ischemic heart disease diagnosed by invasive coronary angiography or coronary CT angiography (7,12-14). Additionally, even in asymptomatic patients, colorectal adenoma has been found to be associated with coronary artery calcification in a severity dependent manner (8,9). The prevalence of clinical CAD in our cohort of patients with colon cancer was 13.0%, which is also similar to the prevalence reported by Fu et al., which was 13.5% (15). In their retrospective study of patients (n=12,648) from two US based medical and pharmacy databases, Fu et al. reported cardiovascular diseases are found to be the most common among patients with metastatic colorectal cancer. In addition, they reported a prevalence of hypertension of 49.7% and heart failure of 7.2%, which was similar to that observed in our cohort. These observations underscore potential common etiologic factors for development of CAD and colorectal cancer. For example, hyperlipidemia is a risk factor common to both cardiovascular disease and colon cancer, and high cholesterol known to promote colon carcinogenesis (16).
To our knowledge there are no prior studies specifically focusing on the association between colon cancer laterality and cardiovascular disease. It has been observed that patients with RCC have increased number of comorbidities, advanced cancer stages, more commonly large and poorly differentiated tumors, and overall poorer prognosis than LCC patients (10). In a recent meta-analysis of 15 studies conducted from 1971 to 2013 (n=108,474), observed that RCC has worse overall survival than LCC (17). The exact mechanism underlying this mortality difference is still not well understood. One potential theory suggests that different pathophysiologic processes are involved in the development of right versus left sided colon cancer, which may contribute to the differences in outcomes (18). RCC has more microsatellite instability 20% compared to LCC in 1% (19). While microsatellite instability has better prognosis, however, it has been proposed that RCC present at later stages, countering this initial benefit (20). Overall it appears that RCC presents with systemic symptoms compared to localized symptoms of LCC. In our cohort, patients with RCC had a higher likelihood of clinical CAD and calcific coronary and vascular atherosclerosis. In addition, the prevalence of common cardiovascular disease risk factors, such as tobacco use, hypertension and dyslipidemia was significantly higher in RCC patients as well. These findings raise the possibility that there are common etiologic factors for CVD and RCC. However, we cannot infer that increased prevalence of CV disease and calcific atherosclerosis could contribute to the higher mortality of RCC. These observations deserve further study in larger multi-center cohorts and prospective studies to further delineate the causes of increased mortality and assess relationship between CV disease and mortality in these populations.
The nascent field of cardio-oncology has come to focus on both preventive and treatment modalities to reduce cardiovascular morbidity and mortality in cancer patients. It has been reported that cardiovascular disease is under-recognized in patients with colon cancer, which could contribute to increased mortality (21). Early identification and vigilant management of cardiovascular disease and its risk factors based on primary tumor location could theoretically reduce cardiovascular-related morbidity and mortality in colon cancer patients. As the prevalence of coronary calcification was 62% in patients with RCC, potential screening with calcium scoring could be especially useful in this group. This screening strategy deserves further investigation, and ideally in prospective randomized clinical trials.
Our study has several limitations. First, the retrospective cross-sectional design limits the ability to determine the development and progression of atherosclerosis as well as the prognosis of patients with colon cancer. Second, while we observed an independent association between clinical CAD and right sided colon cancer, we cannot determine the nature of the relationship nor make informed suggestions for treatment. However, our findings were robust and consistent across subgroups after using multivariate analysis to adjust for confounding factors. Third, not all patients had CT scans available for analysis, although the reduction in sample should bias results towards the null. Fourth, variations in dietary habit, waist circumference, and cholesterol metabolism among individual patients are difficult to control and assess especially in retrospective study. Finally in some studies, RCC is found in older cohorts and thus there is concern for delayed diagnosis accounting for greater prevalence of CAD. However, in our cohort, the mean ages in RCC and LCC groups were similar without statistical significance, and thus delayed diagnosis is unlikely to be contributing to the current results.
In conclusion, we found that both vascular calcifications and clinical CAD including history of myocardial infarction and PCI or CABG are prevalent in patients with colon cancer, and are independently increased in patients with RCC compared to LCC. RCC is similarly independently associated with a higher burden of calcific atherosclerosis. Further studies are needed to identify mechanism for this phenomenon. Patients with colon cancer, especially right-sided, may benefit from earlier identification and treatment of cardiovascular disease including coronary artery disease and risk factors leading to myocardial infarction and cardiovascular mortality.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Albany Medical Center Committee on Research Involving Human Subjects Institutional Review Board (No. 4870) and all consent requirement was met based on the institutional policy for retrospective study.
References
- Benjamin EJ, Virani SS, Callaway CW, et al. Heart Disease and Stroke Statistics-2018 Update: A Report From the American Heart Association. Circulation 2018;137:e67-492. [Crossref] [PubMed]
- American Cancer Society. Cancer Facts and Figures 2017. American Cancer Society. Available online: https://www.cancer.org/research/cancer-facts-statistics/all-cancer-facts-figures/cancer-facts-figures-2017.html
- Barrera G, Pizzimenti S, Dianzani MU. Lipid peroxidation: control of cell proliferation, cell differentiation and cell death. Mol Aspects Med 2008;29:1-8. [Crossref] [PubMed]
- Thanan R, Oikawa S, Hiraku Y, et al. Oxidative stress and its significant roles in neurodegenerative diseases and cancer. Int J Mol Sci 2014;16:193-217. [Crossref] [PubMed]
- Kamp DW, Shacter E, Weitzman SA. Chronic inflammation and cancer: the role of the mitochondria. Oncology (Williston Park) 2011;25:400-10, 413. [PubMed]
- Armenian SH, Xu L, Ky B, et al. Cardiovascular Disease Among Survivors of Adult-Onset Cancer: A Community-Based Retrospective Cohort Study. J Clin Oncol 2016;34:1122-30. [Crossref] [PubMed]
- Chan AO, Jim MH, Lam KF, et al. Prevalence of colorectal neoplasm among patients with newly diagnosed coronary artery disease. JAMA 2007;298:1412-9. [Crossref] [PubMed]
- Yang MH, Cho J, Choi YH, et al. The association between coronary artery calcification and colorectal adenoma. Hepatogastroenterology 2013;60:538-42. [PubMed]
- Choi SH, Kang HY, Choi SY, et al. Colorectal adenoma is associated with coronary artery calcification in a Korean population. Atherosclerosis 2015;242:515-20. [Crossref] [PubMed]
- Hansen IO, Jess P. Possible better long-term survival in left versus right-sided colon cancer - a systematic review. Dan Med J 2012;59:A4444. [PubMed]
- Meguid RA, Slidell MB, Wolfgang CL, et al. Is there a difference in survival between right- versus left-sided colon cancers? Ann Surg Oncol 2008;15:2388-94. [Crossref] [PubMed]
- Hee YJ, Bang CS, Baik GH, et al. Association between ischemic heart disease and colorectal neoplasm: a systematic review and meta-analysis. Springerplus. 2016;5:1664. [Crossref] [PubMed]
- Yang SY, Kim YS, Chung SJ, et al. Association between colorectal adenoma and coronary atherosclerosis detected by CT coronary angiography in Korean men; a cross-sectional study. J Gastroenterol Hepatol 2010;25:1795-9. [Crossref] [PubMed]
- Yang XB, Xu QL, Xu CY, et al. Prevalence of colorectal neoplasm in Chinese patients with high-risk coronary artery disease classified by the Asia-Pacific Colorectal Screening score. J Dig Dis 2015;16:272-8. [Crossref] [PubMed]
- Fu AZ, Zhao Z, Gao S, et al. Comorbid Conditions in Patients With Metastatic Colorectal Cancer. World J Oncol 2011;2:225-31. [PubMed]
- Tseng TH, Hsu JD, Chu CY, et al. Promotion of colon carcinogenesis through increasing lipid peroxidation induced in rats by a high cholesterol diet. Cancer Lett 1996;100:81-7. [Crossref] [PubMed]
- Yahagi M, Okabayashi K, Hasegawa H, et al. The Worse Prognosis of Right-Sided Compared with Left-Sided Colon Cancers: a Systematic Review and Meta-analysis. J Gastrointest Surg 2016;20:648-55. [Crossref] [PubMed]
- Richman S, Adlard J. Left and right sided large bowel cancer. BMJ 2002;324:931-2. [Crossref] [PubMed]
- Elsaleh H, Joseph D, Grieu F, et al. Association of tumour site and sex with survival benefit from adjuvant chemotherapy in colorectal cancer. Lancet 2000;355:1745-50. [Crossref] [PubMed]
- Wright CM, Dent OF, Barker M, et al. Prognostic significance of extensive microsatellite instability in sporadic clinicopathological stage C colorectal cancer. Br J Surg 2000;87:1197-202. [Crossref] [PubMed]
- Lim DR, Kuk JK, Kim T, et al. Comparison of oncological outcomes of right-sided colon cancer versus left-sided colon cancer after curative resection: Which side is better outcome? Medicine (Baltimore) 2017;96:e8241. [Crossref] [PubMed]


