
Comparison of 3D printing model to 3D virtual reconstruction and 2D imaging for the clinical education of interns in hepatocellular carcinoma: a randomized controlled study
Highlight box
Key findings
• 3D printing technology not only improves interns’ comprehensive ability in hepatic anatomy and understanding of the spatial relationships among anatomical structures but also increases their clinical thinking ability and interest.
What is known and what is new?
• In traditional teaching methods, lecture-based learning and two-dimensional (2D) images such as computed tomography (CT) or magnetic resonance imaging (MRI) are usually utilized to explain the anatomical structures of the liver and tumor.
• Patient-specific 3D printing liver models were used in HCC clinical education in addition to lecture-based learning
What are the implications, and what should change now?
• Traditional teaching methods are boring and ineffective, while teaching based on a 3D printing model is vivid, which can improve interns' learning interest and understanding ability.
Introduction
Hepatocellular carcinoma (HCC) is the 4th most common malignant tumor and the 2nd highest cause of cancer-related mortality in China (1). It is particularly prevalent and has a very poor prognosis, with a morbidity-to-mortality ratio of 1:0.9 and a 5-year survival rate of 12.1%, which seriously threatens the life and health of Chinese people (2,3). The general office of the state council of China proposed that the “priority of healthcare must be given to the development of medical education and talent training” (4). The training of hepatobiliary students is a long process. Mastering the hepatic anatomy and determining the location of lesions and their relationship with the surrounding ducts before surgery is crucial for the surgical treatment of HCC. However, the liver is a solid and opaque organ separated into eight segments, known as Couinaud segments, with a dense and intricate distribution of blood vessels and bile ducts.
In traditional teaching methods, lecture-based learning and two-dimensional (2D) images such as computed tomography (CT) or magnetic resonance imaging (MRI) are usually used to explain the anatomical structures of the liver and tumor. It is often difficult for interns to visualize 2D images as 3D spatial concepts and comprehensively understand their anatomical characteristics, which is the difficulty and a key point in the clinical education on HCC. Previous studies suggest that a 3D printing model (3DPM) of HCC may be more informative than 3D virtual reconstruction (3DVR) and multi-detector computed tomography (MDCT) (5,6). 3DPM can realistically display the details of internal organs and tissue structures, and surgeons can observe and manipulate specific anatomical structures in advance. This kind of education and training obviously has many benefits, including increasing anatomical understanding ability, shortening operation time and predicting intraoperative complications (7). 3D printing technology has been widely used in orthopedics and plastic surgery for whether medical education or surgical planning, and gained remarkable efficacy compared to conventional approaches (8). However, due to the complex intrahepatic anatomy as well as high price and prolonged time for accomplishing a specific 3DPM of liver, which was seldom reported in the application of medical teaching. The value of 3D printing technology in medical inters’ clinical education of HCC is uncertain, and relevant literatures are very few. This study aimed to explore the effects of 3DPM on the clinical education of HCC. We present the following article in accordance with the CONSORT reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/rc).
Methods
Subjects
This single-center randomized trial comprised new interns studied in department of Hepatobiliary & Pancreatic Surgery and Minimally Invasive Surgery, Zhejiang Provincial People’s Hospital (Affiliated People’s Hospital, Hangzhou Medical College). This three-parallel study was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital (No. 2021QT333). Informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). Three laparoscopic hepatectomies were collected (Table 1). For each case, 3DVR and 3DPM models would be created from MDCT data, respectively (Figure 1). To be eligible to participate in this study, interns had to meet the following inclusion criteria: all the students completed the courses of hepatic anatomy, diagnosis and treatment of HCC; all the groups of interns were taught by the experienced senior teachers, and the teaching time and cases were the same. Participants who were disobedient to management or had casual learning attitude were excluded from the study.
Table 1
| Case | Diagnosis | Tumor location | Surgical procedure |
|---|---|---|---|
| 1 | HCC | Segment 5, 6, 7, 8 | Lap. right hepatectomy |
| 2 | HCC | Segment 6, 7 | Lap. right posterior lobectomy |
| 3 | HCC | Segment 4,5, 8 | Lap. mesohepatectomy |
HCC, hepatocellular carcinoma; Lap., laparoscopic.
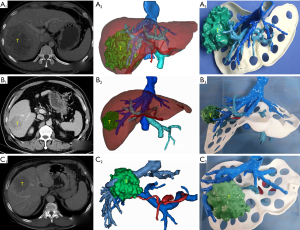
3DPM production process
The 3D printing process was conducted as follows: first, the MDCT data was collected for 3D reconstruction using modeling software (Central and southern E3D digital medical and virtual software V17.06, China). Second, the specific information including location of lesion and its surrounding ducts were analyzed by the open-source slicing software (Ulitmaker Cura 4.4.1, USA), which generated G code. Third, SLA (Stereo Lithography Appearance) (SL600, ZhongRuiZhiChuang3D technology co., LTD., China) identified the code and printed a corresponding hepatic model. The model material was composed of photosensitive resin with fracture elongation rate of 10-15% and bending strength of 66–73 MPa. This material was previously placed in a cylinder after deaeration, solidified and then printed layer-by-layer using the ultraviolet control system (ZhongruiZhichuang3D Technology Co., LTD., China). Only the lesions with ducts (diameter >2 mm) including vessels and bile ducts were printed without the remaining hepatic parenchyma printed. The surface of 3DPM was designed with a hollow-out design using approximately 50 mm diameter apertures. A freshly printed model was cured by ultraviolet mercury lamp (ZhongruiZhichuang 3D Technology Co., LTD., China) and then dyed in a post-processing box. A specific 3DPM was accomplished ultimately (Figure 1).
Randomization and intervention
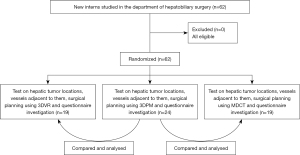
A total of 62 new interns who studied in the department of hepatobiliary surgery were invited to participate in this study and were randomly assigned to each group (3DPM, 3DVR, and MDCT groups) through a table of random numbers for random grouping. In this three-parallel study, 24 interns were allocated to the 3DPM group, 19 interns were allocated to the 3DVR group, and the rest 19 medical interns to the MDCT group (Figure 2). The allocation ratio of 3DPM group to the 3DVR and MDCT group was 1.3:1:1. After lecture-based learning by experienced senior teachers in identical time, including liver anatomy as well as diagnosis and treatment of HCC by presentation, the interns in each group selected a corresponding model of HCC (for example: one intern from the 3DPM group should select one 3DPM among the three cases). Nineteen interns in the MDCT group could view the CT images using the imaging software (Maroland picture archiving and communication system, China), which provides both axial and coronal scan visualization. 19 interns in the 3DVR group could view the virtual 3D reconstructions using the visualization software (Vitaworks, China), which enables free rotation and zooming of the images. As for the 24 interns in the 3DPM group, they were allowed to freely handle the models and observe them from various angles.
Outcome assessment
After the end of the clinical education, the teaching effects were evaluated by theoretical examination and questionnaire survey in 90 min. All of the interns were then tested on the hepatic tumor locations (40 points), the vessels adjacent to them (40 points), surgical planning (including assessment of systemic status function, liver function, and designing an appropriate surgical strategy) (10 points), and test time (10 points) using the centesimal system score (total 100 points) by experienced senior teachers (Table 2). A questionnaire investigation including the degree of satisfaction, interest, and helpfulness for improving the comprehension ability of the liver anatomy and 3D spatial structures was also performed. The 3DPM group were compared with both 3DVR and MDCT group by theoretical examination scores as primary endpoints and questionnaire survey satisfaction as secondary endpoints to evaluate the effects of 3DPM on the interns’ clinical education in HCC.
Table 2
| Parameters | Test contents and scoring standard | Score |
|---|---|---|
| Tumor location | Correctly describe the liver segment where the tumor located (40') | 40' |
| Correctly describe the liver lobe where the tumor located (30') | ||
| Correctly describe right or left liver where the tumor located (20') | ||
| Relationship between tumor and vessels | Correctly describe relevant vessels [≥5] to the tumor (40') | 40' |
| Correctly describe relevant vessels [3–4] to the tumor (30') | ||
| Correctly describe relevant vessels [1–2] to the tumor (20') | ||
| Test time | 0–10 min (10') | 10' |
| 10–30 min (8') | ||
| 30–60 min (5') | ||
| Surgical planning | Correctly assess systemic status function, evaluate liver function and make appropriate surgical strategy (10') | 10' |
| Total | 100' |
Statistical analysis
All the data were registered in an electronic database after being double-check by the researchers and analyzed using SPSS 23.0 software (IBM Corporation, USA). The measurement data are expressed as mean ± standard deviation. Independent sample t-tests were performed for both groups. The categorical variables were analyzed using a chi-square analysis or Fisher’s exact probability method. A P value <0.05 was considered statistically significant.
Results
Participant flow
Eligible participants studied in the department of Hepatobiliary Surgery from October 2020 to December 2020 were randomly assigned for each group, please see the participant flow in detail (Figure 2).
Baseline data comparison
Compared with both 3DVR and MDCT group, 3DPM group had no statistically significant difference in age, sex ratio and grade point average (GPA) (GPA ≥3.0 was considered as A, GPA <3.0 was considered as B, and the ratio of A and B students in the group was used as the standard to measure the basic learning situation of the group). As shown in Table 3 (P>0.05), which suggested that interns in the 3DPM group were comparable with the other two groups by statistical analysis.
Table 3
| Parameters | 3DPM (n=24) | 3DVR (n=19) | MDCT (n=19) | P value | |
|---|---|---|---|---|---|
| 3DPM vs. 3DVR | 3DPM vs. MDCT | ||||
| Age (years) | 22.8±0.7 | 22.6±0.6 | 22.8±0.8 | 0.33 | 1 |
| Gender (male/female) | 11/13 | 6/13 | 9/10 | 0.53 | 0.84 |
| GPA (A/B) | 13/11 | 10/9 | 11/8 | 0.84 | 0.95 |
The measurement data are expressed as mean ± standard deviation. Independent sample t-tests were performed for both groups. GPA ≥3.0 was considered as A, GPA <3.0 was considered as B. 3DPM, three-dimensional printing model; 3DVR, three-dimensional virtual reconstruction; MDCT, multi-detector computed tomography; GPA, grade point average.
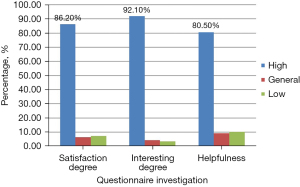
Outcome data comparison
After lecture-based learning, all the interns completed the test and questionnaire with 90 min. The 3DPM group (n=24) had significantly higher scores on the following test contents: indicating the correct tumor location (3DPM vs. 3DVR, MDCT: 36.7±4.8 vs. 33.2±5.8, 26.8±10.0, P=0.03, P<0.01, respectively), accurately identifying the relationship between the tumor and vessels (3DPM vs. 3DVR, MDCT: 37.1±4.6 vs. 31.6±3.7, 30.0±5.8, P<0.01, P<0.01, respectively), and designing appropriate surgical plans (3DPM vs. 3DVR, MDCT: 8±2.7 vs. 4.9±2.7, 5.9±3.8, P<0.01, P=0.04, respectively) than the other two groups. The total scores of the 3DPM group were also significantly higher (3DPM vs. 3DVR, MDCT: 89.4±7.4 vs. 75.8±7.0, 69.5±13.6, P<0.01, P<0.01, respectively) than the other groups (Table 4). The questionnaire investigation of 3DPM application in clinical education showed higher degrees of satisfaction (86.2%), interest (92.1%), and helpfulness (80.5%) for improving the comprehension ability of liver anatomy and 3D spatial structures (Figure 3). Outcomes were available then and no follow-up was required.
Table 4
| Parameters | 3DPM group (n=24) | 3DVR group (n=19) | MDCT group (n=19) | P value | |
|---|---|---|---|---|---|
| 3DPM vs. 3DVR | 3DPM vs. MDCT | ||||
| Tumor location | 36.7±4.8 | 33.2±5.8 | 26.8±10.0 | 0.03 | <0.01 |
| Relationship between tumor and vessels | 37.1±4.6 | 31.6±3.7 | 30.0±5.8 | <0.01 | <0.01 |
| Test time (min) | 7.7±2.1 | 7.3±1.5 | 6.8±1.8 | 0.53 | 0.14 |
| Surgical planning | 8±2.7 | 4.9±2.7 | 5.9±3.8 | <0.01 | 0.04 |
| Total | 89.4±7.4 | 75.8±7.0 | 69.5±13.6 | <0.01 | <0.01 |
The measurement data are expressed as mean ± standard deviation. Independent sample t-tests were performed for both groups. 3DPM, three-dimensional printing model; 3DVR, three-dimensional virtual reconstruction; MDCT, multi-detector computed tomography.
Discussion
In this study, we found that a patient-specific 3DPM of the liver not only improved the comprehension ability of hepatic anatomy and 3D spatial structures but also increased the clinical thinking ability and interest of interns compared with 3DVR and MDCT.
Lecture- and case-based learning are the most commonly used approaches in China, while the educational methods in Western countries are based on student-centered teaching approaches, such as problem-based learning and resource-based learning (9). As for the clinical education of HCC, intrahepatic-specific anatomy is the most relevant information that hard to be mastered, and facilitating the understanding of hepatic anatomy among interns is key. The traditional teaching methods of liver anatomy in China mostly rely on the anatomical atlas, cadaveric anatomy, and 2D imaging (CT or MRI) to achieve cognitive goals. However, these teaching methods are based on normal anatomical structures, leading students to believe that all anatomical structures are the same. However, the liver is an opaque substantial organ with intricate ducts, which often involve variations. Even the same segment where HCC is located is treated differently due to the specificity of different liver anatomies, functions, and systemic conditions.
Therefore, the clinical teaching of HCC should also be individualized. With the development of individualized, accurate, and minimally invasive hepatobiliary surgery, 3D virtual technology has been applied in the diagnosis, treatment, and clinical teaching of hepatobiliary diseases. 3D visualization refers to the application of 3D software to reconstruct and form a virtual 3D hepatic model based on the CT or MRI data of patients, which allows the lesions and important duct details in the liver to be viewed directly. 3DVR technology has been widely used in clinical preoperative planning and intraoperative navigation and overcomes the limitations of traditional, experiential, and textbook-like teaching. Its practical teaching effects are obviously superior to those of traditional teaching methods, which effectively improves the teaching quality (10).
However, 3DVR still has the following shortcomings. First, 3DVR is expressed through virtual models with a lack of real touch and space. Second, 3DVR imaging is still displayed in a 2D plane and overlap with each other. Therefore, inaccurate preoperative evaluation and misunderstandings still occur, especially for complex hepatobiliary diseases (11). Third, some interns may have a low spatial imagination ability, which could result in an incorrect understanding of the virtual images. On the contrary, 3D printing is a technology that transforms 3D virtual models into real objects and can help to solve problems associated with 3DVR. The speed of visual information transfer that the sense of touch offers through the handling of a physical object, which is missing when the same images (either 2D or 3D) are displayed on a screen, is prominent (12). 3DPM of other organs has yielded similar results regarding the clarification of the specific anatomy of solid organs (13,14). The complex intrahepatic ducts can be viewed directly into through a transparent 3DPM of HCC by multiple perspectives. It can improve the cognition and comprehension ability of complex intrahepatic anatomical structures and enhance the accuracy of the hepatectomy strategy (15).
The 3D physical model also plays an important role in anatomical education. 3D printing technology has been widely applied in the clinical teaching of orthopedics and cardiac surgery, achieving better educational effects and higher teaching satisfaction compared with traditional teaching methods (16). 3D liver printing is a valuable tool for understanding the spatial relationships between vascular and biliary anatomical structures (17). In this study, the 3DPM group had significantly higher scores than the other two groups in the following test contents: indicating the correct tumor location (3DPM vs. 3DVR, MDCT: 36.7±4.8 vs. 33.2±5.8, 26.8±10.0, P=0.03, P<0.01, respectively) and relationship between the tumor and vessels (3DPM vs. 3DVR, MDCT: 37.1±4.6 vs. 31.6±3.7, 30.0±5.8, P<0.01, P<0.01, respectively). Compared with the anatomical atlas, CT, MRI, and 3D imaging, a patient-specific 3DPM can display spatial anatomical relations more vividly, and students have higher learning enthusiasm (16). As for the application of 3DPM for the clinical education of interns in this research, we found higher degrees of satisfaction (86.2%), interest (92.1%), and helpfulness (80.5%) for improving the comprehension ability of liver anatomy and 3D spatial structures. Moreover, most interns suggested that it would be better if relevant surgical videos were played during the clinical teaching.
3D printing technology has notably advanced in the past few decades and has been utilized in the field of preoperative surgical planning (18,19). A physical 3D representation of the target anatomical area appears to provide support for surgeons in preoperative planning (17). A patient-specific 3DPM can display individualized anatomical characteristics, such as the shape and position of the hepatic lesions, arteries, and veins. Furthermore, handling these models with both the inflow and outflow structures printed provides a mental reconstruction of the anatomy, which makes the comprehension and memorization of essential details easier (20). This provides convenient and interesting communication between teachers and students, facilitates the understanding of an individual’s HCC clinical characteristics, and allows clinicians to make individualized diagnoses and offer appropriate treatments. The spatial structural relationship of the liver is straight forward in the patient-specific 3DPM. Moreover, with the 3DPM, interns can examine and touch the region of interest, which is considered important for understanding the target anatomy (21,22). These advantages are conducive to improving the ability of clinical thinking about HCC. In this study, the 3DPM group achieved significantly higher scores in designing appropriate surgical plans (3DPM vs. 3DVR, MDCT: 8±2.7 vs. 4.9±2.7, 5.9±3.8, P<0.01, P=0.04, respectively). Precise medicine is the mainstream trend at present, so precise clinical teaching should follow suit (23). A patient-specific 3DPM will play an important role in clinical training and intraoperative real-time navigation in the future.
Conclusions
The clinical teaching by utilizing 3DPM can significantly improve the professional theoretical level, strengthen clinical thinking and comprehensive ability, and improve the teaching effects of HCC for medical interns.
Limitations
This study had several limitations that should be noted. Firstly, a wide variety of patient-specific 3D printing liver models should be applied for the clinical education of HCC to further assess the teaching value of 3D printing technology. Secondly, this study was conducted at a single cancer center instead of multiple centers, and comprised a relatively small number of interns.
Acknowledgments
The authors would like to acknowledge and thank the teaching center of Zhejiang Provincial People’s Hospital for its support.
Funding: This study was supported by the Basic Public Welfare Research Project of Zhejiang Province (No. LGF20H030011) and the Zhejiang Medical and Health Science and Technology Plan (No. 2022RC096).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/rc
Trial Protocol: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/tp
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/dss
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-28/coif). All authors report that this study was supported by the Basic Public Welfare Research Project of Zhejiang Province (No. LGF20H030011) and the Zhejiang Medical and Health Science and Technology Plan (No. 2022RC096). The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study protocol was approved by the Ethics Committee of Zhejiang Provincial People’s Hospital (No. 2021QT333). Informed consent was obtained from all participants. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int J Cancer 2019;144:1941-53. [Crossref] [PubMed]
- Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019;394:1145-58. [Crossref] [PubMed]
- Professional Committee for Prevention and Control of Hepatobiliary and Pancreatic Diseases of Chinese Preventive Medicine Association, Professional Committee for Hepatology, Chinese Research Hospital Association, et al. Guideline for stratified screening and surveillance of primary liver cancer (2020 edition). Journal of Clinical Hepatology 2021;37:286-95. [Crossref] [PubMed]
- Deng WH, Wang ZL, Zhang Z. Exploration and thinking on the construction of clinical medical talent training base under the background of medical-education collaboration. China Modern Doctor 2020;58:149-51.
- Witowski JS, Pędziwiatr M, Major P, et al. Cost-effective, personalized, 3D-printed liver model for preoperative planning before laparoscopic liver hemihepatectomy for colorectal cancer metastases. Int J Comput Assist Radiol Surg 2017;12:2047-54. [Crossref] [PubMed]
- Igami T, Nakamura Y, Oda M, et al. Application of three-dimensional print in minor hepatectomy following liver partition between anterior and posterior sectors. ANZ J Surg 2018;88:882-5. [Crossref] [PubMed]
- Xia J, Yuan H, Chen H, et al. Application and limitations of three-dimensional printing technology in abdominal surgery. Journal of Laparoscopic Surgery 2021;26:388-91.
- Wang C. Application of 3D Printing, PBL and EBL in Orthopedic Teaching. China Continuing Medical Education 2021;13:27-30.
- Ding X, Zhao L, Chu H, et al. Assessing the effectiveness of problem-based learning of preventive medicine education in China. Sci Rep 2014;4:5126. [Crossref] [PubMed]
- Ji B, Sun MH, Wang SP. Application effect of three-dimensional visual practice teaching of liver surgery in standardized residency training. Chinese Journal of Graduate Medical Education 2019;3:335-8.
- Kuroda S, Kihara T, Akita Y, et al. Simulation and navigation of living donor hepatectomy using a unique three-dimensional printed liver model with soft and transparent parenchyma. Surg Today 2020;50:307-13. [Crossref] [PubMed]
- Kappers AM. Human perception of shape from touch. Philos Trans R Soc Lond B Biol Sci 2011;366:3106-14. [Crossref] [PubMed]
- Marconi S, Pugliese L, Botti M, et al. Value of 3D printing for the comprehension of surgical anatomy. Surg Endosc 2017;31:4102-10. [Crossref] [PubMed]
- El Sabbagh A, Eleid MF, Al-Hijji M, et al. The Various Applications of 3D Printing in Cardiovascular Diseases. Curr Cardiol Rep 2018;20:47. [Crossref] [PubMed]
- Yang T, Lin S, Xie Q, et al. Impact of 3D printing technology on the comprehension of surgical liver anatomy. Surg Endosc 2019;33:411-7. [Crossref] [PubMed]
- White SC, Sedler J, Jones TW, et al. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit Heart Dis 2018;13:1045-9. [Crossref] [PubMed]
- Zein NN, Hanouneh IA, Bishop PD, et al. Three-dimensional print of a liver for preoperative planning in living donor liver transplantation. Liver Transpl 2013;19:1304-10. [Crossref] [PubMed]
- Aimar A, Palermo A, Innocenti B. The Role of 3D Printing in Medical Applications: A State of the Art. J Healthc Eng 2019;2019:5340616. [Crossref] [PubMed]
- Burdall OC, Makin E, Davenport M, et al. 3D printing to simulate laparoscopic choledochal surgery. J Pediatr Surg 2016;51:828-31. [Crossref] [PubMed]
- Matsumoto JS, Morris JM, Foley TA, et al. Three-dimensional Physical Modeling: Applications and Experience at Mayo Clinic. Radiographics 2015;35:1989-2006. [Crossref] [PubMed]
- Lee N. The Lancet Technology: 3D printing for instruments, models, and organs? Lancet 2016;388:1368. [Crossref] [PubMed]
- Cheng J, Gong HB, Wang ZF, et al. Optimal design of 3D printing model for complex liver tumors. Chinese Journal of Experimental Surgery 2020;37:603-6.
- Deng QS, Wu CX, Gong JP. Application and effect of 3D printing technology in clinical teaching. Medical Education Management 2019;5:531-5.
(English Language Editor: A. Kassem)


