
The value of using fludeoxyglucose positron-emission tomography scan with respect to colorectal abnormalities—a cross-sectional study
Introduction
Positron-emission tomography (PET) (1) is a functional imaging technique that can be used to observe metabolic processes in the body as an aid to the diagnosis of disease. After tracer administration and a tracer specific uptake period, a co-axial examination range is defined. CT data for attenuation correction and image fusion are acquired followed by the collection of PET emission data. The emission data is subsequently reconstructed without and with CT based attenuation correction. Finally, the functional data from PET is displayed on an anatomical background from CT using two different color lookup tables (2). Today all PET systems for clinical use are combined with CT system.
Mostly, the biologically active molecule used is fludeoxyglucose (FDG). This tracer is a glucose analog that is taken up by glucose-using cells and phosphorylated by hexokinase. Because the oxygen atom is replaced by F-18 in order to generate the labeled FDG, the next step in glucose metabolism in all cells in blocked. Furthermore, most tissues (with the notable exception of liver and kidneys) cannot remove the phosphate added by hexokinase. This means that FDG is trapped in any cell that takes it up until it decays, it cannot exit from the cell. This results in intense radiolabeling of tissues with high glucose uptake, such as the brain, the liver, and most cancers.
As a result, FDG-PET, with the tracer fluorine-18, is widely used for diagnosis, staging, and monitoring treatment of cancers, particularly in Hodgkin’s lymphoma, non-Hodgkin lymphoma, and lung cancer. Nowadays exploration of cancer metastasis (i.e., spreading to other sites) is the most common type of PET scan (90% of current scans). The FDG-PET is also increasingly used for detection and spread of chronic inflammatory processes like vasculitis or sarcoidosis.
To complement molecular information obtained by PET, anatomical correlation obtained by computed tomography (CT) is needed. Hybrid PET/CT imaging allows acquiring molecular and anatomical information in a single whole body examination, without moving the patient in between. FDG PET/CT has a high diagnostic yield with respect to metastatic disease. The usual weight adjusted dose of 4 MBq/kg FDG used in an oncological PET/low dose CT scan has an effective radiation dose in the range of 7.4 mSv (1-3).
Focal FDG uptake in colon and rectum is regularly seen. Colonoscopy is advised in order to detect the origin of this activity. In daily practice in the endoscopy department, it was noticed that more than once no abnormalities responsible for the uptake were seen during endoscopy.
For this reason, all FDG-PET/CT studies done consecutively in a 5-year period were studied in order to gain more information on the findings of colonoscopy in cases of focal FDG uptake in colon or rectum.
Methods
All consecutive FDG-PET/CT studies done in a period of 5 years [2013–2017] were studied.
All patients were scanned with Siemens Biograph 64 PET/CT scanner 60±5 minutes post FDG injection. At the time of FDG administration all patients had fasted for at least 6 hours. The FDG dose was in the range of 200–400 MBq FDG depending of the patient’s body mass index (BMI: range, 20–35 BMI index). PET protocol consisted of 3 minutes scanning per bed position using standard whole body acquisition protocol with 6 or 7 bed positions. The PET data were reconstructed into trans-axial slices using 3D iterative reconstruction (4 iterations/8 subsets, filter Gaussian, FWHM 5 mm, image size 256, zoom 1). The low dose CT scan without intra-venous contrast followed immediately by a PET scan. Low dose CT acquisition protocol consisted: 130 kV, 25 mAs, pitch 0.95 mm, collimation 16×1.2, rotation time 0.6, delay 4 s, FOV 700 mm, slice 4 mm. Corrections for attenuation, random, dead time and normalization were done inside the iterative loop. In addition, fused FDG PET/CT images were made and displayed in coronal, transverse and sagittal planes. The fused PET/CT scan was described by nuclear medicine specialist.
Only scans in which incidental focal FDG uptake above the background (with or without anatomical substrate on low dose CT) in colon and or rectum was seen were included. Focal FDG uptake in colon and rectum were judged as either positive (+) or highly specific (++) for malignancy or polyps.
From each patient the clinical reason for performing the FDG-PET was noted. For each positive case the clinical files and endoscopy reports were searched for further work-up and final diagnosis in colon and or rectum.
Colonoscopy was done, after standard preparation with PEG solution (Moviprep®), with Fujinon colonoscopes. Conscious sedation was done with midazolam 5 mg.
In patients in whom no additional colonoscopy was done, the reason for omitting this procedure was noted.
Statistical analysis was done with Chi-square test for contingency tables. A value below 0.05 was considered statistically significant.
This kind of study does not need approval from an ethical committee in The Netherlands.
Results
In the 5-year period 2,075 FDG-PET/CT scans were done. Seven were excluded because these were repeated scans in the same patient. Focal FDG uptake in the colon and/or rectum was noted in 173 out of 2,068 scans (8.4%); (109 men, 64 women). These scans were used for further evaluation.
Table 1 shows the clinical reasons for the scans. Analysis of pulmonary cancer and search for metastasis in cases of (already diagnosed) colorectal cancer were the most prevalent reasons.
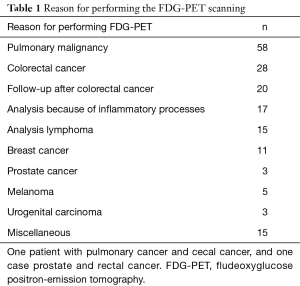
Full table
Focal FDG activity in colon and/or rectum was judged ++ in 73 patients (42.2%) and + in 100 (57.8%). Table 2 shows the uptake in the different sections of the colon and rectum. There was no difference in FDG activity in the proximal colon versus the distal colon and rectum.
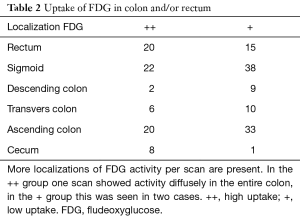
Full table
Table 3 shows the activity of FDG in relation to the clinical indication for doing the scan. As to be expected activity was ++ in the majority of patients with colorectal cancer.
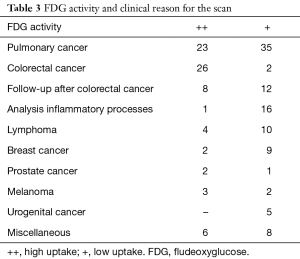
Full table
In 125 patients (72.3%) an additional colonoscopy was done because of the results of the FDG PET/CT scan. Table 4 shows the reasons why this procedure was not done.
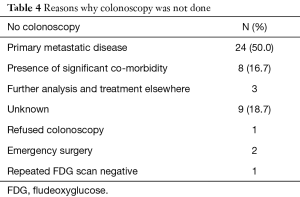
Full table
Patients with ++ activity underwent significantly more often a colonoscopy compared with patients with + activity, 82% versus 65% (P=0.02). This is partly because colonoscopy already was done before the FDG-PET scan (especially in cases of already diagnosed colorectal cancer). All but three patients with colorectal cancer had ++ FDG activity.
Table 5 shows the yield of the diagnostic colonoscopy. FDG PET/CT was false positive with respect to polyp(s) or cancer in 13 cases (22%) of ++ FGD activity and in 38 cases of + FDG (P<0.001).
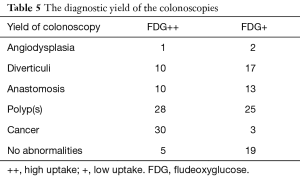
Full table
In 25 patients a total of 69 polyps were not FDG avid, hence these were missed. One case of sigmoid cancer also was missed, while the concurrent cecal carcinoma was FDG avid. In 18 patients these polyp(s) were more than 1 cm in diameter. In the remaining cases the polyp(s) were smaller than 1 cm.
Twenty patients had a prior history of resection because of colorectal cancer. Eighteen of these underwent a follow-up colonoscopy. Two patients were seen with a recurrent cancer, while 5 polyps were detected. In eleven cases no tumors were detected in the colon, hence these scans were false positives.
Discussion
The present study shows FDG uptake in colon and rectum with specific interest in the diagnostic yield of colonoscopy. Positive FDG uptake was noted in 8% of all scans. Treglia et al. did a meta-analysis on results of FDG with respect to colonic uptake. The overall prevalence of FDG uptake was 3.6% in more than 85,000 patients (3). Vella-Boucaud did a study in patients with lung cancer, and 7.3% of patients showed FDG uptake in their colon. In four cases a malignancy in the colon was detected (4). On the other hand lower incidence is also noted. Shmidt et al. found in 0.7% of cases focal uptake in the gastrointestinal tract. The possible explanation is that the study was done in a tertiary referral center, hence a biased population (5). Another study reported uptake in 0.9% of cases. However, all patients with colorectal cancer were excluded on forehand (6).
Apparently, the 28 patients in the present study with colorectal cancer had FDG uptake in colon or rectum. The reason for doing the scan in these cases was not diagnostic with respect to the primary tumor but with respect of staging and the search for distant metastases. In one case a double tumor was missed on FDG scan. In this case the PET avid tumor was well differentiated while the missed tumor was mucinous.
More interesting is the yield in cases with other indications. In all patients (n=124) without colorectal cancer or follow-up after being treated for this cancer and who underwent colonoscopy (n=80) a total of seven colorectal cancers were diagnosed, twice located in a polyp. These cancers were asymptomatic.
Colonoscopy was not done in all cases. If there already was metastasized disease or important co-morbidity rendering the consequence of colonoscopy futile the procedure was omitted.
The yield of FDG-PET for detecting adenomatous polyps of the colon is rather low. Yasuda et al. studied the yield of positive FGD PET. Fourteen out of 59 adenomas 5–30 mm in size were detected. The detection rate increases when adenomas were larger. False-positives were seen in 5.5% of cases (7). Kunawudhi et al. studied patients with a colonic uptake and found almost 50% false-positives with respect to adenomas or colorectal cancer. On the other hand, they also found a high number of false-negatives (8). These patients underwent colonoscopy for clinical reasons and appeared to have neoplastic lesions.
In the present study a total of 69 polyps (hyperplastic as well as adenomatous) were missed with the FDG scan. Hence, the FDG-PET is not an adequate screenings tool for detection of adenomas.
The FDG uptake was judged to be ++ or +. In cases of ++ the number of false-positive with respect to tumor or polyp was 22%, while this was 58% in cases of +. Although interobserver variation in FDG-PET scanning can occur, a study showed that there was a high observer agreement with respect to colonic uptake. ‘FDG uptake patterns’ and ‘FDG uptake degree’ were significantly related to decide on the suspicion of malignancy (P<0.001) and the final result (P<0.001) (9).
Benign lesions like diverticuli, anastomoses or simply normal mucosa can have FDG uptake. Takeshita detected a suture granuloma in the pelvis after prior surgery (10). False-positives even occur after resection of a colon cancer. Orii et al. suspected a local recurrence of colon cancer but histological examination of the resection specimen only showed fatty and fibro-muscular tissue (11). False-positive findings of scanning the colon have been reported due to diverticulitis, colitis, and post-operative scarring (anastomoses) (12). The same was seen in the present study. Anastomoses often have uptake. Activity in the recto-sigmoid region on an FDG PET scan may vary significantly, which may occasionally lead to difficulties in interpretation when assessing local recurrence of colorectal cancer (13). Lee et al. found 11% false positives in the colon. Additional CT-scanning provides clues regarding the localization but does not provide information on the malignant potential (14).
False negatives also occur. In the present study a total of 69 polyps and one colon cancer was not detected with FDG. Also, the additional CT-scan did not detect these lesions. A problem with the combination of both procedures is that there is no specific bowel preparation used for the CT-scan. Unfortunately, the dimensions of the missed polyps were not noted consequently in the endoscopy reports.
From the present study it can be concluded that FDG-PET scanning is a useful tool in assessing metastatic disease. However, false-positive and false-negative findings with respect to colonic uptake are present in a significant number of patients. If the clinical condition and the potential prognosis allows the performance of colonoscopy this procedure should be done in order to gain more information. Colonoscopy can be absolutely essential in order to avoid unnecessary resections. Any positive finding that could lead to a clinically significant change in patient management should be confirmed by subsequent histopathologic examination because of the risk of false-positive results (15).
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lee JC, Hartnett GF, Hughes BG, et al. The segmental distribution and clinical significance of colorectal fluorodeoxyglucose uptake incidentally detected on PET-CT. Nucl Med Commun 2009;30:333-7. [Crossref] [PubMed]
- Kamel EM, Thumshirn M, Truninger K, et al. Significance of incidental 18F-FDG accumulations in the gastrointestinal tract in PET/CT: correlation with endoscopic and histopathologic results. J Nucl Med 2004;45:1804-10. [PubMed]
- Treglia G, Taralli S, Salsano M, et al. Prevalence and malignancy risk of focal colorectal incidental uptake detected by (18)F-FDG-PET or PET/CT: a meta-analysis. Radiol Oncol 2014;48:99-104. [Crossref] [PubMed]
- Vella-Boucaud J, Papathanassiou D, Bouche O, et al. Incidental gastrointestinal 18F-Fluorodeoxyglucose uptake associated with lung cancer. BMC Pulm Med 2015;15:152. [Crossref] [PubMed]
- Shmidt E, Nehra V, Lowe V, et al. Clinical significance of incidental [18 F]FDG uptake in the gastrointestinal tract on PET/CT imaging: a retrospective cohort study. BMC Gastroenterol 2016;16:125. [Crossref] [PubMed]
- Servente L, Gigirey V, García Fontes M, et al. Incidental focal colonic uptake in studies 18F-FDG PET/CT. Rev Esp Med Nucl Imagen Mol 2018;37:15-9. [Crossref] [PubMed]
- Yasuda S, Fujii H, Nakahara T, et al. 18F-FDG PET detection of colonic adenomas. J Nucl Med 2001;42:989-92. [PubMed]
- Kunawudhi A, Wong AK, Alkasab TK, et al. Accuracy of FDG-PET/CT for Detection of Incidental Pre-Malignant and Malignant Colonic Lesions - Correlation with Colonoscopic and Histopathologic Findings. Asian Pac J Cancer Prev 2016;17:4143-7. [PubMed]
- Minamimoto R, Terauchi T, Jinnouchi S, et al. Observer variation study of the assessment and diagnosis of incidental colonic FDG uptake. Ann Nucl Med 2013;27:468-77. [Crossref] [PubMed]
- Takeshita N, Tohma T, Miyauchi H, et al. Suture Granuloma With False-Positive Findings on FDG-PET/CT Resected via Laparoscopic Surgery. Int Surg 2015;100:604-7. [Crossref] [PubMed]
- Orii T, Okumura M, Yoshimura M, et al. An FDG-PET/CT-positive lesion mimicking local recurrence of colon cancer 5 years after radical colectomy. Am J Case Rep 2015;16:149-52. [Crossref] [PubMed]
- O'Connor OJ, McDermott S, Slattery J, et al. The Use of PET-CT in the Assessment of Patients with Colorectal Carcinoma. Int J Surg Oncol 2011;2011:846512. [Crossref] [PubMed]
- Chun H, Kim CK, Krynckyi BR, et al. The usefulness of a repeat study for differentiating between bowel activity and local tumor recurrence on FDG PET scans. Clin Nucl Med 2003;28:672-3. [Crossref] [PubMed]
- Lee ST, Tan T, Poon AM, et al. Role of low-dose, noncontrast computed tomography from integrated positron emission tomography/computed tomography in evaluating incidental 2-deoxy-2-[F-18]fluoro-D-glucose-avid colon lesions. Mol Imaging Biol 2008;10:48-53. [Crossref] [PubMed]
- Fletcher JW, Djulbegovic B, Soares HP, et al. Recommendations on the use of 18F-FDG PET in oncology. J Nucl Med 2008;49:480-508. [Crossref] [PubMed]


