Morbidity and mortality of synchronous hepatectomy with cytoreductive surgery/hyperthermic intraperitoneal chemotherapy (CRS/HIPEC)
Introduction
There are relatively few operative indications for stage IV cancers. Notable exceptions include isolated lung or liver metastasis in GI cancers and cytoreductive surgery (CRS) with hyperthermic intraperitoneal chemotherapy (HIPEC) for peritoneal carcinomatosis. The specific approaches to managing these metastatic lesions have been previously debated. For colorectal cancer patients presenting with synchronous hepatic metastasis, only a minority are suitable for resection (1). Synchronous resection for colon and rectal cancer is considered a safe and effective method of management in patients with isolated liver metastasis. However, there is some concern regarding the safety of synchronous resections when major hepatic resections are required, especially with higher risk colon and rectal resections (1,2).
CRS/HIPEC has been used effectively to treat peritoneal carcinomatosis since the 1980s (3). Traditionally, CRS/HIPEC has been used to treat peritoneal malignancy arising from colorectal adenocarcinoma, appendiceal mucinous carcinoma, and gynecologic malignancies. More recently, this method has been applied to a widening range of pathologies with an associated 5-year survival benefit. The success of the surgery is highly dependent on the extent of disease burden as well as the completeness of the cytoreduction. While cytoreduction alone has been found to be inferior to CRS plus HIPEC, failure to achieve an acceptable minimum residual tumor burden during CRS is a contraindication to proceeding with HIPEC. To aid with assessing successful cytoreduction, pre-operative and intra-operative clinical scores such as the peritoneal carcinomatosis index (PCI) and the cytoreduction completeness (CC) score have been developed (4). However, the use of clinical scoring systems has not been well standardized across surgeons who perform CRS/HIPEC. For colon and rectal malignancies, typical chemotherapeutic agents include Mitomycin-C and oxaliplatin. However, the use of other agents has been previously described (5). The variability of the dissection and resection during CRS/HIPEC has made characterizing morbidity difficult. The procedure is independently associated with expected complications of bleeding, digestive fistula, intra-abdominal abscess, and systemic sepsis, as well as chemotherapy-specific complications such as neutropenia and renal insufficiency (6).
Multiple tools have become available to assist surgeons in characterizing post-operative complications. The Clavien-Dindo classification (CDC) attempts to categorize complications based on the severity of the intervention required for treatment. This score has six categories of increasing severity and ranges from no intervention to patient death (7). The comprehensive complication index (CCI) is a computational score which accounts for all complications associated with an admission (8). Neither score has shown superiority in all cases or to more accurately capture the post-operative course for patients who experience complications. It is not well understood how CRS/HIPEC impacts the morbidity of associated procedures. This is highly relevant in cases such as synchronous resection of hepatic metastasis where the benefit appears to be rapidly offset by added morbidity. We propose to quantify the additional morbidity of CRS/HIPEC in the setting of synchronous colorectal and liver resection using these operative complication scoring systems. Doing so will assist surgeons in patient selection and may help to minimize harm in patients undergoing morbid procedures.
Methods
A query of the University of Kansas Medical Center billing data was used to assemble a patient list according to Current Procedural Terminology (CPT) codes for CRS/HIPEC. This study was approved by the University of Kansas Institutional Review Board. Patients were included who underwent CRS/HIPEC between 2005 and 2016. All patients had colon, rectal or high-grade appendiceal adenocarcinoma primary malignancy. All patients were undergoing concurrent colon resection at the time of CRS/HIPEC and/or hepatectomy. Patients who had the primary tumor resected at a prior operation were excluded. Data was abstracted from patient charts to include basic demographics, comorbidities, intra-operative details, and recurrences. The study group was defined as patients who underwent hepatectomy in addition to CRS/HIPEC. Those patients who underwent colectomy with CRS/HIPEC without hepatectomy formed the control group for this study. CRS included patients who underwent omentectomy, peritonectomy, and diaphragm stripping. Patients undergoing additional abdominal or pelvic organ resection were excluded from either group. CDC and CCI scores were assessed based on manual review of patient charts. Results were tabulated and means were compared using the Student’s t-test. When applicable, percentages were compared using the Z test for proportions.
Results
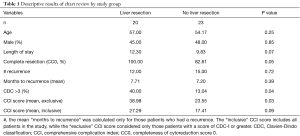
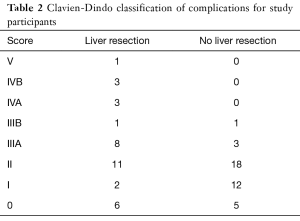
The primary study findings are summarized in Table 1. There were 43 patients included in this study, of which 20 underwent CRS/HIPEC and hepatectomy. Patient ages ranged from 29 to 83. The study groups were similar in terms of age, sex, length of stay, and completeness of resection. There was a trend toward longer hospital stays with hepatectomy, but the result was not significant (12.3 vs. 9.8 days, P=0.07). Of the 20 patients who underwent hepatectomy, 16 underwent minor hepatectomy. For major hepatectomy, two patients underwent three or more segmental resections, and two patients underwent formal lobectomy. There were no incomplete resections in the hepatectomy group, and three patients only achieved a CC score of 1 rather than 0 within the non-hepatectomy group. This difference was not significant. Two of the three patients with incomplete resection had documented recurrences on follow-up. The overall incidence of recurrence was similar between hepatectomy and non-hepatectomy groups (12 vs. 15 individuals, P=0.72) as was the average months to recurrence (7.71 vs. 7.20 months, P=0.39). There were significantly more patients with complications scored CDC III or above within the hepatectomy group (40.00% vs. 13.04%, P=0.04), and there were no patients in the non-hepatectomy group to experience a CDC IV or higher complication. There was one CDC V complication observed in the hepatectomy group (Table 2). The average CCI for patients who experienced a complication was greater for the hepatectomy group compared to the non-hepatectomy group (38.98 vs. 23.55, P=0.03). However, the average CCI between groups including all patients was similar (27.29 vs. 17.41, P=0.09). Perioperative and overall mortality between groups was similar.
Full table
Full table
Discussion
In this study, we retrospectively examined the morbidity of hepatectomy in combination with CRS/HIPEC. Previous reports have demonstrated the safety of synchronous minor hepatectomy with colon and rectal resection. While CRS/HIPEC is commonly performed at the same time as colectomy, the impact of combining these procedures had not been previously studied. As a general consideration, it is best to limit the number of separate operations for any individual patient to minimize risk. At times, however, the morbidity associated with aggressive surgical intervention can warrant a staged approach. We found an increased rate of CDC III or greater complications with hepatectomy when added to CRS/HIPEC. These were most commonly percutaneous interventions and sepsis requiring intensive care unit (ICU) care. While there was an increase in the average CDC with hepatectomy, the difference in the CCI between groups was not significant. This was primarily due to the relatively high frequency of CDC II complications between both groups which attenuated the impact of the CDC III or greater complications seen with hepatectomy. Additionally, this study was likely underpowered to detect smaller differences between groups. It is possible that an increased sample size might have shown a significant difference in the CCI. However, comparison of only those patients who experienced complications did reveal a significantly higher CCI score for hepatectomy, while the overall number of patients who had complications was similar. This finding may suggest that patients undergoing CRS/HIPEC and hepatectomy more severe complications, but at similar rates to CRS/HIPEC with colectomy only.
Additionally, there has been some debate over synchronous major hepatectomy with colon or rectal resections. In this series, there were four patients who fit criteria for major hepatectomy. Two of these patients had no significant complications, one patient received a single unit of blood intra-operatively resulting in a CDC-II, and the final patient required percutaneous intervention. Despite an inadequate sample size of major hepatectomy for a formal statistical analysis, there was no trend in the rates of complications for these patients. That two of the patients had no discernable complications and a third was limited to a single blood transfusion is promising that there may be no clinically relevant risk to major vs. minor hepatectomy in conjunction with CRS/HIPEC. However more work is needed before drawing any conclusions on this subject. Additionally, while patients undergoing synchronous hepatectomy did have more severe complications, it remains unclear if this would be avoided with delayed hepatectomy.
This study was limited by its retrospective design. Retrospective chart reviews have well-documented shortcomings including bias and issues with incomplete documentation. It is unlikely, however, that any complication requiring intervention would go undocumented, and, therefore, all data regarding CDC III complications and greater is expected to be complete. While the CDC and CCI systems have been examined in selected patient populations, it is unclear how well these systems capture patients undergoing CRS/HIPEC. Furthermore, the Clavien-Dindo system includes events that could be considered routine post-operative care, such as prophylactic electrolyte replacement. In our study, we did not score patients who lacked clinical evidence of an electrolyte deficiency. At this institution, most inpatients will receive small doses of oral or intravenous electrolyte supplementation for “low-normal” laboratory measurements as a means of prophylaxis. The Clavien-Dindo system does not adequately account for such strategies which will result in drift and additional noise within the CCI calculations. Additionally, the CDC score does not differentiate between complications caused by the surgeon or by other providers. For example, treating anemia with a blood transfusion is a CDC II event. However, it is not uncommon for patients to receive blood intra-operatively based on estimated blood loss without meeting more traditionally accepted thresholds for clinically relevant post-operative anemia. It is also likely in these circumstances that the procedure itself influences other providers on their decision to transfuse which may artificially inflate the complication scores for these patients. Another important limitation is the lack of scoring for the severity of peritoneal disease, as this is likely to increase the needed dissection and therefore the morbidity of the procedure. Scoring systems such as the PCI were not recorded at the time of operation for these patient groups and were therefore unavailable for analysis.
Conclusions
This study lays ground work for the use of complication scoring systems in CRS/HIPEC. Despite some shortcomings, these systems provide an objective assessment of a patient’s post-operative course. We also raise concerns that synchronous hepatectomy may increase the severity of individual complications. However, a direct comparison between synchronous hepatectomy and delayed hepatectomy in patients requiring CRS/HIPEC would be more able to answer this question.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the University of Kansas institutional review board (No. 00140094). An IRB-approved waiver of informed consent was granted due to the entirely retrospective nature of the study.
References
- Collins D, Chua H. Contemporary surgical management of synchronous colorectal liver metastases. F1000Res 2017;6:598. [Crossref] [PubMed]
- Shubert CR, Habermann EB, Bergquist JR, et al. A NSQIP Review of Major Morbidity and Mortality of Synchronous Liver Resection for Colorectal Metastasis Stratified by Extent of Liver Resection and Type of Colorectal Resection. J Gastrointest Surg 2015;19:1982-94. [Crossref] [PubMed]
- Neuwirth MG, Alexander HR, Karakousis GC. Then and now: cytoreductive surgery with hyperthermic intraperitoneal chemotherapy (HIPEC), a historical perspective. J Gastrointest Oncol 2016;7:18-28. [PubMed]
- Harmon RL, Sugarbaker PH. Prognostic indicators in peritoneal carcinomatosis from gastrointestinal cancer. Int Semin Surg Oncol 2005;2:3. [Crossref] [PubMed]
- Valle SJ, Alzahrani NA, Liauw W, et al. Hyperthermic Intraperitoneal Chemotherapy (HIPEC) Methodology, Drugs and Bidirectional Chemotherapy. Indian J Surg Oncol 2016;7:152-9. [Crossref] [PubMed]
- Newton AD, Bartlett EK, Karakousis GC. Cytoreductive surgery and hyperthermic intraperitoneal chemotherapy: a review of factors contributing to morbidity and mortality. J Gastrointest Oncol 2016;7:99-111. [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of Surgical Complications: A New Proposal With Evaluation in a Cohort of 6336 Patients and Results of a Survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Slankamenac K, Nederlof N, Pessaux P, et al. The comprehensive complication index: a novel and more sensitive endpoint for assessing outcome and reducing sample size in randomized controlled trials. Ann Surg 2014;260:757-62; discussion 762-3. [Crossref] [PubMed]


