Brain metastasis and herniation in a patient with ampullary adenocarcinoma presenting with jaundice and memory loss: case report
Introduction
Periampullary carcinoma are neoplasms arising from the head of the pancreas, common bile duct, duodenum or the ampulla of Vater accounting for 5% of malignancies that rise from the gastrointestinal (GI) tract (1). Ampullary adenocarcinoma (AA) is one of the rare periampullary carcinomas as it represents only 6–9% of periampullary malignancies (2). Ampullary adenocarcinoma usually present with abdominal pain, vomiting, obstructive jaundice, loss of weight & appetite (3).
Although ampullary adenocarcinoma has a tendency for early lymph node metastasis, but patients usually present before having a further distant organ metastasis which is often intra-abdominal and rarely extra-abdominal which mostly occur in older age group in the reported cases of extra abdominal metastases (4,5).
The surgical management of ampullary adenocarcinoma depends on whether the tumor is resectable or not; and if so, the treatment of choice would be pancreaticoduodenectomy with regional lymphadenectomy. However, in case of unresectable tumor there are two choices regarding the primary tumor and they are either stenting or surgical bypass to palliatively relieve the obstructive jaundice (3).
Case presentation
We are reporting a case of a 41-year-old male, previously medically free who presented to our hospital as a case of obstructive jaundice and weight loss over a period of one month. Clinical evaluation revealed memory loss, headache, blurred vision and ataxia hindering the patient’s daily activities. Endoscopic retrograde cholangiopancreatography (ERCP) was carried out and showed a mass in the ampullary area. Biopsy was taken and histopathology came as ampullary adenocarcinoma. Metastatic work up was done including:
- Tumor markers which were as follows—CA-19-9: 4,427 IU/mL, CEA: 1.67 IU/mL;
- CT chest, abdomen and pelvis with contrast showed: bilateral pulmonary nodules, multiple lesions in the liver, significant necrotic retroperitoneal lymph nodes in the portocaval area displacing the celiac and portal axes;
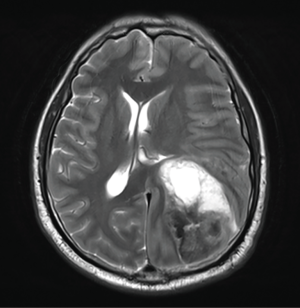
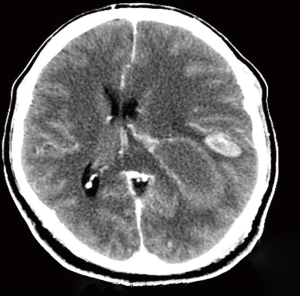
- Brain MRI & CT showed: two hemorrhagic lesions associated with surrounding edema and mass effect (Figure 1). The largest lesion involved the posterior aspect of the frontal lobe and the superior aspect of the temporal lobe and occipital lobe measuring 6.7 cm × 4.7 cm × 5.3 cm (Figure 1). The smaller lesion was within the left supramarginal gyrus 2.1 cm × 0.9 cm × 2.2 cm (Figure 1 and in CT scan in Figure 2). Also, there was edema and midline shift by 0.9 cm to the right with slight downward herniation with impending left uncal herniation;
- PET scan showed uptake in: multiple bilateral lung nodules, multiple liver lesions, and multiple abdominal lymph nodes;
- Liver biopsy showed: moderately differentiated adenocarcinoma.
So, the decision was to keep the patient on palliative care including; methotrexate and mannitol to decrease the intra cranial pressure and radiation therapy for the systematic metastasis involving the brain. Later on, his condition got complicated by difficulty in swallowing and recurrent vomiting that ended up with aspiration pneumonia. Unfortunately, the patient died three months after his presentation due to the aspiration pneumonia followed by cardiac arrest.
Discussion
In the literature, Hsu et al. reported a case series of 135 patients were diagnosed with ampullary carcinoma that underwent pancreaticoduodenectomy with regional lymphadenectomy. Forty-two percent of patients had disease recurrence and metastasis during follow-up, 19% of them were locoregional recurrences, 23% liver metastases, 7% peritoneal carcinomatosis, 5% bone metastases, and 4% metastases at other sites but no brain metastases were mentioned (6).
Extra-abdominal metastases of ampullary adenocarcinoma are much less common than intra-abdominal ones. The rarity of such cases is most likely due to the aggressiveness of such tumors & also due to the fact that the patients don’t survive long enough to develop such extra abdominal distant metastasis. It is also a possibility that the actual incidence is higher than reported as many patients may have not been evaluated for a central nervous system (CNS) lesion as a cause for their presentation. Matsuoka et al. and Voutsadakis et al. reported the only two cases of brain metastasis from ampullary (5,7). While Nassar et al. reported two cases of neuroendocrine carcinoma of the ampulla with brain metastasis. Goto et al., Moriya et al. and Pih et al. have reported cases of lung metastases from ampullary cancer patients whom underwent lung metastasectomy (8-11).
Metastatic brain tumors are the commonest intracranial neoplasm in adult. The majority of brain metastases originate commonly from lung cancer (50%), breast cancer (25%), and melanoma (20%), among these the melanoma has the highest tendency to metastasize to the brain with rate of 50% in each case of melanoma (12). Variable factors should be considered in managing brain metastases which include: age, performance status, number of brain metastases (single or multiple), primary tumor type, and systemic tumor activity (controlled versus uncontrolled). The management of brain metastases can be divided into symptomatic and therapeutic strategies. Symptomatic therapy includes corticosteroids and osmotic diuretics (mannitol) to minimize peritumoral edema. Anticonvulsants could be given to prevent recurrent seizures. Therapeutic therapy of brain metastases includes curative surgical resection or debulking, whole brain radiotherapy (WBRT), stereotactic radiosurgery (SRS), and chemotherapy (13).
In our case the patient had multiple metastatic brain lesions which lead us to apply multiple metastatic brain lesions management which showed significant improvement in his symptoms and ability to resume his daily activities in the first couple of weeks. The approach to patients with multiple brain metastases has evolved over the last decade, particularly for patients with a limited number of tumors, as SRS has become more widely available. There are many trials support use of SRS as the initial therapy for up to four brain metastases each less than 3 cm in diameter. In case of large multiple tumors WBRT remains the standard approach. Kalkanis et al. published a systematic review for the role of SRS in the management of brain metastases. There are two randomized control trials (RTC) that show a single-dose SRS + WBRT provide significantly superior local tumor control compared to WBRT alone for patients with 1–3 brain metastases. In comparing using of SRS alone versus WBRT + SRS, One RCT supports equivalent survival results for single dose SRS alone vs. WRBT + single dose SRS, although adjunctive WBRT reduces the relative risk of intracranial disease progression by approximately 50% but it doesn’t extend the overall survival and is associated with neurocognitive decline (14).
Conclusions
We are reporting the third case of brain metastasis from ampullary adenocarcinoma. It metastasizes commonly intra-abdominally, but extra-abdominal metastases are rare yet it should be included in the differential diagnosis of patients with a history of ampullary carcinoma who present with neurological symptoms. There are no current specific management guidelines for brain metastasis secondary to ampullary adenocarcinoma, so general brain metastasis management could be applied.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Sunil BJ, Seshadri RA, Gouthaman S, et al. Long-Term Outcomes and Prognostic Factors in Periampullary Carcinoma. J Gastrointest Cancer 2017;48:13-9. [Crossref] [PubMed]
- Chavez MT, Sharpe JP, O'Brien T, et al. Management and outcomes following pancreaticoduodenectomy for ampullary adenocarcinoma. Am J Surg 2017;214:856-61. [Crossref] [PubMed]
- Pancreatric Section, British Society of Gastroenterology; Pancreatic Society of Great Britain and Ireland; Association of Upper Gastrointestinal Surgeons of Great Britain and Ireland, et al. Guidelines for the management of patients with pancreatic cancer periampullary and ampullary carcinomas. Gut 2005;54 Suppl 5:v1-16. [Crossref] [PubMed]
- Askew J, Connor S. Review of the investigation and surgical management of resectable ampullary adenocarcinoma. HPB (Oxford) 2013;15:829-38. [Crossref] [PubMed]
- Voutsadakis IA, Doumas S, Tsapakidis K, et al. Bone and brain metastases from ampullary adenocarcinoma. World J Gastroenterol 2009;15:2665-8. [Crossref] [PubMed]
- Hsu HP, Yang TM, Hsieh YH, et al. Predictors for patterns of failure after pancreaticoduodenectomy in ampullary cancer. Ann Surg Oncol 2007;14:50-60. [Crossref] [PubMed]
- Matsuoka G, Wanifuchi H, Suzuki S, et al. A brain metastasis from ampullary carcinoma: a case report. No Shinkei Geka 2013;41:143-8. [PubMed]
- Nassar H, Albores-Saavedra J, Klimstra DS. High-grade neuroendocrine carcinoma of the ampulla of vater: a clinicopathologic and immunohistochemical analysis of 14 cases. Am J Surg Pathol 2005;29:588-94. [Crossref] [PubMed]
- Goto T, Urakami H, Akanabe K, et al. Solitary pulmonary metastasis from carcinoma of the papilla of vater. Ann Thorac Cardiovasc Surg 2011;17:404-7. [Crossref] [PubMed]
- Moriya T, Kimura W, Hirai I, et al. Twelve years survival with repeated hepatectomy and lung resection for metastasis from carcinoma of the papilla of Vater after pancreaticoduodenectomy. Hepatogastroenterology 2007;54:1652-4. [PubMed]
- Pih GY, Kim DK, Park KM, et al. Bilateral lung metastasectomy in carcinoma of the ampulla of Vater. Thorac Cancer 2017;8:124-7. [Crossref] [PubMed]
- Nayak L, Lee EQ, Wen PY. Epidemiology of brain metastases. Curr Oncol Rep 2012;14:48-54. [Crossref] [PubMed]
- Yaeger KA, Nair MN. Surgery for brain metastases. Surg Neurol Int 2013;4:S203-8. [Crossref] [PubMed]
- Kalkanis SN, Kondziolka D, Gaspar LE, et al. The role of surgical resection in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 2010;96:33-43. [Crossref] [PubMed]