Advanced age does not increase morbidity in pancreaticoduodenectomy
Introduction
Periampullary cancer predominantly affects elderly patients, with 40% aged more than 75 years at the time of diagnosis (1). Since the 90’s, several studies have demonstrated low mortality rates after pancreaticoduodenectomy (PD), however morbidity still remains high (40%) (2,3). As surgery is the only curative treatment available for these tumors, it is essential to consider the survival benefit in elderly patients against the risks of severe complications.
Previous studies reported contradictory data regarding morbidity and mortality associated with PD in elderly patients (3,4). Although some authors have found similar complication rates between groups, others have shown that elderly patients usually have longer stay in the intensive care unit (ICU) and require more readmissions after PD (4-6). Recent publications are focused in establishing perioperative factors associated with overall morbidity and classifying severity of the complications, as mild ones have little clinical significance (7-9).
The aim of this study was to assess the safety of surgical treatment for periampullary cancer in patients older than 75 years in such demanding procedures.
Methods
This present study was approved by the institutional ethics committee. Consecutive patients with periampullary tumors who underwent pancreaticoduodenectomy between January 2009 and October 2014 were retrospectively reviewed from a prospectively maintained database. The cohort was divided into two groups according to age: <75 and ≥75 years old.
Primary outcome was severe complications. Secondary outcomes were overall complications, length of ICU and hospital stay, readmission rate and 30-day mortality. Preoperative factors, intraoperative data and postoperative outcomes were compared between groups. Pancreatic fistula and delayed gastric emptying were defined according to the International Study Group of Pancreatic Surgery definitions (10,11). Complications were recorded using the Clavien-Dindo classification system (12). Severe complication was defined as Clavien-Dindo classification ≥3.
All patients underwent open PD and the pylorus was preserved whenever possible. Reconstruction was performed with a double jejunal loop technique, as standardized in our institution since 1976 (13). All procedures were performed by the same team of three experienced pancreatic surgeons.
Quantitative variables were expressed as mean ± standard deviation (SD) or median and compared using Student t-test. Qualitative variables were expressed as number and percentage and compared by means of chi-square or Fisher exact test, when appropriate. The significance level was set as P<0.05. Additionally, multivariate logistic regression was used to generate odds ratio for factors associated with major complication. Statistical analysis was carried out with SPSS software version 20.0 (SPSS, Inc. Chicago, IL).
Results
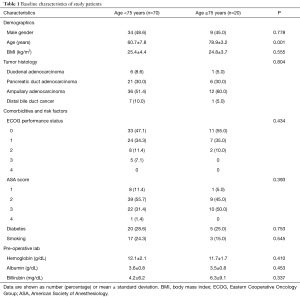
A total of 90 patients who underwent PD were included in the final analysis. Among these, 20 (22.2%) were aged ≥75 years (median age: 78.9±3.2 years). Patient demographic characteristics and preoperative variables are shown in Table 1. Except for the age itself, there were no statistically significant differences between groups.
Full table
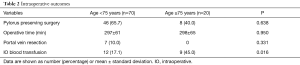
Intra-operative outcomes are outlined in Table 2. Although there was no difference in preoperative hemoglobin level, elderly patients received more red blood cells transfusion (17.1% vs. 45.0%; P=0.016). No difference was observed in terms of operative technique, operative time and vascular resection.
Full table
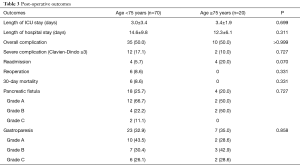
As shown in Table 3, overall and specific complication s, such as pancreatic fistula and gastroparesis, were similar in both groups. Although the incidence of severe complications (17.1% vs. 10.0%; P=0.727) and 30-day mortality (8.6% vs. 0%; P=0.331) was higher in younger patients, these differences were not statistically significant. The elderly group had no re-operation, no mortality and only 2 cases (10.0%) of severe complication (acute kidney failure after pancreatic fistula and gastrointestinal bleeding after cardiogenic shock), but a higher rate of readmission (20%) was observed, although not statistically significant. Furthermore, the younger group had 12 (17.1%) patients with severe complications: 4 related to pancreatic fistula, 2 extra-luminal bleeding, 2 intestinal obstruction and the other 4 due to clinical complications. Early re-operation were required in 6 of these patients.
Full table
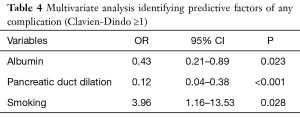
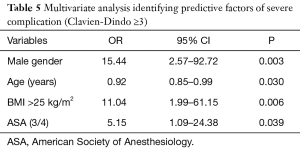
Risk factors that were predictive of complications are shown in Tables 4 and 5. Considering any complication (Clavien-Dindo ≥1), multivariate analysis showed that smoking is an independent risk factor (P=0.028), but higher albumin values (P=0.023) and pancreatic duct dilation (P<0.001) are protective factors for any complications. Furthermore, in multivariate analysis for severe complication (Clavien-Dindo ≥3), male gender (P=0.003), BMI >25 kg/m2 (P=0.006) and American Society of Anesthesiologists (ASA) physical status classification system score 3 or 4 (P=0.039) were noted to be independent risk factors. Moreover, older age (P=0.030) was found to be a protective factor against it.
Full table
Full table
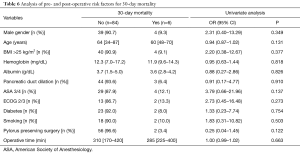
Pre- and post-operative variables for 30-day mortality are disposed in Table 6. None of these were associated with mortality.
Full table
Discussion
Contrary to previous studies that have shown older age to be a risk factor for morbidity and mortality after PD (8,9,14), our study found that patients aged ≥75 years old have the same rates of severe complications and 30-day mortality as younger patients. As there are dissonant results in the literature, it is difficult to make an assumption based on the current data, but we believe that careful selection of elderly patients is of paramount importance to find better results in these patients.
In our series, increased ASA score was an important risk factor for severe complications, in accordance with previous studies (8,14). However, it must be considered that elderly patients have more comorbidities and use of medication, so ASA score alone should not be used as an exclusion criteria for surgical treatment, as done by Sulpice et al. (9) Prior to PD in elderly, it is important to perform a geriatric assessment (GA) to identify individuals who are at higher risk and treat reversible conditions to improve outcome, as recently shown by Dale et al. (15). Even though other studies chose age cutoff as 80 years old (7,14), we used 75 years old because it is considered by geriatricians as the threshold in patient management and it is the life expectancy in Brazil (16).
Male gender and higher BMI are known risk factors for complications after PD. In a recent study by Okano et al. (17), both variables were independently associated with infectious complications. Previous studies showed male gender to be related to specific complications, such as surgical site infection, pancreatic fistula and delayed gastric emptying (17-19). Recent studies have shown visceral fat as a predictor for pancreatic fistula and postoperative mortality (20,21). Knowing that both male gender and higher BMI are associated with visceral fat, this could be an important pre-operative data in further studies. Restricted by the limited number of patients and low incidence of complications, our study could not calculate the specific complications associated with preoperative risk factors.
As observed by de la Fuente et al. (8), elderly patients had a higher incidence of intraoperative blood transfusion despite of same preoperative hemoglobin levels. This fact is not necessarily a sign of bleeding or poor surgical performance, but it is more likely linked to lower volume variation tolerance during surgery due to baseline chronic diseases.
Although no elderly patient died during the study, the difference in mortality between both groups was not statistically significant. As mortality was a rare event and the number of patients in this study is limited, we were not able to establish any risk factor associated with that.
Despite prospectively collected, this study was limited by its observational design derived from a single center. Different from previous studies (9,22,23), we selected patients only with periampullary neoplasms to avoid confounding factors. Our judicious selection of patients for comparison and the decreasing rate of PD indication in elderly (24) may be the reasons for our limited number of patients despite being in a referral oncologic center.
In conclusion, our study revealed PD to be safe in patients aged ≥75 years old. Severe complication was found to be associated with clinical preoperative variables such as male gender, higher ASA score and overweight. In clinical practice, the decision to perform a major abdominal surgery must not be based only on chronological age, but in clinical and functional scores and discussed in a multidisciplinary context.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by Ethics Committee for Analysis of Research Projects of University of São Paulo Medical School General Hospital (No. 13015) and informed consent was taken from all the patients.
References
- SEER Cancer Statistics Review, 1975-2010, National Cancer Institute. Available online: http://seer.cancer.gov/csr/1975_2012/
- van Heek NT, Kuhlmann KF, Scholten RJ, et al. Hospital volume and mortality after pancreatic resection: a systematic review and an evaluation of intervention in the Netherlands. Ann Surg 2005;242:781-8; discussion 788-90. [Crossref] [PubMed]
- Cameron JL, Riall TS, Coleman J, et al. One thousand consecutive pancreaticoduodenectomies. Ann Surg 2006;244:10-5. [Crossref] [PubMed]
- Lightner AM, Glasgow RE, Jordan TH, et al. Pancreatic resection in the elderly. J Am Coll Surg 2004;198:697-706. [Crossref] [PubMed]
- Melis M, Marcon F, Masi A, et al. The safety of a pancreaticoduodenectomy in patients older than 80 years: risk vs. benefits. HPB 2012;14:583-8. [Crossref] [PubMed]
- Yermilov I, Bentrem D, Sekeris E, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol 2009;16:554-61. [Crossref] [PubMed]
- Tani M, Kawai M, Hirono S, et al. A pancreaticoduodenectomy is acceptable for periampullary tumors in the elderly, even in patients over 80 years of age. J Hepatobiliary Pancreat Surg 2009;16:675-80. [Crossref] [PubMed]
- de la Fuente SG, Bennett KM, Pappas TN, et al. Pre- and intraoperative variables affecting early outcomes in elderly patients undergoing pancreaticoduodenectomy. HPB 2011;13:887-92. [Crossref] [PubMed]
- Sulpice L, Rayar M, D'Halluin PN, et al. Impact of age over 75 years on outcomes after pancreaticoduodenectomy. J Surg Res 2012;178:181-7. [Crossref] [PubMed]
- Bassi C, Dervenis C, Butturini G, et al. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 2005;138:8-13. [Crossref] [PubMed]
- Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761-8. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Machado MC, da Cunha JE, Bacchella T, et al. A modified technique for the reconstruction of the alimentary tract after pancreatoduodenectomy. Surg Gynecol Obstet 1976;143:271-2. [PubMed]
- Lee DY, Schwartz JA, Wexelman B, et al. Outcomes of pancreaticoduodenectomy for pancreatic malignancy in octogenarians: an American College of Surgeons National Surgical Quality Improvement Program analysis. Am J Surg 2014;207:540-8. [Crossref] [PubMed]
- Dale W, Hemmerich J, Kamm A, et al. Geriatric assessment improves prediction of surgical outcomes in older adults undergoing pancreaticoduodenectomy: a prospective cohort study. Ann Surg 2014;259:960-5. [Crossref] [PubMed]
- Tábua completa de mortalidade para o Brasil – 2015 Breve análise da evolução da mortalidade no Brasil. Available online: ftp://ftp.ibge.gov.br/Tabuas_Completas_de_Mortalidade/Tabuas_Completas_de_Mortalidade_2015/tabua_de_mortalidade_analise.pdf
- Okano K, Hirao T, Unno M, et al. Postoperative infectious complications after pancreatic resection. Br J Surg 2015;102:1551-60. [Crossref] [PubMed]
- Fujiwara Y, Shiba H, Shirai Y, et al. Perioperative serum albumin correlates with postoperative pancreatic fistula after pancreaticoduodenectomy. Anticancer Res 2015;35:499-503. [PubMed]
- Eisenberg JD, Rosato EL, Lavu H, et al. Delayed Gastric Emptying After Pancreaticoduodenectomy: an Analysis of Risk Factors and Cost. J Gastrointest Surg 2015;19:1572-80. [Crossref] [PubMed]
- Pecorelli N, Carrara G, De Cobelli F, et al. Effect of sarcopenia and visceral obesity on mortality and pancreatic fistula following pancreatic cancer surgery. Br J Surg 2016;103:434-42. [Crossref] [PubMed]
- Tranchart H, Gaujoux S, Rebours V, et al. Preoperative CT scan helps to predict the occurrence of severe pancreatic fistula after pancreaticoduodenectomy. Ann Surg 2012;256:139-45. [Crossref] [PubMed]
- Makary MA, Winter JM, Cameron JL, et al. Pancreaticoduodenectomy in the very elderly. J Gastrointest Surg 2006;10:347-56. [Crossref] [PubMed]
- Sukharamwala P, Thoens J, Szuchmacher M, et al. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB 2012;14:649-57. [Crossref] [PubMed]
- Riall TS. What is the effect of age on pancreatic resection? Adv Surg 2009;43:233-49. [Crossref] [PubMed]


