Biomarkers for immune therapy in colorectal cancer: mismatch-repair deficiency and others
Introduction
Colorectal cancer (CRC) is one of the most common cancer worldwide and the third leading cause of cancer-related deaths in the United States. In 2015 there was estimated to be 132,700 new cases and 49,700 deaths related to CRC (1). Individuals who are diagnosed with early stage CRC (stage I–III) usually have a good prognosis with a 5-year survival exceeding 50%, however patients with metastatic disease have a less than 12% survival at 5 years. With better understanding of the disease biology, effective combinations of cytotoxic chemotherapy and biologic agents have improved overall survival (OS) and progression free survival (PFS). At the molecular level, CRC is a heterogeneous disease that harbors many distinct genetic characteristics and thus molecular testing is performed to identify patients who are candidates for targeted biologic agents or immunotherapy (2).
CRC biomarkers that have been evaluated include KRAS, NRAS, and BRAF mutation (MT), DNA mismatch repair (MMR) status, microsatellite instability (MSI), and CpG island methylation (Table 1) (3). The mutational status of KRAS and NRAS is indicative of worse prognosis, and its presence predicts the lack of efficacy of anti-epidermal growth factor receptor (anti-EGFR) antibody therapy (4,5). Approximately 8–10% patients with CRC have a MT in BRAF V600E (6). It has been consistently shown these individuals have a more aggressive disease and worse outcome in the adjuvant and metastatic setting (7,8). Interestingly, individuals who have BRAF MT and microsatellite instability-high (MSI-H) tumors have a better overall prognosis compared to those who have BRAF MT and microsatellite stable (MSS) disease. MSI has growing importance in CRC, not only to screen for Lynch syndrome but also to identify individuals who could benefit from immunotherapy. In this manuscript, we will discuss the role of DNA MMR, MSI, tumor-infiltrating lymphocytes (TILs), programmed death protein-1 (PD-1), and programmed death-ligand 1 (PD-L1) as potential biomarkers.
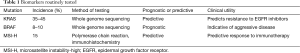
Full table
Biomarkers for immunotherapy
DNA MMR and MSI
The majority of patients develop CRC as a result of chromosomal instability but approximately 15% patients develop CRC due to abnormalities in DNA MMR. Deficient MMR can be secondary to germline MTs or sporadic hypermethylation, which silences DNA MMR genes (2). The main function of MMR proteins is to maintain genomic stability by correcting for single base nucleotide mismatches, insertions or deletions that can arise during DNA replication (9). Furthermore, the MMR proteins also regulate genetic recombination by correcting mismatches that occur during meiosis and mitosis (10). The four main MMR genes are MLH1, MSH2, MSH6, and PMS2, and germline defect in these genes are characteristic of Lynch syndrome. These genes can form heterodimers in various combinations; the most common are MSH2/MSH6 and MLH1/PMS2 (11). MSI-H tumors due to sporadic causes, are a result of epigenetic silencing of the MLH1 promoter (12,13).
Microsatellites are defined as repeat DNA sequences consisting of 2–5 base pairs, usually occurring 10–60 times, and are scattered throughout coding and noncoding regions of the genome. MSI refers to the replicative error phenotype caused by MTs in MMR and is subdivided into two groups: MSI-H or MSS (14). Patients who have tumors deficient of DNA MMR carry the phenotype MSI-H and tumors that are proficient in MMR carry the phenotype MSS. Patients who have MSI-H due to either the sporadic or hereditary cause have tumors that share similar histologic features that are mucin-rich, signet ring and medullary types and have increased number of TILs (15). Haraldsdottir et al. compared outcomes in CRC patients who have deficient MMR due to Lynch syndrome versus sporadic hypermethylation. A total of 143 patients were evaluated and the cancer-specific survival (defined as time from diagnosis to death related to CRC) was the same between the Lynch-associated and sporadic CRC (16).
Methods for testing DNA MMR and MSI
The Association of Molecular Pathology recommends Lynch screening for all new CRC patients, and CRC tumors to be tested for MMR deficiency by immunohistochemistry (IHC) or MSI by polymerase chain reaction (PCR), as well as BRAF V600E MT (12). Thus CRC tissue is usually first tested for loss of MMR proteins by IHC. If there is an absence of an MMR protein, then BRAF V600E MT is checked because Lynch syndrome patients generally have tumors that are BRAF wild-type (WT). In the presence of a BRAF V600E MT, the patient likely has loss of MMR genes secondary to sporadic causes (17). For MSI testing by PCR, the Bethesda guidelines recommend a reference panel of five microsatellites (two mononucleotide loci BAT 25/26; three dinucleotide loci D2S123, D5S346, and D17S250) to ensure reproducibility and standardization. These microsatellite areas are both amplified in the tumor and normal tissue by PCR and their size is measured by capillary electrophoresis. A change in the size of at least two microsatellites in the tumor compared to normal tissue is defined as MSI-H (18). Following this, Promega has developed the MSI analysis system that replaced the dinucleotide markers with mononucleotide markers (NR-21, NR-24, and MONO-27) (19,20). IHC for MMR proteins has comparable results compared PCR testing and a high concordance rate (12). IHC has several advantages compared to PCR testing, one of which is that it can be done on pauci-cellular specimens, is broadly available in most pathology labs and less expensive compared to PCR. However, MSI PCR may be ordered to confirm IHC findings, or if there is high suspicion for MSI-H tumors despite presence of all MMR proteins on IHC. Recently, mutant heat shock protein 110 (HSP110) has been described to be only found in MSI-H tumors (21). Buhard et al. report that there is a high frequency of MTs in a series of thymidine mononucleotide repeats (T17) of HSP110 that leads to mutant HSP110 (22). Thus, they compared testing for HSP110 T17 polymorphism versus MSI testing by PCR (with five mononucleotide repeats that were previously published) to identify MSI-H tumors, and found that sensitivity and specificity of both tests were comparable (21). They propose that testing for HSP110 T17 polymorphism as an additional and more simplified test to detect MSI-H tumors.
Clinical significance of MSI-H cancers
MSI is not only a key component for the pathogenesis of CRC but can also be a biomarker for improved prognosis and predict efficacy of chemotherapy and immunotherapy (21). Patients with MSI-H CRC present at a lower stage of disease at diagnosis, and have improved outcomes when compared to stage specific MSS CRC (23,24). Ribic et al. performed a retrospective evaluation of MSI status from patients who had enrolled on adjuvant chemotherapy trials. Univariate analysis, not controlling for chemotherapy, showed that patients who have MSI-H tumors did better than MSS in general, and patients with stage II and III MSI-H tumors did not benefit from adjuvant 5-fluorouracil (5-FU) chemotherapy (HR =1.07, P=0.80) (24). Conversely, patients with MSS tumors did benefit from 5FU therapy (HR =0.72, P=0.04) (25). However, patients with stage III MSI-H cancers, like MSS cancers, do benefit from adjuvant FOLFOX chemotherapy. A pooled analysis of adjuvant chemotherapy trials evaluated patients with stage III who received FOLFOX alone or in combination with cetuximab, and showed that patients with MSI-H tumors did as well as patients with MSS tumors (BRAF and KRAS WT) and there was no difference in the 3-year disease free survival (26). A large retrospective study evaluating 433 patients with MSI-H tumors who had stage II or III CRC, reported that patients with stage III MSI-H tumors still benefited from adjuvant 5FU and oxaliplatin (FOLFOX) chemotherapy (27). There is preclinical data suggesting that MSI-H tumor cells are resistant to fluoropyrimidines possibly due to higher levels of thymidylate synthase but more sensitive to irinotecan and mitomycin C (14,15,21). Further studies are needed to confirm this in the clinical setting.
Immunotherapy
Immunotherapy has been widely tested and is currently approved for many solid tumors. Interaction of PD-1 on T cells with its ligand PD-L1 promotes an immunosuppressive tumor microenvironment. PD-1 is an immune checkpoint receptor that is located on activated T-cells, B-cells, natural killer (NK) cells and can bind to its ligand PD-L1 that is typically located on tumor or stromal cells (28). Upon binding, the PD-1/PD-L1 axis produces an inhibitory signal that causes T-cell exhaustion and inactivation (29). Blocking this interaction has been shown to reverse T-cell exhaustion and induce tumor regression in diseases such as melanoma, non-small cell lung cancer (NSLC), and renal cell carcinoma. Although initial trials have suggested no role for immunotherapy in patients with CRC, Brahmer et al. showed that a specific subset of patients did benefit. In that phase I study, one patient treated with MDX-1106, a PD-1 inhibitor, had a complete response for more than 21 months. This patient’s tumor was found to have a deficiency in MMR proteins. It is proposed that in MSI-H tumors, there is a significant immunological response that is elicited by neoepitopes due to the increased DNA repair mistakes. MSI-H tumors are hypermutated and express a lot of frameshift peptides which act as neoantigens which elicit an immune response by TILs (30). Thus, when PD-1 is inhibited, the TILs present at the tumor border are activated and attack the tumor.
Le et al. conducted a phase II trial in patients with mCRC with or without MMR deficiency to evaluate the clinical activity of an antibody to programmed death 1 (anti-PD-1) receptor, pembrolizumab (31). In this study there were three different cohorts of patients: (I) deficient MMR in CRC patients; (II) proficient MMR in CRC patients; and (III) deficient MMR in non-CRC patients. The Promega test was utilized to identify MSI-H tumors. The interim published report shows that patients overall tolerated pembrolizumab well with only 17% experiencing grade 3 or 4 toxicity limited to anemia, lymphopenia, diarrhea, bowel obstruction, elevated alanine aminotransferase or hyponatremia. CRC patients who had deficient MMR had a 40% response rate [95% confidence interval (CI), 12 to 74] and the immune related PFS at 20 weeks was 78% (95% CI, 40 to 97). The median PFS and OS were not reached in this group. In contrast, CRC patients with proficient MMR the median PFS was 2.2 months (95% CI, 1.4 to 2.8) and median OS was 5 months (95% CI, 3.0 to not estimable). Additional correlative work to evaluate tumor infiltrating lymphocytes and PD-1 expression at the invasive front of the tumor was also done in this trial. Correlative analysis showed that there was an increase number of CD8+ cells and PD-L1 expression seen at the invasive front of MSI-H tumors. Interestingly, this did not correlate with improvement in PFS or OS but the trial is still ongoing (31).
Potential biomarkers (Table 2)

Full table
TILs
TILs represent the host immune response to cancer cells and the infiltration of TILs may have an impact on the prognosis of CRC patients (32). CD8+ cytotoxic T cells (CTL) are capable of directly killing the tumor cells and CD4+ helper cells (Th) are heterogeneous cytokine-secreting T-cells (33). T-helper type 1 lymphocytes (Th1s) activate CTL, and T-helper type 2 lymphocytes (Th2s) stimulate humoral immunity (34). Regulator T cells (Tregs) can suppress the activity of CTLs by direct cell to cell contact or releasing cytokines such as transforming growth factor-β (TGF-β) or transcription factor forkhead box P3 (FoxP3), which specifically identify Tregs (35). FoxP3 has been reported to be a good prognostic biomarker in CRC (36,37) but conversely associated with poor prognosis in other cancers (38). Katz et al. have reported that the absolute number of Tregs does not correlate with OS or recurrence free survival but if Tregs are increased compared to CD4+/CD8+ cells, it indicates a poorer outcome (39). These mechanisms provide a way for dampening the immune response and allowing expression of ligands, such as PD-L1, to decrease innate antitumor response. PD-1 association with PD-L1 is a negative feedback system, which represses CTLs from killing tumor cells (31,40,41).
In CRC, analyses of immune reaction and TILs have already been explored as a means for tumor classification and as a prognostic biomarker. There has been characterization of TILs with tumor invasion, spread to lymph node, and tumor (TNM) staging system. Pagès et al. demonstrated that the extent of immune reaction at the tumor site is correlated with improved clinical outcome (42). In addition, the authors showed that CD8+ cytotoxic T cell lymphocytes and CD45RO+ memory T cells at the invasive margin of the tumor could determine tumor recurrence and survival in patients with early stage (stage I and II) CRC. Subsequently, Mlecnik et al. showed the relationship between intratumoral immune cell density with degree of tumor extension and frequency of tumor recurrence (43). Based on these factors, an immune score can be calculated. Thus, further studies are needed to see if it is possible to utilize an immune scoring system for metastatic CRC, to determine whether patients will be responsive to immunotherapy.
Checkpoint proteins
It is possible to identify the effects immunotherapy has on the immune cell population in the tumor and around the tumor tissue. As discussed before, in the phase II pembrolizumab study for MSI-H CRC, PD-L1 expression was detected at the invasive front of the tumor, but this has not correlated with improved OS thus far. Checkpoint inhibitors are approved by the US Food and Drug Administration in NSLC, renal cell cancer, and melanoma, thus evaluation of tumor expression of PD-1 and PD-L1 has been mainly in these diseases. In NSCLC, pembrolizumab was shown to have improved OS and PFS in patients with PD-L1 expression in tumor greater than 50% using the Merck proprietary proportion score (44). However, PD-L1 expression itself as a predictive biomarker has conflicting results in the literature. A meta-analysis reviewed a total of 13 immunotherapy trials in NSCLC and showed that there was a statistically significant higher overall response rate in patients who had PD-L1 positive tumors (RR 2.08; 95% CI, 1.49–2.91; P<0.01). The authors concluded that while PD-L1 expression is a reasonable predictive biomarker there is no universal consensus, as there is substantial heterogeneity in the methodology of evaluation and the expression is possibly a dynamic process which changes according to the tumor microenvironment (29). Another study done by Pan et al. was a meta-analysis of nine clinical trials in NSCLC in which high PD-L1 expression was associated with poor tumor differentiation (OR 0.53; 95% CI, 0.39–0.72) and worse OS (HR 1.47; 95% CI, 1.19–1.83) indicating that PD-L1 is a poor prognostic biomarker (45). It is evident that a standard test and grading system is needed for these tumor markers to be meaningful in guiding therapy in all cancers.
Neoantigens
MSI-H tumors have a dense infiltration of intraepithelial CD8+ T-lymphocytes, activated Th1 cells (interferon γ and Th1 transcription factor TBET), and are more prone to local cytotoxic cellular immune response (31,46,47). The association of the MSI-H phenotype with the presence of TILs is explained by the accumulation of frameshift MTs and synthesis of neoantigens thus triggering the host immune system (48). Neoantigens are mutated peptides that arise in the tumor and are not present in the normal genome. With the use of whole-exome RNA sequencing, it has become possible to identify novel neoantigens (49). When there is degradation of neoantigens, it can cause a release of immunogenic neopeptides that is presented by human leukocyte antigen class I (HLA-1) molecules.
Recently, a study by Van Allen et al. evaluated tumor biopsies of patients with metastatic melanoma before and after anti-cytotoxic T lymphocyte-associated protein 4 (anti-CTLA-4) immunotherapy (50). The authors found that patients who had a high number of neoantigens were more likely to respond to anti-CTLA-4 therapy. When trying to evaluate similarities among neoantigens, the authors did not find a single antigen or MT that correlated with clinical benefit among those who responded. Similar to this study, several others have shown that the number of MTs and presence of neoantigens correlates with response to anti-CTLA-4, anti-PD1, and anti-PD-L1 therapies in patients with melanoma, lung cancer and MSI-H CRC (51). This data suggests that there is not a single MT or abnormality which can predict the response to immunotherapy, rather it is the presence of high number of MTs and response by T-cells in the tumor microenvironment. Furthermore, Angelova et al. characterized the immunophenotypes and antigenome (repertoire of tumor antigens) in CRC (52). The authors have shown there are many common germline MTs; however, neoantigens are infrequently shared between patients. A total of 92,028 neoantigens were evaluated based on The Cancer Genome Atlas database and only 4% were shared between two or more patients. In addition, neoantigens were most frequently induced by MTs in KRAS, RNF43 and PIK3CA (52).
Gene MTs
It is now known that the density of TILs and expression of immune related genes may be prognostic and predictive of efficacy of PD-1 and PD-L1 inhibitors; however, the factors that determine a patient’s immune phenotype are unclear (32). For example, it is not known if specific molecular subsets like RAS or BRAF MTs versus WT are associated with high or low immune infiltration (53). Maby et al. showed that there is a relationship between frameshift MTs and TIL subpopulations (54). The authors analyzed 103 MSI-H tumors and found that CD8+ TIL density correlated with number and spectrum of frameshift MTs. Their results also correlated with other small studies (55), which showed that genes ACVR2, TAF1B, TFGBR2, and ASTE1 had the most majority of frameshift MTs in MSI-H CRC. It may be interesting to further explore these gene MTs as biomarkers.
CpG island methylation
DNA methylation of CpG dinucleotide islands in gene promoter regions is a mechanism of silencing genes and leading to genomic instability, which contributes to CRC pathogenesis. Approximately 40% of all CRC patients have the CpG methylation phenotype-high (CIMP-high) phenotype (56). CIMP-high phenotype is associated with CRC in the proximal colon, poorly differentiated histopathologic features, MSI-H, and BRAF MT tumors. However it is not routinely tested in the clinic due to lack of standardization (57). To determine CIMP status in CRC, there are three different promoter panels which are available: (I) classic five-marker panel [MINT1, MINT2, MINT31, CKDN2A (p16) and hMLH1] (58,59); (II) Weisenberger five-marker panel (CACNA1G, IGF2, NEUROG1, RUNX2 and SOCS1) (60); and (III) a combination of the two panels. The classic panel has been associated with predicting clinical outcomes and the Weisenberger panel is better at detecting known clinic-pathological features but worse at predicting outcomes. More recently, another method of identifying CIMP-high tumors is by performing genome-wide DNA methylation analysis by Infinium bead array. Interestingly, CIMP-high does not correlate with stage of tumor but has been associated with a shorter OS (61). Patients with younger onset of disease typically have CIMP-low tumors compared to late onset CRC patients (62). Perea et al. evaluated young and older onset patients according to carcinogenic pathways and found that young onset CIMP-high tumors were associated with a germline MT in MMR gene and late onset CIMP-high CRC was associated with sporadic MSI tumors (56). Loss of expression of methylguanine DNA methyltransferase (MGMT) has been noted in CRC with CIMP-high and MSI-H phenotype (63,64). MGMT hypermethylation has been described in both sporadic and hereditary tumors and been shown to be a predictor for response to alkylating agents such as temozolomide and decarbazine (65). Further studies are needed to see if this will hold true for MSI-H CRC patients.
Conclusions
Advances in tumor characterization of CRC have enabled us to personalize treatment for CRC patients. Currently KRAS, NRAS, and BRAF MT testing are of upmost importance to determine whether patients are eligible for anti-EGFR antibody therapy and/or clinical trials. In addition, DNA MMR and MSI status is now clinically significant to determine whether patients may be eligible for immunotherapy on clinical trials. Better understanding of pathological and genomic features seen in MSI-H CRC will enable us to look for other biomarkers, such as TILs, checkpoint proteins, or other genomic MTs so that we may be able to include eligible patients even with MSS tumors in the future for immunotherapy. More importantly, understanding why MSI-H tumors are responsive to immunotherapy will help us develop better treatment combinations to improve efficacy for all CRC patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- National Cancer Institute. Surveillance, Epidemiology, and End Results Program. SEER stat fact sheets: colon and rectum cancer. Available online: http://www.seer.cancer.gov
- Gatalica Z, Vranic S, Xiu J, et al. High microsatellite instability (MSI-H) colorectal carcinoma: a brief review of predictive biomarkers in the era of personalized medicine. Fam Cancer 2016;15:405-12. [Crossref] [PubMed]
- Sinicrope FA, Okamoto K, Kasi PM, et al. Molecular biomarkers in the personalized treatment of colorectal cancer. Clin Gastroenterol Hepatol 2016;14:651-8. [Crossref] [PubMed]
- Douillard JY, Oliner KS, Siena S, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 2013;369:1023-34. [Crossref] [PubMed]
- Heinemann V, Stintzing S. FOLFIRI with cetuximab or bevacizumab: FIRE-3-authors' reply. Lancet Oncol 2014;15:e583-4. [Crossref] [PubMed]
- Rajagopalan H, Bardelli A, Lengauer C, et al. Tumorigenesis: RAF/RAS oncogenes and mismatch-repair status. Nature 2002;418:934. [Crossref] [PubMed]
- Van Cutsem E, Köhne CH, Hitre E, et al. Cetuximab and chemotherapy as initial treatment for metastatic colorectal cancer. N Engl J Med 2009;360:1408-17. [Crossref] [PubMed]
- Roth AD, Tejpar S, Delorenzi M, et al. Prognostic role of KRAS and BRAF in stage II and III resected colon cancer: results of the translational study on the PETACC-3, EORTC 40993, SAKK 60-00 trial. J Clin Oncol 2010;28:466-74. [Crossref] [PubMed]
- Modrich P. Mechanisms in eukaryotic mismatch repair. J Biol Chem 2006;281:30305-9. [Crossref] [PubMed]
- Stojic L, Brun R, Jiricny J. Mismatch repair and DNA damage signalling. DNA Repair (Amst) 2004;3:1091-101. [Crossref] [PubMed]
- Peltomäki P. Lynch syndrome genes. Fam Cancer 2005;4:227-32. [Crossref] [PubMed]
- Funkhouser WK Jr, Lubin IM, Monzon FA, et al. Relevance, pathogenesis, and testing algorithm for mismatch repair-defective colorectal carcinomas: a report of the association for molecular pathology. J Mol Diagn 2012;14:91-103. [Crossref] [PubMed]
- Veigl ML, Kasturi L, Olechnowicz J, et al. Biallelic inactivation of hMLH1 by epigenetic gene silencing, a novel mechanism causing human MSI cancers. Proc Natl Acad Sci U S A 1998;95:8698-702. [Crossref] [PubMed]
- Devaud N, Gallinger S. Chemotherapy of MMR-deficient colorectal cancer. Fam Cancer 2013;12:301-6. [Crossref] [PubMed]
- Smyrk TC, Watson P, Kaul K, et al. Tumor-infiltrating lymphocytes are a marker for microsatellite instability in colorectal carcinoma. Cancer 2001;91:2417-22. [Crossref] [PubMed]
- Haraldsdottir S, Hampel H, Wu C, et al. Patients with colorectal cancer associated with Lynch syndrome and MLH1 promoter hypermethylation have similar prognoses. Genet Med 2016;18:863-8. [Crossref] [PubMed]
- Peltomäki P. Role of DNA mismatch repair defects in the pathogenesis of human cancer. J Clin Oncol 2003;21:1174-9. [Crossref] [PubMed]
- Berg KD, Glaser CL, Thompson RE, et al. Detection of microsatellite instability by fluorescence multiplex polymerase chain reaction. J Mol Diagn 2000;2:20-8. [Crossref] [PubMed]
- Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 2004;96:261-8. [Crossref] [PubMed]
- Bacher JW, Flanagan LA, Smalley RL, et al. Development of a fluorescent multiplex assay for detection of MSI-High tumors. Dis Markers 2004;20:237-50. [Crossref] [PubMed]
- Hewish M, Lord CJ, Martin SA, et al. Mismatch repair deficient colorectal cancer in the era of personalized treatment. Nat Rev Clin Oncol 2010;7:197-208. [Crossref] [PubMed]
- Buhard O, Lagrange A, Guilloux A, et al. HSP110 T17 simplifies and improves the microsatellite instability testing in patients with colorectal cancer. J Med Genet 2016;53:377-84. [Crossref] [PubMed]
- Goldstein J, Tran B, Ensor J, et al. Multicenter retrospective analysis of metastatic colorectal cancer (CRC) with high-level microsatellite instability (MSI-H). Ann Oncol 2014;25:1032-8. [Crossref] [PubMed]
- Popat S, Hubner R, Houlston RS. Systematic review of microsatellite instability and colorectal cancer prognosis. J Clin Oncol 2005;23:609-18. [Crossref] [PubMed]
- Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med 2003;349:247-57. [Crossref] [PubMed]
- Zaanan A, Shi Q, Taieb J, et al. Analysis of DNA mismatch repair (MMR) and clinical outcome in stage III colon cancers from patients (pts) treated with adjuvant FOLFOX +/- cetuximab in the PETACC8 and NCCTG N0147 adjuvant trials. J Clin Oncol 2015;33:3506.
- Tougeron D, Mouillet G, Trouilloud I, et al. Efficacy of adjuvant chemotherapy in colon cancer with microsatellite instability: a large multicenter AGEO study. J Natl Cancer Inst 2016.108. [PubMed]
- Gandini S, Massi D, Mandalà M. PD-L1 expression in cancer patients receiving anti PD-1/PD-L1 antibodies: A systematic review and meta-analysis. Crit Rev Oncol Hematol 2016;100:88-98. [Crossref] [PubMed]
- Aguiar PN Jr, Santoro IL, Tadokoro H, et al. The role of PD-L1 expression as a predictive biomarker in advanced non-small-cell lung cancer: a network meta-analysis. Immunotherapy 2016;8:479-88. [Crossref] [PubMed]
- Schwitalle Y, Kloor M, Eiermann S, et al. Immune response against frameshift-induced neopeptides in HNPCC patients and healthy HNPCC mutation carriers. Gastroenterology 2008;134:988-97. [Crossref] [PubMed]
- Le DT, Uram JN, Wang H, et al. PD-1 Blockade in Tumors with Mismatch-Repair Deficiency. N Engl J Med 2015;372:2509-20. [Crossref] [PubMed]
- Galon J, Costes A, Sanchez-Cabo F, et al. Type, density, and location of immune cells within human colorectal tumors predict clinical outcome. Science 2006;313:1960-4. [Crossref] [PubMed]
- Nakagawa K, Tanaka K, Homma Y, et al. Low infiltration of peritumoral regulatory T cells predicts worse outcome following resection of colorectal liver metastases. Ann Surg Oncol 2015;22:180-6. [Crossref] [PubMed]
- Yu P, Fu YX. Tumor-infiltrating T lymphocytes: friends or foes? Lab Invest 2006;86:231-45. [Crossref] [PubMed]
- Hori S, Nomura T, Sakaguchi S. Control of regulatory T cell development by the transcription factor Foxp3. Science 2003;299:1057-61. [Crossref] [PubMed]
- Frey DM, Droeser RA, Viehl CT, et al. High frequency of tumor-infiltrating FOXP3(+) regulatory T cells predicts improved survival in mismatch repair-proficient colorectal cancer patients. Int J Cancer 2010;126:2635-43. [PubMed]
- Salama P, Phillips M, Grieu F, et al. Tumor-infiltrating FOXP3+ T regulatory cells show strong prognostic significance in colorectal cancer. J Clin Oncol 2009;27:186-92. [Crossref] [PubMed]
- Gao Q, Qiu SJ, Fan J, et al. Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J Clin Oncol 2007;25:2586-93. [Crossref] [PubMed]
- Katz SC, Bamboat ZM, Maker AV, et al. Regulatory T cell infiltration predicts outcome following resection of colorectal cancer liver metastases. Ann Surg Oncol 2013;20:946-55. [Crossref] [PubMed]
- Ahmadzadeh M, Johnson LA, Heemskerk B, et al. Tumor antigen-specific CD8 T cells infiltrating the tumor express high levels of PD-1 and are functionally impaired. Blood 2009;114:1537-44. [Crossref] [PubMed]
- Baitsch L, Legat A, Barba L, et al. Extended co-expression of inhibitory receptors by human CD8 T-cells depending on differentiation, antigen-specificity and anatomical localization. PLoS One 2012;7:e30852. [Crossref] [PubMed]
- Pagès F, Kirilovsky A, Mlecnik B, et al. In situ cytotoxic and memory T cells predict outcome in patients with early-stage colorectal cancer. J Clin Oncol 2009;27:5944-51. [Crossref] [PubMed]
- Mlecnik B, Tosolini M, Kirilovsky A, et al. Histopathologic-based prognostic factors of colorectal cancers are associated with the state of the local immune reaction. J Clin Oncol 2011;29:610-8. [Crossref] [PubMed]
- Garon EB, Rizvi NA, Hui R, et al. Pembrolizumab for the treatment of non-small-cell lung cancer. N Engl J Med 2015;372:2018-28. [Crossref] [PubMed]
- Pan ZK, Ye F, Wu X, et al. Clinicopathological and prognostic significance of programmed cell death ligand1 (PD-L1) expression in patients with non-small cell lung cancer: a meta-analysis. J Thorac Dis 2015;7:462-70. [PubMed]
- Phillips SM, Banerjea A, Feakins R, et al. Tumour-infiltrating lymphocytes in colorectal cancer with microsatellite instability are activated and cytotoxic. Br J Surg 2004;91:469-75. [Crossref] [PubMed]
- Guidoboni M, Gafà R, Viel A, et al. Microsatellite instability and high content of activated cytotoxic lymphocytes identify colon cancer patients with a favorable prognosis. Am J Pathol 2001;159:297-304. [Crossref] [PubMed]
- Woerner SM, Gebert J, Yuan YP, et al. Systematic identification of genes with coding microsatellites mutated in DNA mismatch repair-deficient cancer cells. Int J Cancer 2001;93:12-9. [Crossref] [PubMed]
- Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science 2015;348:69-74. [Crossref] [PubMed]
- Van Allen EM, Miao D, Schilling B, et al. Genomic correlates of response to CTLA-4 blockade in metastatic melanoma. Science 2015;350:207-11. [Crossref] [PubMed]
- Koster BD, de Gruijl TD, van den Eertwegh AJ. Recent developments and future challenges in immune checkpoint inhibitory cancer treatment. Curr Opin Oncol 2015;27:482-8. [Crossref] [PubMed]
- Angelova M, Charoentong P, Hackl H, et al. Characterization of the immunophenotypes and antigenomes of colorectal cancers reveals distinct tumor escape mechanisms and novel targets for immunotherapy. Genome Biol 2015;16:64. [Crossref] [PubMed]
- Kim H, Nam SW, Rhee H, et al. Different gene expression profiles between microsatellite instability-high and microsatellite stable colorectal carcinomas. Oncogene 2004;23:6218-25. [Crossref] [PubMed]
- Maby P, Tougeron D, Hamieh M, et al. Correlation between density of CD8+ T-cell infiltrate in microsatellite unstable colorectal cancers and frameshift mutations: a rationale for personalized immunotherapy. Cancer Res 2015;75:3446-55. [Crossref] [PubMed]
- Tougeron D, Fauquembergue E, Rouquette A, et al. Tumor-infiltrating lymphocytes in colorectal cancers with microsatellite instability are correlated with the number and spectrum of frameshift mutations. Mod Pathol 2009;22:1186-95. [Crossref] [PubMed]
- Perea J, Rueda D, Canal A, et al. Age at onset should be a major criterion for subclassification of colorectal cancer. J Mol Diagn 2014;16:116-26. [Crossref] [PubMed]
- Silla IO, Rueda D, Rodríguez Y, et al. Early-onset colorectal cancer: a separate subset of colorectal cancer. World J Gastroenterol 2014;20:17288-96. [Crossref] [PubMed]
- Toyota M, Ahuja N, Ohe-Toyota M, et al. CpG island methylator phenotype in colorectal cancer. Proc Natl Acad Sci U S A 1999;96:8681-6. [Crossref] [PubMed]
- Issa JP. CpG island methylator phenotype in cancer. Nat Rev Cancer 2004;4:988-93. [Crossref] [PubMed]
- Weisenberger DJ, Siegmund KD, Campan M, et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet 2006;38:787-93. [Crossref] [PubMed]
- Zong L, Abe M, Ji J, et al. Tracking the correlation between CpG island methylator phenotype and other molecular features and clinicopathological features in human colorectal cancers: a systematic review and meta-analysis. Clin Transl Gastroenterol 2016;7:e151. [Crossref] [PubMed]
- Ballester V, Rashtak S, Boardman L. Clinical and molecular features of young-onset colorectal cancer. World J Gastroenterol 2016;22:1736-44. [Crossref] [PubMed]
- Nazemalhosseini Mojarad E, Kuppen PJ, Aghdaei HA, et al. The CpG island methylator phenotype (CIMP) in colorectal cancer. Gastroenterol Hepatol Bed Bench 2013;6:120-8. [PubMed]
- Zheng CG, Jin C, Ye LC, et al. Clinicopathological significance and potential drug target of O6-methylguanine-DNA methyltransferase in colorectal cancer: a meta-analysis. Tumour Biol 2015;36:5839-48. [Crossref] [PubMed]
- Inno A, Fanetti G, Di Bartolomeo M, et al. Role of MGMT as biomarker in colorectal cancer. World J Clin Cases 2014;2:835-9. [Crossref] [PubMed]


