
A systematic review and meta-analysis of nursing effect of fast-track recovery surgery on patients undergoing total endoscopic resection of esophageal cancer: fast-track recovery surgery vs. nursing care as usual
Highlight box
Key findings
• Fast-track recovery surgery (FTS) care is effective at accelerating patients’ postoperative recovery.
What is known and what is new?
• Esophageal cancer (EC) is the 6th leading cause of cancer-related deaths worldwide, and the morbidity and mortality of EC have continued to increase in recent years. The results of the clinical application of the FTS concept in nursing interventions for EC patients after total endoscopic esophagectomy are unconvincing.
• This study evaluated the nursing effect of the fast-track recovery surgical nursing model on patients with EC after total cavity endoscopic esophagectomy.
What is the implication, and what should change now?
• This model of care needs to be further validated in the future by higher-quality and longer follow-up studies.
Introduction
Esophageal cancer (EC) is the 6th leading cause of cancer-related deaths worldwide, and the morbidity and mortality of EC have continued to increase in recent years (1). It is estimated that China has the world’s highest incidence and mortality rates for EC (1). The number of new EC cases each year in China accounts for more than 1/2 of the world sum, and there are 160,000–200,000 EC-related deaths in China each year (2,3). The pathological types of EC vary greatly across different geographical locations (4). In China, the high prevalence of EC occurs mostly in males aged >40 years, and the ratio of EC is approximately 20:1 between men and women (4). EC is most frequently found in the mid-thoracic segment (52.69–63.33%) and least frequently in the upper thoracic segment (2.80–14.10%) (4). Risk factors for EC include inappropriate dietary habits, nitrosamines, long-term chronic esophageal inflammation, micronutrient deficiencies, and genetic factors (5).
At present, surgery-based multidisciplinary comprehensive treatment is the main treatment of EC. The anatomical position of the esophagus is special, as the esophagus passes longitudinally through the neck, chest and abdomen, and is horizontally adjacent to the trachea and spine. This particular anatomical location complicates the surgical treatment of EC. The surgical approaches for EC currently include the left thoracic approach (Sweet operation), right thoracic approach (McKeown Ivor-Lewis operation) and non-thoracotomy (through the mediastinum and esophageal hiatus). The resection of EC using the right thoracic approach has become the preferred surgical treatment for EC (6,7). Despite continued advances in esophageal surgery, the overall postoperative recurrence and metastasis rates for EC patients remain high, and the overall survival rate for EC patients remains low (8,9). In terms of their long-term prognosis, EC patients may suffer from recurrence and lymph node metastasis, with lymph node metastasis accounting for 21–37.5% of patients (10).
With the standardized treatment of EC and the development of surgical techniques, especially improvements in minimally invasive extraesophageal techniques, thoracic surgeons have begun to pay more and more attention to total lumen esophagectomy (TLE). The advantages of TLE include that it results in less postoperative complications, less organ damage, and can protect the respiratory function of patients. It can also enhance the life quality of patients, and its safety and efficacy have been confirmed in a number of clinical studies (11,12). For instance, Yang et al. (13) described the clinical characteristics, treatment outcomes, and survival of surgical treatment in patients with esophageal cancer in Shanghai Chest Hospital (SCH). They revealed important surgical treatment effects of esophageal cancer patients and contributes to improvement of clinical management and future treatment development (13). However, patients may experience surgical trauma during the operation, which can lead to limited postoperative recovery. Thus, corresponding nursing measures need to be adopted in a timely manner to promote patients’ postoperative recovery (14).
Traditional nursing measures require patients to fast and stay in bed after the operation, which may lead to postoperative malnutrition, and even thrombus, infection, and other complications. As the concept of Fast-track recovery surgery (FTS) has gained acceptance, many different surgical procedures have been adapted to it. FTS mainly includes peri-operative optimization measures for patients, such as preoperative health education, the intraoperative control of infusion volume, postoperative enhanced enteral nutrition, and rehabilitation, which can reduce the physiological and psychological stress reactions caused by surgery (15). A previous case-control study have confirmed that nursing interventions based on the FTS concept can significantly facilitate the postoperative recovery of patients undergoing total endoscopic resection for EC (15). However, the conclusions drawn by different studies are not entirely consistent, and there is considerable variation in the design and evaluation metrics of the various studies. The results of the clinical application of the FTS concept in nursing interventions for EC patients after total endoscopic esophagectomy are unconvincing. Thus, in order to collect related information, we conducted a meta-analysis to evaluate the effectiveness of the nursing intervention of the FTS concept in patients after total endoscopic esophagectomy. We present the following article in accordance with the PRISMA reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-101/rc).
Methods
Sources and retrieval methods for documents
All articles on case-control trials about nursing interventions after total endoscopic esophagectomy published in PUBMED, EMBASE, MEDLINE and Cochrane libraries between January 2010 and May 2022 were searched by computer. The relevant data from the case-control trials in nursing interventions based on the concept of fast-track recovery surgery in patients with EC after total endoscopic esophagectomy were extracted. We searched for the articles using the following keywords: total endoscopic resection; EC; perioperative period; nursing intervention; effect analysis
Fast-track recovery surgical nursing model: On the basis of traditional nursing measures, FTS also mainly includes perioperative optimization measures for patients, such as preoperative health education, intraoperative infusion volume control, postoperative intestinal nutrition enhancement, rehabilitation, etc., which can reduce the physiological and psychological stress reactions caused by surgery.
Inclusion and exclusion criteria
Inclusion criteria
To be eligible for inclusion in this meta-analysis, the articles had to meet the following inclusion criteria: (I) concern a case-control study examining a nursing intervention based on fast-track recovery surgery in patients who had undergone complete endoscopic resection for EC; (II) include subjects who met the diagnostic criteria in the guidelines for the standardized diagnosis and treatment of EC (16), who had their EC diagnoses confirmed by pathological examinations, who had clinical stages of 0–III, who agreed to undergo video-assisted thoracoscopic surgery, who had no contraindications, conscious, and who had no cognitive impairments; (III) include a control group who received a routine nursing intervention, and a study group who received a fast-track recovery surgery concept nursing intervention; and (IV) report on >1 of the following outcome indexes: hospital stay, extubation time, the time out-of-bed activity, exhaust time, Riker Sedation-Agitation Scale (SAS) score (from January 2010 to May 2022), Severity of Dependence Scale (SDS) score and postoperative complications (from January 2010 to May 2022).
Exclusion criteria
Articles were excluded from the meta-analysis if they met any of the following exclusion criteria: (I) did not concern a case-control study; (II) had unavailable data due to insufficient data reports; (III) concerned a repeated study, in which case the most recent research was included; (IV) have study results that did not examine remarkable curative effects; and/or (V) concerned a review of a related article.
Quality evaluation and data extraction
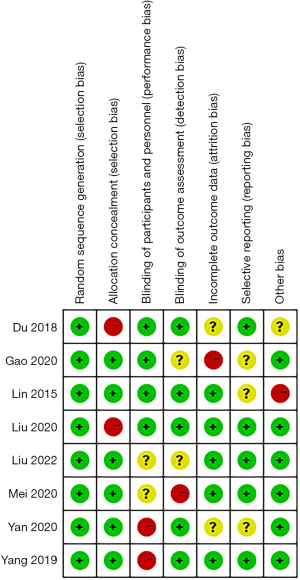
The Cochrane System Review Manual 5.3 (https://training.cochrane.org/) was recommended using a risk-of-bias assessment tool to evaluate the bias risk.
The article screening and data extraction was conducted by 2 researchers independently, who reviewed the articles. Several steps were taken to extract, evaluate, and cross-check the data. Any differences in opinions between the researchers were resolved by a third researcher who assisted them to make a decision. The following information was collected: in the data extraction: (I) basic information; (II) intervention measures (i.e., plan and treatment); (III) outcome data; and (IV) outcome indicators (i.e., hospital stay, extubation time, out-of-bed time, exhaust time, SAS score, SDS score, and postoperative complications). For SAS score and SDS score, they were measured in the included articles.
Cochrane operation procedure: Risk of bias was determined by two reviewers using the Risk of Bias 2 (RoB 2) tool for randomized controlled trials (RCTs). The following bias: selection bias, performance bias, detection bias, attrition bias, reporting bias and other bias were included. Discrepancies were discussed with a third reviewer.
Statistical processing
The meta-analysis was conducted using RevMan5.3 software (https://training.cochrane.org/). The counting data were indexed by the relative risk [odds ratio (OR)], and the measurement data were indexed by the mean difference (MD). Point estimates and 95% confidence intervals (CIs) were provided for each effect. Heterogeneity test and meta-analysis were carried out by means of RevMan 5.3 software. Heterogeneity was assessed using I2 and the χ2 test. The fixed effect model and random effect model were carried out to analyze the data. First, statistical heterogeneity analysis was performed. I2<50% means that no statistical heterogeneity among the studies, or the heterogeneity was small, and the fixed effects model was used to combine the data. I2>50% thought that there was some heterogeneity among the studies, and the random effects model was carried out to combine the effect sizes. If heterogeneity is found, a sensitivity analysis or subgroup analysis is carried out to estimate the source of heterogeneity. If more than 10 studies were included for an outcome indicator, the inverted funnel plot was used to analyze whether there was publication bias. In this study, relative risk (RR) was carried out as the effect scale for dichotomous variables, and mean discrepancy (MD) was used for measurement data with the same unit and measurement methods. If the measurement methods are different or the units are not consistent, standardized mean discrepancy (SMD) is used. 95% confidence interval (CI) is also given, P<0.05, suggesting statistically remarkable discrepancy between the two groups. A P value <0.05 was considered statistically significant. Eggers’s test was used to test for funnel plot asymmetry. The trim-and-fill correction method was used if the P value for the test was <0.1 when adjusting for potential publication bias in the funnel plot.
Results
General information of articles
Based on a reading of the titles and abstracts of the articles, we retrieved 416 of the 1,071 articles from a computer database. Among these, 655 articles were removed as the studies were did not meet the inclusion criteria, and 312 other articles were removed based on a reading of the titles and abstracts. Of the 104 remaining articles, 96 lacked complete data and failed to highlight the main findings; thus, ultimately 8 controlled trials comprising 613 samples were included in the meta-analysis (Figure 1 and Table 1) (17-24). For these studies, rehabilitation includes extubation time, exhaust time, the out-of-bed time for activity, hospitalization time, pulmonary rehabilitation, muscle strength training, aerobic exercise, exercise instruction, nutritional therapy and so on.
Table 1
| First author | Publication year | Sample size | Intervention measures | Research type | Grouping method | Outcome indexes | |||
|---|---|---|---|---|---|---|---|---|---|
| Control group | Research group | Control group | Research group | ||||||
| Gao M (17) | 2020 | 35 | 35 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Random-number table method | (a) (b) (c) (d) (e) | |
| Mei K (18) | 2020 | 47 | 47 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Random-number table method | (a) (b) (d) (e) (f) (g) | |
| Liu Y (19) | 2022 | 34 | 34 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Drawing method | (a) (b) (c) (d) | |
| Du H (20) | 2018 | 39 | 39 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Admission-sequence grouping | (a) (b) (c) (d) | |
| Yan H (21) | 2020 | 40 | 40 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Double-simulation method | (a) (b) (c) (d) (e) | |
| Liu J (22) | 2020 | 35 | 35 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Random grouping | (d) (e) (f) (g) | |
| Yang L (23) | 2019 | 28 | 28 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Different perioperative intervention methods | (f) (g) | |
| Lin Z (24) | 2015 | 49 | 48 | Routine nursing | Concept nursing of fast-track recovery surgery | Prospective study | Different perioperative intervention methods | (a) (b) (d) (e) | |
(a) Extubation time; (b) Exhaust time; (c) Get-out-of-bed time; (d) Hospitalization time; (e) Complication; (f) SAS score; (g) SDS score. SAS, sedation-agitation scale; SDS, severity of dependence scale.
Article evaluation of the methodological quality
The 8 case-control studies included in this meta-analysis. All of the articles detailed the interventions and randomization methods used. Among the 8 trials, none described in detail how many subjects had missed interviews or withdrawn. The quality of the included literature was independently assessed by 2 reviewers using the Risk of Bias 2 (RoB 2) tool. The tool consists of five modules: bias generated during randomization, bias away from established interventions, bias with missing outcome data, bias with outcome measurement, and bias with selective reporting of results. According to the signal problem and path map of each module, the researchers gave bias judgments, and the judgment results were “low risk bias”, “possible risk bias” and “high risk bias”. The overall risk assessment was judged as “Low risk of bias”, “Unclear risk of bias” and “High risk of bias” according to each module. Two people independently evaluate and compare the results. If there is any difference, negotiate to solve the problem. The two researchers compared the bias risk of each module, discussed the differences, reached a consensus, and judged the overall bias risk of the paper based on this. If no consensus can be reached, an evidence-based medical or epidemiological and health statistics professional should be invited to evaluate the article and use this as a conclusion to determine the overall risk of bias. Figures 2,3 illustrate the results of the risk of bias analysis.
Meta-analysis results
Extubation time
An analysis of the extubation time was conducted. According to these studies, extubation time was improved to 1d-2d after Fast-track recovery surgical nursing. The heterogeneity test results were as follows: Chi2=10785.33, degree of freedom (df)=5, P<0.00001, I2=100%. Thus, there was a significant degree of heterogeneity in our study (P<0.05, Figure 4). The extubation time in study group was remarkably shortened than that in the control group.
Exhaust time
A meta-analysis of the exhaust time was conducted. According to these studies, exhaust time was improved to 30–40 h after Fast-track recovery surgical nursing. The heterogeneity test results indicated that there was a significant degree of heterogeneity among the 6 studies (Figure 5). An impressive reduction in the exhaust time was observed in the research group.
The out-of-bed time for activity
A meta-analysis of the time it took patients to leave bed was conducted. According to these studies, the out-of-bed time for activity was improved to around 1.5 d after Fast-track recovery surgical nursing. The heterogeneity test results revealed that there was significant heterogeneity in the included studies. It seems to us that the concept of FTS encourages people to leave bed early; therefore, the out-of-bed time for activity may be used to verify how well FTS was performed. In the study group, the out-of-bed time for activity was significant reduced according to the random-effects model analysis (Figure 6).
Hospitalization time
A meta-analysis was performed of the hospitalization time. According to these studies, hospitalization time was improved to around 8.3 d after Fast-track recovery surgical nursing. The heterogeneity test results showed that the included studies contained significant heterogeneity, and thus a random-effects model was used (Figure 7). The length of hospital stay was significantly shorter for participants in the study group than for those in the control group (P<0.05).
SAS and SDS scores
There were 8 clinical controlled studies comprising 613 samples in this study, and analyses of the SAS and SDS scores were conducted in the relevant paper. The heterogeneity test results were as follows: SAS score: Chi2=146.70, df=2, P<0.00001, I2=99% (Figure 8); and SDS score: Chi2=262.66, df=2, P<0.00001, I2=99% (Figure 9). The study group had extremely low SAS and SDS scores.
Postoperative complications
A meta-analysis was performed on the incidence of postoperative complications. The heterogeneity test results revealed that the included studies showed a significant degree of heterogeneity. There was no significant difference in the incidence of postoperative complications and the incidence of preoperative complications according to the random-effects model analysis (Figure 10).
Publication bias analysis
Funnel plots were drawn based on the patients’ extubation time, exhaust time, get-out-of-bed time, hospitalization time, SAS score, SDS score, and incidence of postoperative complications. A publication bias analysis was performed (see Figures 11-17). Almost all the funnel charts were symmetrical; however, there was a small percentage of asymmetrical funnel charts, which suggest that this study was heterogeneous, and the included articles had a publication bias.
Discussion
EC is a common tumor of the esophagus. It has been reported that the incidence and mortality of EC ranks 4th among all malignant tumors in China in those aged >60 years (25). The etiology of EC has not yet been fully clarified, but it is mostly associated with bad eating habits, long-term smoking, and excessive drinking (26). Most patients with EC are treated with thoracoscopic surgery. Thoracoscopic surgery can reduce the surgical trauma; however, most patients with EC have symptoms, such as malnutrition and low immunity before surgery. Postoperative infections and other complications require appropriate nursing interventions (27). Traditional care mostly requires bed rest and fasting after surgery, which can exacerbate malnutrition, affecting the homeostasis of the patient’s internal environment. Thus, more reasonable and effective nursing interventions are needed for the postoperative rehabilitation of patients with EC.
Accelerated recovery surgery is an evidence-based postoperative management strategy (28). In addition to reducing surgical trauma, pain, and physical and psychological stress, this method can improve the recovery process of patients, shorten hospital stays, and decrease hospital expenses (28). It is a scientific perioperative management program (28). This type of perioperative medical collaboration combines surgery, anesthesiology, nursing, and rehabilitation. Under fast-track surgery, the rapid administration of anesthesia, minimally invasive surgery, adequate analgesic protocols, and the early initiation of postoperative feeding are conducive to safe and rapid patient recovery.
Perioperative medical and nursing interventions can be incorporated into tissue fixation system (TFS) to help patients progress through the perioperative period safely and quickly. Early study has shown that there is no remarkable difference in the joint range of motion, muscle strength, and stability between patients undergoing rehabilitation under the guidance of accelerated rehabilitation programs and conventional rehabilitation programs, but the advantages, such as the shorter rehabilitation time, are remarkable (29). When implementing care under the FTS concept, it is necessary to assess the patient’s situation before the implementation of the intervention and to develop specific measures to ensure the relevance and effectiveness of the nursing intervention. Nursing intervention can minimize the discomfort of patients, relieve their negative emotions, improve their physical and mental levels, and promote the recovery of patients.
In this study, there were 8 case-control studies comprising 613 samples. A meta-analysis was performed of the extubation time, exhaust time, out-of-bed time for activity, and hospitalization time. Compared to the control group, the extubation time, exhaustion time, and time spent in the hospital were all remarkably shorter in the study group than that in the control group. This may be due to a number of reasons. First, rapid recovery programs shorten the duration of preoperative water fasting without bowel preparation and reduce dehydration and hypoglycemia caused by prolonged water fasting. The stimulation of gastrointestinal function through early bedtime activities and nutritional support also promotes deflation and reduces surgical stress. Second, adequate nursing preparation allows for the standardization of the nursing protocol. Third, the patient’s immune system is boosted to shorten the recovery time so that the catheter can be removed as soon as possible (30,31). Fourth, the application of the surgical concept of rapid recovery also speeds up the patient’s postoperative recovery, which is the aim of implementing this model of care. It also reduces medical costs, eases the financial burden on patients, and establishes a good doctor-patient relationship, which is the most obvious difference between the rapid recovery care model and the traditional care model.
The concept of rapid recovery has an important place in perioperative health guidance. Medical staff inform the patient of the diagnosis, treatment, and precautions before the procedure. These basic practices of care can also alleviate patient preoperative stress and improve compliance with treatment. A recent study found that effective psychological counselling can relieve subjective symptoms and anxiety, improve patients’ tolerance of surgery and diminish their postoperative stress, thereby decreasing the risk of complications and speeding up recovery (32). In addition, effective psychological care can reduce the patient’s sympathetic nerve excitation and speed up the recovery of gastrointestinal function. According to the meta-analysis, the study group had significantly lower SAS and SDS scores compared with control group. The concept of rapid recovery care is recommended for patients undergoing total thoracic laparoscopic surgery to alleviate anxiety and depression through optimized clinical care measures.
Under the rapid recovery surgical concept of care, the recovery process of patients can be accelerated. The traditional model of healthcare is disease centered and pays little attention to the patient’s subjective feelings and psychological wellbeing. Conversely, the fast-track recovery surgery concept of nursing is patient centered and focuses on the patient’s physical health and psychological wellbeing. The relationship between psychological wellbeing and disease recovery is balanced, thereby reducing the patient’s negative emotions.
The results of the meta-analysis suggest that the nursing intervention of rapid recovery had no significant effect on postoperative complications in patients undergoing total thoraco-laparoscopic EC surgery. The reason for this may be the short observation period in some of the studies included in this meta-analysis. The follow-up observation of postoperative complications is a long-term process. Accelerated rehabilitation surgery may be effective at reducing postoperative complications in patients during the long-term follow-up, but the actual effect still needs to be confirmed by a large number of studies.
Several case-control studies have demonstrated that nursing interventions based on the FTS concept can significantly promote postoperative recovery in patients undergoing EC total endoscopic resection (15). However, the conclusions of different studies are not completely consistent, and there are considerable differences in the design and evaluation indicators of different studies (33,34). The clinical application of FTS concept in nursing intervention of EC patients after esophagoendoscopic total resection is not convincing. Therefore, in order to collect relevant information, we conducted a meta-analysis to evaluate the effectiveness of the FTS concept in patient care interventions after total endoscopic esophagotomy.
This study had a number of limitations. Notably, only a small number of articles were included in the meta-analysis, and the heterogeneity was not analyzed in great detail in the subgroups. In addition, the analysis of the outcomes in terms of patient prognosis had some limitations due to the inconsistent follow-up times across the included studies.
Conclusions
FTS care is effective at accelerating postoperative recovery. It also remarkably reduces the length of hospital stay, eases the financial burden, and relieves negative emotions without increasing the risk of postoperative complications in EC patients. This model of care should be replicated in clinical practice, and higher-quality studies with longer follow-up periods need to be conducted in the future to further validate our findings.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-101/rc
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-101/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-101/coif). YL reports that she is employed by R&G PharmaStudies Co., Ltd. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ponte Neto FL, de Moura DTH, Sagae VMT, et al. Endoscopic resection of esophageal and gastric submucosal tumors from the muscularis propria layer: submucosal tunneling endoscopic resection versus endoscopic submucosal excavation: A systematic review and meta-analysis. Surg Endosc 2021;35:6413-26. [Crossref] [PubMed]
- Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Zhou M, Wang X, Hu J, et al. Geographical distribution characteristics of major malignant tumor deaths in China from 2004 to 2005. Chinese Journal of Preventive Medicine 2010;303-8. [PubMed]
- Kamarajah SK, Bundred J, Spence G, et al. Critical Appraisal of the Impact of Oesophageal Stents in the Management of Oesophageal Anastomotic Leaks and Benign Oesophageal Perforations: An Updated Systematic Review. World J Surg 2020;44:1173-89. [Crossref] [PubMed]
- Jiao X, Lu Z. Progress in clinical treatment of EC in 2021. Electronic Journal of Comprehensive Oncology Therapy 2022;8:61-71.
- Liu T, Wu J. Progress of surgical approach for EC. Snake Will 2021;33:349-50.
- Uhlenhopp DJ, Then EO, Sunkara T, et al. Epidemiology of EC: update in global trends, etiology and risk factors. Clin J Gastroenterol 2020;13:1010-21. [Crossref] [PubMed]
- Musa IH, Musa TH, Musa HH, et al. EC epidemiology, diagnosis, and management in Sudan - A review. Med J Malaysia 2021;76:691-7. [PubMed]
- Liu B, Qiu ML, Feng Z, et al. Clinical application and analysis of single-port laparoscopic and thoracoscopic McKeown esophagectomy for EC. Zhonghua Yi Xue Za Zhi 2021;101:2316-21. [PubMed]
- Wang WP, Ni PZ, Yang JL, et al. Esophagectomy after endoscopic submucosal dissection for esophageal carcinoma. J Thorac Dis 2018;10:3253-61. [Crossref] [PubMed]
- Mönig S, Chevallay M, Niclauss N, et al. Early EC: the significance of surgery, endoscopy, and chemoradiation. Ann N Y Acad Sci 2018;1434:115-23. [Crossref] [PubMed]
- Yang Y, Liu Z, Sun Y, et al. Clinical characteristics and survival of esophageal cancer patients: annual report of the surgical treatment in Shanghai Chest Hospital, 2016. J Thorac Dis 2022;14:4966-82. [Crossref] [PubMed]
- Li G. Evaluation of the effect of nursing safety management in clinical nursing of EC surgery. Chinese Medicine and Clinic 2021;21:1244-6.
- Chen L, Sun L, Lang Y, et al. Fast-track surgery improves postoperative clinical recovery and cellular and humoral immunity after esophagectomy for esophageal cancer. BMC Cancer 2016;16:449. [Crossref] [PubMed]
- EC Professional Committee of China Anti-Cancer Association. Guidelines for standardized diagnosis and treatment of EC. China Union Medical College Press, 2013.
- Gao M, Yang Y, Jing X. The effect of rapid rehabilitation concept on pulmonary function in patients with EC after total thoracoscopic laparoscopic surgery. Chinese Oncology Clinic and Rehabilitation 2020;27:1116-9.
- Mei K. Application of nursing intervention based on the concept of rapid rehabilitation surgery in patients undergoing thoracic laparoscopic resection of EC. Heilongjiang Medical Science 2020;43:142-3.
- Liu Y. Effect of nursing based on FTS concept on rehabilitation of elderly patients with EC after thoracoscopic surgery. Health standard management in China 2022;13:148-52.
- Du H. Effect of FTS nursing intervention on rehabilitation and incidence of pulmonary infection in elderly patients with EC after thoracoscopic surgery. Food and Medicine in the Capital 2018;25:143.
- Yan H, Li S. To study the effect of nursing intervention of rapid rehabilitation surgery on thoracoscopic surgery in elderly patients with EC. Health Must Read 2020:129-30.
- Liu J, Su S, Ouyang L. Application of rapid rehabilitation surgical nursing in thoracoscopic radical resection of EC. Diet and Health Care 2020;7:122-3.
- Yang L. Effect of perioperative accelerated rehabilitation surgical nursing on patients with thoracoscopic EC. Chinese Health Care and Nutrition 2019;29:31-2.
- Lin Z, Yao X, Wu G. Application of the concept of rapid rehabilitation surgery in perioperative nursing care of patients undergoing thoracic laparoscopic esophagectomy. Chinese Journal of practical Nursing 2015;31:580-2.
- Zheng Y, Yang H, Wu Q, et al. Tim-3 expression on T cell surface of patients with EC and its clinical significance. Chinese Journal of Oncology Biotherapy 2019;26:312-6.
- Wang H, Liu X, Lei Y, et al. Advances in metabonomics of biomarkers related to EC. Chinese Journal of Cancer Prevention and Treatment 2022;29:1080-6.
- Qiu J, Liu Y, Liu T. Effect of early nutritional nursing on immune function and nutritional status of patients after radical resection of EC. Jilin Medicine 2022;43:271-3.
- Tang Y, Liu P, Gao J, et al. Effect of accelerated rehabilitation surgery on postoperative rapid recovery, stress response and complications in patients with laryngeal carcinoma. Journal of Clinical and Pathology 2022;42:1885-91.
- Wang Q. Accelerate the effect of the concept of rehabilitation surgery in tumor surgery. Enterprise Health in Urban and Rural Areas of China 2022;37:178-180.
- Liu L, Yin Z, Wang X, et al. Application and progress of accelerated rehabilitation surgery in perioperative period of EC. Chinese Journal of Thoracic and Cardiovascular Surgery 2020;27:840-4.
- Yoshida T, Hashimoto S, Mizuno KI, et al. Advanced squamous cell carcinoma in an asymptomatic, large, epiphrenic esophageal diverticulum. Clin J Gastroenterol 2020;13:477-82. [Crossref] [PubMed]
- Gao RY, Gan RY, Huang JL, et al. The influence of family support during endoscopic submucosal dissection on patient's anxiety. Front Public Health 2022;10:992018. [Crossref] [PubMed]
- Triantafyllou T, Olson MT, Theodorou D, et al. Enhanced recovery pathways vs standard care pathways in esophageal cancer surgery: systematic review and meta-analysis. Esophagus 2020;17:100-12. [Crossref] [PubMed]
- Puccetti F, Wijnhoven BPL, Kuppusamy M, et al. Impact of standardized clinical pathways on esophagectomy: a systematic review and meta-analysis. Dis Esophagus 2022;35:doab027. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


















