
Evaluation of the up-to-7 criterion for determining the treatment of hepatocellular carcinoma in Barcelona Clinic Liver Cancer stage B: a single-center retrospective cohort study
Highlight box
Key findings
• Hepatectomy may be associated with better survival than TACE in patients with BCLC-B HCC who meet the up-to-7 criterion, but this criterion is not a strict indication for deciding whether to treat patients with BCLC-B surgically. Tumor number, strongly affects the prognosis of BCLC-B patients after hepatectomy.
What is known and what is new?
• European studies have recommended TACE for patients with BCLC-B HCC who met the up-to-7 criterion, Japanese study has recommended hepatectomy for such patients.
• Hepatectomy may be the best primary treatment for patients with BCLC-B HCC who meet up-to-7 criterion, but this criterion should not serve as a deciding factor in determining whether to treat patients with BCLC-B surgically.
What is the implication, and what should change now?
• Up-to-7 criterion is not a strict indication for deciding whether to treat patients with BCLC-B surgically. Tumor number, but not tumor size, strongly affects the prognosis of BCLC-B patients after hepatectomy. We suggest that the criterion should be extended in the treatment of BCLC-B patients.
Introduction
Hepatocellular carcinoma (HCC) is the third-leading cause of death from solid tumors worldwide (1). The Barcelona Clinic Liver Cancer (BCLC) system recommends surgery for patients in stages 0 and A, and transcatheter arterial chemoembolization (TACE) or systemic treatment for patients in the intermediate and late stages (2,3). Hepatectomy is recommended for patients who meet the Milan criterion (i.e., those with a single tumor with a diameter ≤5 cm, of those with <3 tumors that each have a maximum diameter ≤3 cm), and can improve patient survival (4,5). However, due to the strictness of the Milan criterion, some clinicians have proposed an alternative up-to-7 criterion (6). Under the up-to-7 criterion, HCC can be treated by hepatectomy if the sum of the number of tumors and the maximum tumor diameter (cm) is 7 or below. At present, it is considered that the factors influence survival in the surgical treatment of HCC are: tumor size, tumor number, tumor site, tumor envelope integrity, microvascular invasion (MVI) (7-12). Up-to-seven criterion is established based on the number of tumors and tumor diameter. Patients who meet the up-to-seven criterion have fewer tumor numbers, smaller tumor diameters, and are relatively early in the clinical stage, so it is speculated that surgical treatment in these patients may be more effective than TACE. However, studies have made conflicting recommendations about whether patients with Barcelona Clinic Liver Cancer stage B (BCLC-B) disease who meet the up-to-7 criterion should undergo TACE or hepatectomy. European study (13) has recommended TACE for patients with BCLC-B HCC who met the up-to-7 criterion, while Japanese study (14) has recommended hepatectomy for such patients. Thus, the recommended treatment for such patients is unclear. In stage B disease, liver function and tumor load vary greatly among patients and the effect of TACE treatment is highly variable. Notably, in patients with stage B disease who exceed the up-to-7 criterion, TACE may harm liver reserve function and thus worsen their prognosis (15).
In this study, we retrospectively compared the efficacy of surgical treatment or TACE among patients whose HCC was in BCLC-B and who met the up-to-7 criterion. We also compared the post-surgical outcomes between patients who met or exceeded the up-to-7 criterion. As the criterion takes into account the number and diameter of tumors, we compared the relative effects of these 2 parameters on post-surgical outcomes. We present the following article in accordance with the STROBE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-69/rc).
Methods
Patients
The clinical records of 340 patients with HCC in BCLC-B who treated with hepatectomy or TACE at the Department of Hepatobiliary, Pancreatic and Splenic Surgery at Guangxi Medical University Cancer Hospital between November 2013–October 2019 were retrospectively collected, and the number of patients determined the sample size.
Patients were enrolled in this study if they underwent a first-time radical hepatectomy or TACE for HCC, if their HCC was diagnosed histologically or by imaging techniques [magnetic resonance imaging and/or triphasic computed tomography (CT)] according to the available European Association for the Study of the Liver (EASL) guidelines version, and if their recorded clinical data were complete. Patients were excluded from this study if they underwent preoperative transhepatic artery catheter chemoembolization, radiotherapy, or chemotherapy, if they died perioperatively, if their HCC recurred or required re-operation, and if their clinical data were otherwise incomplete.
The study was approved by board of Ethics Committee of Guangxi Medical University Cancer Hospital (No. LW2022030) and informed consent was taken from all the patients. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Treatments
The surgical patients underwent radical hepatectomy, depending on the tumor size and location. Whenever feasible, anatomic resections were preferred. The TACE patients underwent transhepatic arterial chemoembolization via femoral artery puncture.
Data collection
We retrospectively extracted the following data from the patients’ medical records: age, sex, alpha-fetoprotein (AFP), prothrombin time, total bilirubin, albumin, alanine transaminase (ALT), aspartate aminotransferase (AST), the number of tumors, tumor location, the integrity of tumor envelope, hepatitis B surface antigen (HBsAg), the presence or absence of cirrhosis, and MVI.
OS and PFS were compared between patients who met the up-to-7 criterion and who underwent either hepatectomy or TACE. OS and recurrence time were also compared between the patients who were treated with hepatectomy and who either met or exceeded the up-to-7 criterion. To evaluate whether the up-to-seven criteria can be used as an indication for choosing surgery in patients with BCLC-B HCC, we extended the range of the sum of the number of tumors and the maximum diameter of the tumor, i.e., up-to-8, up-to-9, up-to-10, up-to-12, etc., to investigate the survival prognosis of patients with BCLC-B HCC who underwent surgery within the range of our hypothesized criterion. Based on the up-to-seven criterion, which was established by two dimensions of tumor numbers and maximum tumor diameter, we performed a further extension to investigate whether tumor numbers and tumor diameter affect the survival prognosis of patients undergoing surgery in BCLC-B. Univariate and multivariate COX risk regression analyses were applied to assess independent risk factors affecting overall survival in patients meeting up-to-seven criteria, and independent risk factors for overall survival in patients undergoing BCLC-B surgery were also assessed.
Follow-up
The outcomes of interest were overall survival (OS), progression-free survival (PFS) and recurrence time. OS was defined as the interval from the patient’s first surgery until death or last follow-up. PFS was defined as the interval from the patient’s first surgery until tumor progression or last follow-up. Recurrence time was defined as the interval from first surgery until tumor progression or last follow-up. In all cases, censored data were obtained for those lost to follow-up. The last follow-up date in this study was October 31, 2022.
In this study, the post-surgical follow-up was conducted by extracting the relevant data from the inpatient medical records, outpatient medical records and by contacting the patients or their families by telephone.
Statistical analysis
The data were analyzed using SPSS 25.0 (IBM, Chicago, IL, USA). A 2-sided P value <0.05 was considered statistically significant. The inter-group differences in the clinicodemographic data were assessed for significance using the chi-squared test. The overall survival, progression-free survival and recurrence rates were calculated using the Kaplan-Meier method, and the inter-group differences were assessed using the log rank test. The risk factors for mortality were identified by a Univariate Cox regression, and the factors with P values <0.05 in that analysis were further explored in the multivariate Cox regression analysis.
Results
A total of 340 patients with BCLC-B HCC were enrolled in this study after screening according to the inclusion and exclusion criterion. Among the patients, 285 underwent hepatectomy only and 55 underwent TACE only. Of the 285 HCC patients who underwent hepatectomy, 108 met the “up-to-7 criterion” and 177 exceeded the up-to-7 criterion. All the patients in the TACE group met the “up-to-7 criterion”.
Comparison of outcomes after hepatectomy or TACE in patients who met the up-to-7 criterion
Among the patients who met the up-to-7 criterion, those who underwent hepatectomy or TACE differed significantly in terms of albumin, total bilirubin, the number of tumors, and the tumor site (Table 1).
Table 1
| Characteristic | Hepatectomy group (n=108) | TACE group (n=55) | P value |
|---|---|---|---|
| Age (years) | 0.183 | ||
| >50 | 61 | 37 | |
| ≤50 | 47 | 18 | |
| Sex | 0.761 | ||
| Male | 96 | 48 | |
| Female | 12 | 7 | |
| Albumin (g/L) | <0.001 | ||
| >35 | 92 | 33 | |
| ≤35 | 16 | 22 | |
| ALT (U/L) | 0.569 | ||
| >40 | 46 | 26 | |
| ≤40 | 62 | 29 | |
| AST (U/L) | 0.152 | ||
| >40 | 54 | 34 | |
| ≤40 | 54 | 21 | |
| AFP (ng/mL) | 0.084 | ||
| >400 | 40 | 13 | |
| ≤400 | 68 | 42 | |
| Cirrhosis | 0.966 | ||
| (–) | 14 | 7 | |
| (+) | 94 | 48 | |
| HBsAg | 0.591 | ||
| (+) | 99 | 49 | |
| (–) | 9 | 6 | |
| Number of tumors | 0.005 | ||
| >3 | 4 | 9 | |
| ≤3 | 104 | 46 | |
| Prothrombin time (s) | 0.061 | ||
| >13 | 50 | 34 | |
| ≤13 | 58 | 21 | |
| Total bilirubin (μmol/L) | 0.003 | ||
| >20 | 14 | 18 | |
| ≤20 | 94 | 37 | |
| Tumor site | 0.007 | ||
| Single lobe of liver | 71 | 24 | |
| Both lobes of liver | 37 | 31 |
AFP, alpha-fetoprotein; ALT, alanine transaminase; AST, aspartate aminotransferase; TACE, transcatheter arterial chemoembolization.
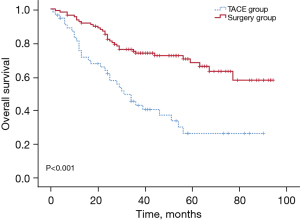
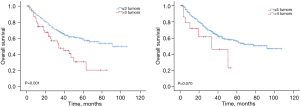
The study was followed up until October 2022, the median OS of the TACE group was 31.0 months, and the median OS of the hepatectomy group was prolonged compared to that of the TACE group, the median OS was approximately 95.0 months until the last follow-up. The OS rates were significantly higher in the hepatectomy group than the TACE group at 1 year (92.6% vs. 75.2%), 2 years (82.0% vs. 61.6%), and 3 years (73.8% vs. 42.8%) (P<0.05) (Figure 1).
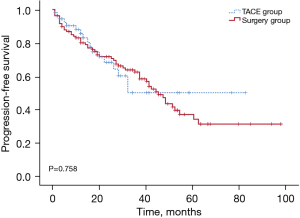
The median PFS of the TACE group was 45.0 months and that of the hepatectomy group was 50.0 months, but the difference between the 2 groups was not significant. Similarly, the PFS rates tended to be higher in the hepatectomy group than the TACE group at 1 year (80.1% vs. 85.7%), 2 years (71.8% vs. 68.4%), and 3 years (62.7% vs. 50.3%), but the differences were not significant (P>0.05) (Figure 2).
The Univariate Cox regression analysis revealed that the following variables were significantly related to OS: albumin, hepatitis B, prothrombin time, and tumor site. The multivariate Cox regression analysis of these variables identified albumin, prothrombin time, and tumor site as independent risk factors for mortality (Table 2).
Table 2
| Variable | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| AFP (ng/mL) | 1.103 (0.666–1.828) | 0.703 | |||
| Albumin (g/L) | 2.174 (1.282–3.687) | 0.004 | 2.147 (1.263–3.649) | 0.005 | |
| ALT (U/L) | 0.851 (0.523–1.385) | 0.517 | |||
| AST (U/L) | 1.293 (0.797–2.097) | 0.299 | |||
| Cirrhosis | 2.615 (0.951–7.188) | 0.062 | |||
| HBsAg | 0.457 (0.225–0.928) | 0.030 | 0.547 (0.264–1.332) | 0.104 | |
| Number of tumors | 1.767 (0.806–3.874) | 0.155 | |||
| Prothrombin time (s) | 1.780 (1.084–2.923) | 0.023 | 1.708 (1.026–2.842) | 0.039 | |
| Sex | 0.706 (0.305–1.633) | 0.416 | |||
| Total bilirubin (μmol/L) | 1.232 (0.681–2.227) | 0.490 | |||
| Tumor site | 1.664 (1.030–2.688) | 0.037 | 1.640 (1.014–2.652) | 0.044 | |
AFP, alpha-fetoprotein; ALT, alanine transaminase; AST, aspartate aminotransferase; CI, confidence interval; HR, hazard ratio.
Comparison of post-hepatectomy outcomes between patients who met or exceeded the up-to-7 criterion
Among the patients who underwent hepatectomy, those who met the up-to-7 criterion differed significantly to those who exceeded it in terms of AFP, intraoperative bleeding, MVI, the number of tumors, and the integrity of tumor envelope (Table 3).
Table 3
| Characteristic | Met criterion (n=108) | Exceeded criterion (n=177) | P value |
|---|---|---|---|
| Age (years) | 0.116 | ||
| >50 | 61 | 83 | |
| ≤50 | 47 | 94 | |
| Sex | 0.847 | ||
| Male | 96 | 156 | |
| Female | 12 | 21 | |
| Albumin (g/L) | 0.164 | ||
| >35 | 92 | 139 | |
| ≤35 | 16 | 38 | |
| ALT(U/L) | 0.807 | ||
| >40 | 46 | 78 | |
| ≤40 | 62 | 99 | |
| AST(U/L) | 0.058 | ||
| >40 | 54 | 107 | |
| ≤40 | 54 | 70 | |
| AFP (ng/mL) | 0.008 | ||
| >400 | 40 | 94 | |
| ≤400 | 68 | 83 | |
| Cirrhosis | 0.593 | ||
| (–) | 14 | 27 | |
| (+) | 94 | 150 | |
| HBsAg | 0.143 | ||
| (+) | 99 | 152 | |
| (–) | 9 | 25 | |
| Intraoperative bleeding (mL) | 0.042 | ||
| ≥500 | 19 | 50 | |
| <500 | 89 | 127 | |
| MVI | 0.008 | ||
| (–) | 67 | 81 | |
| (+) | 41 | 96 | |
| Number of tumors | <0.001 | ||
| >3 | 4 | 44 | |
| ≤3 | 104 | 133 | |
| Prothrombin time (s) | 0.073 | ||
| >13 | 50 | 63 | |
| ≤13 | 58 | 114 | |
| Total bilirubin (µmol/L) | 0.366 | ||
| >20 | 14 | 30 | |
| ≤20 | 94 | 147 | |
| Tumor envelope | 0.036 | ||
| Complete | 84 | 117 | |
| Incomplete | 24 | 60 | |
| Tumor site | 0.819 | ||
| Single lobes of the liver | 71 | 114 | |
| Both lobes of the liver | 37 | 63 |
Values are n, unless otherwise noted. AFP, alpha-fetoprotein; ALT, alanine transaminase; AST, aspartate aminotransferase; MVI, microvascular invasion.
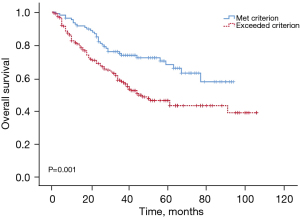
The study was followed up until October 2022, in terms of the median OS, the median OS of the exceeded the up-to-7 criterion was 45.0 months, and the median OS of the met up-to-7 criterion group was prolonged compared to that of the exceeded the up-to-7 criterion group, the median OS was approximately 95.0 months until the last follow-up. The patients who met the up-to-7 criterion had significantly higher OS rates at 1 year (92.6% vs. 81.3%), 2 years (82.0% vs. 68.8%), and 3 years (73.8% vs. 57.9%) (P<0.05) (Figure 3).
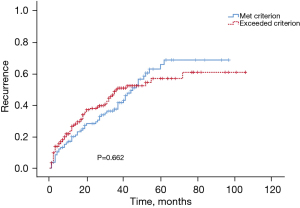
Recurrence did not differ significantly between the patients who met or exceeded the criterion, both in terms of the median time to recurrence (45.0 vs. 37.0 months) and in terms of the recurrence rates at 1 year (19.9% vs. 26.4%), 2 years (28.2% vs. 37.7%), or 3 years (37.3% vs. 49.5%) (P>0.05) (Figure 4).
The Univariate Cox regression analysis showed that AST, chronic infection with hepatitis B virus, the number of tumors, intraoperative bleeding, and MVI were significantly related to OS. The multivariate Cox regression analysis of these factors identified AST, the number of tumors, intraoperative bleeding and MVI as independent risk factors of mortality (Table 4).
Table 4
| Variable | Univariate analysis | Multivariate analysis | |||
|---|---|---|---|---|---|
| HR (95% CI) | P value | HR (95% CI) | P value | ||
| AFP (ng/mL) | 1.276 (0.888–1.835) | 0.188 | |||
| Albumin (g/L) | 1.159 (0.733–1.833) | 0.527 | |||
| ALT (U/L) | 1.274 (0.887–1.831) | 0.190 | |||
| AST (U/L) | 1.772 (1.212–2.591) | 0.003 | 1.492 (1.006–2.212) | 0.047 | |
| Cirrhosis | 1.565 (0.861–2.844) | 0.142 | |||
| HBsAg | 0.577 (0.352–0.943) | 0.028 | 0.632 (0.385–1.040) | 0.071 | |
| Number of tumors | 1.989 (1.289–3.068) | 0.002 | 1.832 (1.181–2.844) | 0.007 | |
| Prothrombin time (s) | 1.042 (0.719–1.510) | 0.830 | |||
| Sex | 0.841 (0.472–1.497) | 0.555 | |||
| Total bilirubin (µmol/L) | 1.092 (0.668–1.786) | 0.725 | |||
| Intraoperative bleeding (mL) | 1.945 (1.312–2.881) | 0.001 | 1.666 (1.110–2.502) | 0.014 | |
| Tumor site | 1.077 (0.740–1.569) | 0.698 | |||
| MVI | 1.942 (1.345–2.802) | <0.001 | 1.799 (1.242–2.606) | 0.002 | |
| Tumor envelope | 0.876 (0.592–1.298) | 0.510 | |||
AFP, alpha-fetoprotein; ALT, alanine transaminase; AST, aspartate aminotransferase; CI, confidence interval; HR, hazard ratio; MVI, microvascular invasion.
Relative influence of the tumor number and size on survival after hepatectomy
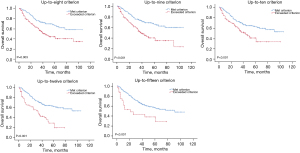
As the up-to-7 criterion takes into account both tumor number and size, we examined the relative influence of each of these 2 factors on the post-surgery survival of the patients. OS was significantly better in patients with ≤3 tumors than those with >3 tumors in terms of both median OS (91.0 vs. 34.0 months) or OS rates at 1 year (87.9% vs. 74.5%), 2 years (76.2% vs. 62.1%), and 3 years (67.1% vs. 47.7%) (P<0.05). Conversely, OS did not differ significantly between patients with ≤4 or >4 tumors (P>0.05) (Figure 5).
To investigate the influence of tumor size on OS, we extended the tumor size in the patients with ≤3 tumors and stratified them based on whether the sum of the tumor number and the largest tumor diameter satisfied the criterion from “up-to-8” to “up-to-15”. In all cases, OS was significantly higher among patients who met the criterion than among those who exceeded it (P<0.05) (Figure 6).
Discussion
Our findings suggest that if HCC patient in BCLC-B meets the up-to-7 criterion, that patient is likely to benefit more from hepatectomy than TACE, and that if a patient exceeds the up-to-7 criterion, surgery should not automatically be excluded, especially if that patient is chronically infected with the hepatitis B virus. Among patients with stage B disease, the tumor number appears to influence the post-surgery prognosis much more than the tumor size.
The BCLC system, which is widely accepted for HCC staging and the treatment selection (16), does not recommend hepatectomy for stage B disease patients. However, several studies have suggested that potentially curative treatments, such as resection, can be safe and effective for stage B disease patients (17-19). However, the use of TACE in BCLC-B patients has been questioned in recent years (20). The BCLC system was developed based on an analysis of patients in which HCC was predominantly related to chronic infection with the hepatitis C virus. In China, HCC is predominantly related to chronic infection with the hepatitis B virus, and often co-occurs with cirrhosis. A previous study showed that many patients with stage B disease who meet the up-to-7 criterion are treated with hepatectomy, which may lead to surprising improvements in OS (17).
The difficulty of hepatectomy depends on several factors, including the tumor numbers, size, and location (21); however, our results suggest that the number of tumors is the main factor affecting the post-hepatectomy survival of HCC patients in BCLC-B. Similarly, a previous study of patients with HCC who underwent surgery showed that the number of tumors was significantly associated with the prognosis of patients with HCC, the 5-year survival rate of BCLC-B patients with 2 or 3 tumors is 52.3%, while the 5-year postoperative survival rate is only 29.0% in patients with more than 4 tumors (22). As the number of tumors increases, the risk of intrahepatic metastasis increases, which can reduce treatment efficacy. Based on a consideration of our present findings, it appears that patients with stage B disease who have ≤3 tumors may achieve better survival after surgery than the patients who have >3 tumors.
In the analysis of the factors affecting survival prognosis, the tumor site was a risk factor affecting the prognosis of the patients who met the up-to-7 criterion, those who underwent hepatectomy or TACE. As the growth site of the tumor varies, the recurrence rate is relatively high if the tumor is not in the same liver lobe, the choice of surgery (e.g., hemi-hepatectomy, hepatic segmentectomy, and local resection of tumor) varies, and the choice of surgery will have a different effect on the prognosis of patients. The number of tumors and MVI were independent risk factors for postoperative survival in the surgical group of the patients who met or exceeded the up-to-7 criterion. The number of tumors is one of the most important factors affecting patient prognosis. A previous study showed that the recurrence rate after surgery in patients with >3 tumors was significantly higher than that in patients with 2 to 3 tumors or a single large tumor (23). Another study reported a higher risk of postoperative recurrence in patients with HCC with >4 tumors (24). MVI is a major predictor of HCC prognosis and is associated with a more advanced tumor stage, disease progression, local invasion, and distant metastasis, MVI also increases the risk of postoperative recurrence and metastasis in patients with HCC (25-27), and MVI has significant clinical value for prognosis evaluations in HCC (28).
Initial treatment has a great impact on the long-term survival of patients with liver cancer. This paper mainly compares and evaluates the efficacy of BCLC-B patients with up-to-seven criterion from the perspective of surgery and TACE, so we use OS as the main evaluation standard. However, due to the high recurrence rate of BCLC-B patients after surgical resection, the reason of recurrence is related to the theory of intrahepatic diffusion or multicenter recurrence of the tumor, and there are various options for the treatment of tumor recurrence, which will affect the survival of patients, so we believe that OS should be used as an important criterion for the efficacy evaluation of cancer patients.
From our existing data, all patients who met up-to-seven criterion in BCLC-B underwent hepatectomy was superior to TACE. From the point of view of exceeding the up-to-seven criterion, the recurrence rate was higher than that of met up-to-seven criterion group, which suggests that the risk of recurrence was relatively high. If the tumor was not located in the same liver lobe, the recurrence rate was relatively high. Based on the progress of targeted therapy and immunotherapy, for the patients who exceeded up-to-seven criterion, we tend to perform neoadjuvant TACE, targeted therapy, or immunotherapy first, and then perform surgical resection after the tumor is appropriately reduced, which may improve the prognosis of the patient. Because it is very difficult to judge MVI before surgery, it can only be detected by postoperative pathology. If patients who meet the up-to-seven criterion confirm the existence of MVI after surgery, we recommend adjuvant TACE treatment after surgery.
Conclusions
In summary, despite the small sample size of our retrospective analysis, our findings suggest that surgery may be the best primary treatment for patients with BCLC-B HCC who meet up-to-7 criterion, but this criterion should not serve as a deciding factor in determining whether to treat patients with BCLC-B surgically. Indeed, the criterion may not be suitable as an indication for surgery in HCC patients with the chronic hepatitis B virus. Based on the up-to-7 criterion, which was developed based on the 2 dimensions of tumor number and tumor size, for HCC patients with BCLC-B, tumor size is not a decisive factor for surgical treatment, but the number of tumors has a significant effect on the prognosis of patients who have undergone surgery. Patients with multiple tumors may also first consider Radiofrequency Ablation (RFA), TACE, immune, targeted, and other therapeutic modalities for translational therapy to obtain the opportunity of surgical treatment. To further validate our findings, more clinical data should continue to be accumulated and large-sample, multicenter studies should be conducted to support the conclusions drawn.
Acknowledgments
Funding: This research was supported by the Suitable Medical and Health Technology Research in Developmental Projects of Guangxi (No. S201516), and the Project of the Guangxi Province Education Commission of the Teacher Foundation for Youth (No. KY2016YB085).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-69/rc
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-69/dss
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-69/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-69/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by board of Ethics Committee of Guangxi Medical University Cancer Hospital (No. LW2022030) and informed consent was taken from all the patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Reig M, Forner A, Rimola J, et al. BCLC strategy for prognosis prediction and treatment recommendation: The 2022 update. J Hepatol 2022;76:681-93. [Crossref] [PubMed]
- Gao R. Hypoxia features as potential indicators in prognosis, immunotherapy and drug screening in hepatocellular carcinoma patients. Transl Cancer Res 2022;11:3932-4. [Crossref] [PubMed]
- Feng H, Yang C, Xu F, et al. Therapeutic efficacy of microwave coagulation versus liver resection for hepatocellular carcinoma within the Milan criteria: A propensity score matching analysis. Eur J Surg Oncol 2022;48:418-24. [Crossref] [PubMed]
- Shin SW, Ahn KS, Kim SW, et al. Liver Resection Versus Local Ablation Therapies for Hepatocellular Carcinoma Within the Milan Criteria: A Systematic Review and Meta-analysis. Ann Surg 2021;273:656-66. [Crossref] [PubMed]
- Mazzaferro V, Llovet JM, Miceli R, et al. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol 2009;10:35-43. [Crossref] [PubMed]
- Hong SK, Jin XL, Suh S, et al. Different Risk Factors for Early and Late Recurrence After Curative Resection of Hepatocellular Carcinoma. World J Surg 2022;46:197-206. [Crossref] [PubMed]
- Xu XF, Xing H, Han J, et al. Risk Factors, Patterns, and Outcomes of Late Recurrence After Liver Resection for Hepatocellular Carcinoma: A Multicenter Study From China. JAMA Surg 2019;154:209-17. [Crossref] [PubMed]
- Wang MD, Li C, Liang L, et al. Early and Late Recurrence of Hepatitis B Virus-Associated Hepatocellular Carcinoma. Oncologist 2020;25:e1541-51. [Crossref] [PubMed]
- Dai Y, Chen G, Chen Y, et al. Usefulness of the estimation of physiologic ability and surgical stress (E-PASS) system for prediction of complication and prognosis in hepatocellular carcinoma patients after hepatectomy. Transl Cancer Res 2022;11:2700-12. [Crossref] [PubMed]
- Deng M, Li S, Wei W, et al. What clinicopathological factors affect the recurrence of hepatocellular carcinoma after surgery? Ann Transl Med 2022;10:1185. [Crossref] [PubMed]
- Zhou Z, Qi L, Mo Q, et al. Effect of surgical margin on postoperative prognosis in patients with solitary hepatocellular carcinoma: A propensity score matching analysis. J Cancer 2021;12:4455-62. [Crossref] [PubMed]
- Bolondi L, Burroughs A, Dufour JF, et al. Heterogeneity of patients with intermediate (BCLC B) Hepatocellular Carcinoma: proposal for a subclassification to facilitate treatment decisions. Semin Liver Dis 2012;32:348-59. [PubMed]
- Kudo M, Arizumi T, Ueshima K, et al. Subclassification of BCLC B Stage Hepatocellular Carcinoma and Treatment Strategies: Proposal of Modified Bolondi's Subclassification (Kinki Criteria). Dig Dis 2015;33:751-8. [Crossref] [PubMed]
- Kudo M, Ueshima K, Chan S, et al. Lenvatinib as an Initial Treatment in Patients with Intermediate-Stage Hepatocellular Carcinoma Beyond Up-To-Seven Criteria and Child-Pugh A Liver Function: A Proof-Of-Concept Study. Cancers (Basel) 2019;11:1084. [Crossref] [PubMed]
- Goyal P, Salem R, Mouli SK. Role of interventional oncology in hepatocellular carcinoma: Future best practice beyond current guidelines. Br J Radiol 2022;95:20220379. [Crossref] [PubMed]
- Wee IJY, Moe FNN, Sultana R, et al. Extending Surgical Resection for Hepatocellular Carcinoma Beyond Barcelona Clinic for Liver Cancer (BCLC) Stage A: A Novel Application of the Modified BCLC Staging System. J Hepatocell Carcinoma 2022;9:839-51. [Crossref] [PubMed]
- Brozzetti S, D'Alterio C, Bini S, et al. Surgical Resection Is Superior to TACE in the Treatment of HCC in a Well Selected Cohort of BCLC-B Elderly Patients-A Retrospective Observational Study. Cancers (Basel) 2022;14:4422. [Crossref] [PubMed]
- Glantzounis GK, Korkolis D, Sotiropoulos GC, et al. Individualized Approach in the Surgical Management of Hepatocellular Carcinoma: Results from a Greek Multicentre Study. Cancers (Basel) 2022;14:4387. [Crossref] [PubMed]
- Wang P, Zhang D, Fang C, et al. Partial hepatectomy vs. transcatheter arterial chemoembolization for multiple hepatocellular carcinomas of BCLC-B stage: A meta-analysis of high-quality studies. Eur J Surg Oncol 2022;48:1685-91. [Crossref] [PubMed]
- Mogahed MM, Zytoon AA, Eysa B, et al. Outcome of Laparoscopic Assisted Percutaneous Microwave Ablation for Exophytic Versus Non-exophytic Hepatocellular Carcinoma. J Gastrointest Cancer 2021;52:892-8. [Crossref] [PubMed]
- Kamiyama T, Orimo T, Wakayama K, et al. Survival outcomes of hepatectomy for stage B Hepatocellular carcinoma in the BCLC classification. World J Surg Oncol 2017;15:156. [Crossref] [PubMed]
- Zhong JH, You XM, Lu SD, et al. Historical Comparison of Overall Survival after Hepatic Resection for Patients With Large and/or Multinodular Hepatocellular Carcinoma. Medicine (Baltimore) 2015;94:e1426. [Crossref] [PubMed]
- Kamiyama T, Nakanishi K, Yokoo H, et al. Analysis of the risk factors for early death due to disease recurrence or progression within 1 year after hepatectomy in patients with hepatocellular carcinoma. World J Surg Oncol 2012;10:107. [Crossref] [PubMed]
- Chen ZH, Zhang XP, Feng JK, et al. Patterns, treatments, and prognosis of tumor recurrence after resection for hepatocellular carcinoma with microvascular invasion: a multic enter study from China. HPB (Oxford) 2022;24:1063-73. [Crossref] [PubMed]
- Huang DS, Liu TT, Lu WT, et al. Comparison of portal and capsular microscopic vascular invasion in the outcomes of early HCC after curative resection. Am J Cancer Res 2022;12:2659-72. [PubMed]
- Liu YN, Xu YK, Deng SY, et al. Research progress in radiomics based on CT and MRI images for prediction of microvascular invasion in hepatocellular carcinoma. Zhonghua Gan Zang Bing Za Zhi 2022;30:809-13. [PubMed]
- Tang Y, Xu L, Ren Y, et al. Identification and Validation of a Prognostic Model Based on Three MVI-Related Genes in Hepatocellular Carcinoma. Int J Biol Sci 2022;18:261-75. [Crossref] [PubMed]


