
A glimpse into the future of esophageal carcinoma in the United States: predicting the future incidence until 2040 based on the current epidemiological data
Highlight box
Key findings
• Using the current Surveillance, Epidemiology, and End Results (SEER) epidemiological data, we predicted the future incidence of esophageal cancer in the United States, which showed a 3.2% increase in incidence of esophageal adenocarcinoma while the incidence of esophageal squamous cell carcinoma declined.
What is known and what is new?
• While esophageal squamous cell carcinoma was most common esophageal cancer in the twentieth century, there has been a dramatic increase in adenocarcinoma subtype of esophageal cancer over the last couple of decades both in Eastern and Western World.
• In the current study, we forecast an increased incidence of adenocarcinoma histology subtype of esophageal cancer while squamous subtype will have a decreased trend over the next two decades.
What is the implication, and what should change now?
• Preventive efforts of esophageal adenocarcinoma should primarily target males of age up to 65 years and females of current age 40 to 65 years who will make up the older age group (>65 years) in 2040.
Introduction
Carcinoma of esophagus is the eighth most common malignancy and is the sixth most common cause of death worldwide (1). In the United States, it is estimated that a total of 20,640 cases of esophageal cancer will be diagnosed in 2022, accounting for 16,410 deaths (2). Esophageal squamous cell carcinoma and adenocarcinoma are two main histologic subtypes that represent majority of esophageal cancers. While esophageal squamous cell carcinoma is common in Eastern World, adenocarcinoma histology is the most common histologic subtype seen in the Western World (3). The incidence of esophageal carcinoma, especially squamous cell histology has been traditionally much higher in regions of Asia, predominantly central Asia, northern part of China, and Iran. Possible etiological factors associated with higher incidence of esophageal squamous cell carcinoma are smoking, alcohol, nutritional habits such as consumption of hot tea, pickles and food rich in N-nitroso compounds, smoked foods, low intake of fruits and vegetables, nutritional deficiencies such as zinc and selenium, or fungal toxins (aflatoxin). In contrast, gastroesophageal reflux disease, obesity, alcohol, and metabolic syndrome have been implicated in the etiopathogenesis of esophageal adenocarcinoma. Notably, majority of esophageal adenocarcinomas have a pre-cancerous Barrett’s metaplasia and dysplasia changes. Given the relative higher incidence of metabolic syndrome in the Western population, esophageal adenocarcinoma histology is not surprisingly more commonly seen histologic subtype of esophageal carcinoma in the Western World. Epidemiological data have shown that the incidence of esophageal cancer has an uptrend, predicting an increase by 140% per decade by 2025 (4). While esophageal squamous cell carcinoma was most common esophageal cancer in the twentieth century, there has been a dramatic increase in adenocarcinoma subtype of esophageal cancer over the last couple of decades both in Eastern and Western World (5). With this changing paradigm of esophageal carcinoma, it is important to forecast the future burden of esophageal carcinoma by histology, age, sex, and race that could potentially help us to plan prevention and control strategies for esophageal carcinoma. In the current study we sought to estimate the future burden of esophageal carcinoma by histology, age, sex, and race, which could help plan prevention, control, and treatment strategies for this cancer. We present the following article in accordance with the STROBE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-729/rc).
Methods
We extracted incidence and population data on esophageal carcinoma between the years 2000 and 2016 from the Surveillance, Epidemiology, and End Results (SEER) 18 registries using the SEER*Stat 8.3.4 (https://seer.cancer.gov/seerstat/) statistical software. SEER is a population-based registry program of the US National Cancer Institute that covers 28% of the population diagnosed each year. We identified esophageal carcinoma cases that were histologically confirmed using International Classification of Diseases for Oncology, 3rd edition. Histology codes 8050–8078 and 8083–8084 were used to extract esophageal squamous cell carcinoma cases while 8140, 8141, 8143–8145, 8190–8231, 8260–8263, 8310, 8401, 8480–8490, 8550–8551, 8570–8574, and 8576 codes were used to extract adenocarcinoma subtypes. Of note, other rare histologic subtypes of esophageal carcinomas such as sarcomatous variants and neuroendocrine tumors were excluded. Poisson regression was used to model the trend in incidence rates over time based on age, sex, and race. Future trends in the incidence of esophageal cancer were predicted by histology up to the year 2030 by taking a weighted average of the projected incidence rates for the last two prediction periods, and then applying the rates to the United States national population forecasts. Assuming these population trends would hold into the future, we estimated the forecasted incidence rates and 95% confidence intervals per 100,000 person years. All analyses were performed using R version 4.0.3 (R Core Team, R Foundation for Statistical Computing, Vienna, Austria). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As the Surveillance, Epidemiology, and End Results (SEER) Program contains de-identified data, individual consent for this retrospective analysis was waived by the Mayo Clinic Institutional Review Board.
Results
Esophageal adenocarcinoma
This forecasting study suggest that the incidence (per 100,000 persons) of esophageal adenocarcinoma is increasing in people within age group of 40–65 years while a decreased trend was noticed in age >65 years (Figure 1). Our prediction showed that the incidence of esophageal adenocarcinoma for age group 40–65 years will increase from 2.12 in 2021 to 3.86 in 2040, which corresponds to an 82% increase over the course of 19 years (3.2% per year, 95% CI: −2.3% to 9.1%) (Table 1). Males seem to have a considerable increase in incidence of esophageal adenocarcinoma with the predicted increase in incidence to 4.02 in 2040 as compared to 3.71 in 2021 (Table 2). We noticed a similar increase in incidence rates per year among Black and Whites in 40–65 years age group (3.8%, and 3.5%, per year respectively) (Table S1). On the contrary, the incidence of esophageal adenocarcinoma remained stable in Asians aged between 40–65 years between the years 2021 and 2040, 0.78 and 0.77 per 100,000 persons, respectively. We noticed that the incidence of esophageal adenocarcinoma doubled (a 100% increase over the span of 2 decades) in White and Black females aged 40–65 from the year 2021 (0.98 and 0.43, respectively) to 2040 (1.82 and 0.82, respectively). On the contrary, the incidence in Asian females aged 40–65 seem to remain the same between 2021 and 2040 (0.11 and 0.13, respectively) (Table 3).
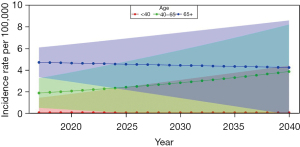
Table 1
| Year | Age <40 years | Age 40–65 years | Age 65+ years |
|---|---|---|---|
| 2017 | 0.05 | 1.87 | 4.71 |
| 2018 | 0.05 | 1.93 | 4.68 |
| 2019 | 0.05 | 1.99 | 4.66 |
| 2020 | 0.05 | 2.06 | 4.64 |
| 2021 | 0.05 | 2.12 | 4.62 |
| 2022 | 0.05 | 2.19 | 4.60 |
| 2023 | 0.05 | 2.26 | 4.58 |
| 2024 | 0.05 | 2.33 | 4.56 |
| 2025 | 0.05 | 2.41 | 4.54 |
| 2026 | 0.05 | 2.48 | 4.51 |
| 2027 | 0.05 | 2.56 | 4.49 |
| 2028 | 0.05 | 2.65 | 4.47 |
| 2029 | 0.05 | 2.73 | 4.45 |
| 2030 | 0.05 | 2.82 | 4.43 |
| 2031 | 0.05 | 2.91 | 4.41 |
| 2032 | 0.05 | 3.00 | 4.39 |
| 2033 | 0.05 | 3.10 | 4.37 |
| 2034 | 0.05 | 3.20 | 4.35 |
| 2035 | 0.05 | 3.30 | 4.33 |
| 2036 | 0.05 | 3.40 | 4.31 |
| 2037 | 0.05 | 3.51 | 4.29 |
| 2038 | 0.05 | 3.63 | 4.27 |
| 2039 | 0.05 | 3.74 | 4.25 |
| 2040 | 0.05 | 3.86 | 4.23 |
Table 2
| Year | Males | Females |
|---|---|---|
| 2017 | 3.75 | 0.62 |
| 2018 | 3.76 | 0.62 |
| 2019 | 3.77 | 0.62 |
| 2020 | 3.78 | 0.62 |
| 2021 | 3.79 | 0.62 |
| 2022 | 3.81 | 0.63 |
| 2023 | 3.82 | 0.63 |
| 2024 | 3.83 | 0.63 |
| 2025 | 3.84 | 0.63 |
| 2026 | 3.85 | 0.63 |
| 2027 | 3.86 | 0.63 |
| 2028 | 3.88 | 0.63 |
| 2029 | 3.89 | 0.63 |
| 2030 | 3.90 | 0.63 |
| 2031 | 3.91 | 0.64 |
| 2032 | 3.92 | 0.64 |
| 2033 | 3.94 | 0.64 |
| 2034 | 3.95 | 0.64 |
| 2035 | 3.96 | 0.64 |
| 2036 | 3.97 | 0.64 |
| 2037 | 3.99 | 0.64 |
| 2038 | 4.00 | 0.64 |
| 2039 | 4.01 | 0.65 |
| 2040 | 4.02 | 0.65 |
Table 3
| Year | Females, age <40 years | Females, age 40–65 years | Females, age 65+ years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | White | Black | Asian | Other | |||
| 2017 | 0.02 | 0.00 | 0.00 | 0.03 | 0.83 | 0.36 | 0.11 | 0.68 | 2.53 | 0.87 | 0.33 | 1.93 | ||
| 2018 | 0.02 | 0.00 | 0.00 | 0.03 | 0.85 | 0.37 | 0.11 | 0.71 | 2.52 | 0.87 | 0.32 | 1.94 | ||
| 2019 | 0.02 | 0.00 | 0.00 | 0.03 | 0.88 | 0.39 | 0.11 | 0.74 | 2.51 | 0.87 | 0.31 | 1.95 | ||
| 2020 | 0.02 | 0.00 | 0.00 | 0.03 | 0.92 | 0.40 | 0.11 | 0.78 | 2.49 | 0.86 | 0.30 | 1.97 | ||
| 2021 | 0.02 | 0.00 | 0.00 | 0.03 | 0.95 | 0.42 | 0.11 | 0.81 | 2.48 | 0.86 | 0.29 | 1.98 | ||
| 2022 | 0.02 | 0.00 | 0.00 | 0.03 | 0.98 | 0.43 | 0.11 | 0.85 | 2.47 | 0.86 | 0.28 | 1.99 | ||
| 2023 | 0.02 | 0.00 | 0.00 | 0.04 | 1.01 | 0.45 | 0.11 | 0.89 | 2.46 | 0.86 | 0.27 | 2.00 | ||
| 2024 | 0.03 | 0.00 | 0.00 | 0.04 | 1.05 | 0.46 | 0.11 | 0.93 | 2.44 | 0.85 | 0.27 | 2.01 | ||
| 2025 | 0.03 | 0.00 | 0.00 | 0.04 | 1.09 | 0.48 | 0.11 | 0.98 | 2.43 | 0.85 | 0.26 | 2.03 | ||
| 2026 | 0.03 | 0.00 | 0.00 | 0.04 | 1.12 | 0.50 | 0.11 | 1.02 | 2.42 | 0.85 | 0.25 | 2.04 | ||
| 2027 | 0.03 | 0.00 | 0.00 | 0.04 | 1.16 | 0.52 | 0.12 | 1.07 | 2.41 | 0.84 | 0.24 | 2.05 | ||
| 2028 | 0.03 | 0.00 | 0.00 | 0.04 | 1.20 | 0.53 | 0.12 | 1.12 | 2.39 | 0.84 | 0.23 | 2.06 | ||
| 2029 | 0.03 | 0.00 | 0.00 | 0.04 | 1.25 | 0.55 | 0.12 | 1.17 | 2.38 | 0.84 | 0.23 | 2.08 | ||
| 2030 | 0.03 | 0.00 | 0.00 | 0.04 | 1.29 | 0.57 | 0.12 | 1.22 | 2.37 | 0.84 | 0.22 | 2.09 | ||
| 2031 | 0.03 | 0.00 | 0.00 | 0.04 | 1.34 | 0.60 | 0.12 | 1.28 | 2.36 | 0.83 | 0.21 | 2.10 | ||
| 2032 | 0.03 | 0.00 | 0.00 | 0.05 | 1.38 | 0.62 | 0.12 | 1.34 | 2.35 | 0.83 | 0.20 | 2.11 | ||
| 2033 | 0.03 | 0.00 | 0.00 | 0.05 | 1.43 | 0.64 | 0.12 | 1.40 | 2.33 | 0.83 | 0.20 | 2.13 | ||
| 2034 | 0.03 | 0.00 | 0.00 | 0.05 | 1.48 | 0.66 | 0.12 | 1.47 | 2.32 | 0.82 | 0.19 | 2.14 | ||
| 2035 | 0.03 | 0.00 | 0.00 | 0.05 | 1.53 | 0.69 | 0.12 | 1.54 | 2.31 | 0.82 | 0.19 | 2.15 | ||
| 2036 | 0.03 | 0.00 | 0.00 | 0.05 | 1.59 | 0.71 | 0.12 | 1.61 | 2.30 | 0.82 | 0.18 | 2.17 | ||
| 2037 | 0.03 | 0.00 | 0.00 | 0.05 | 1.64 | 0.74 | 0.12 | 1.68 | 2.29 | 0.82 | 0.17 | 2.18 | ||
| 2038 | 0.03 | 0.00 | 0.00 | 0.05 | 1.70 | 0.77 | 0.12 | 1.76 | 2.28 | 0.81 | 0.17 | 2.19 | ||
| 2039 | 0.03 | 0.01 | 0.00 | 0.05 | 1.76 | 0.79 | 0.12 | 1.84 | 2.26 | 0.81 | 0.16 | 2.21 | ||
| 2040 | 0.03 | 0.01 | 0.00 | 0.06 | 1.82 | 0.82 | 0.13 | 1.93 | 2.25 | 0.81 | 0.16 | 2.22 | ||
White males aged >65 years had highest incidence of esophageal adenocarcinoma (17.34 in 2021) and incidence decreased 1.3% per year. We noticed a marginal decreased incidence in Black male (−1.1% per year) and Asian male (−3.9% per year) population aged >65 years (Table 4). On subgroup analysis by sex, we noticed a similar marginal decreased incidence in Black male (−1.1% per year) and Asian male (−3.9% per year) population aged >65 years. Though a decrease in trend is noticed in White males aged >65 years, they remain to be at higher risk of esophageal adenocarcinoma in the year 2040 (13.63 per 100,000) as compared to the other age groups of 40–65 years (12.60 per 100,000) and <40 years (0.23 per 100,000). Of note, we noticed a decrease in incidence of esophageal adenocarcinoma in White, Black, and Asian females aged >65 years from the year 2021 to 2040 (Table 3).
Table 4
| Year | Males, age <40 years | Males, age 40–65 years | Males, age 65+ years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | White | Black | Asian | Other | |||
| 2017 | 0.18 | 0.02 | 0.05 | 0.15 | 6.97 | 1.60 | 0.78 | 3.26 | 18.24 | 3.33 | 2.33 | 6.04 | ||
| 2018 | 0.19 | 0.02 | 0.05 | 0.15 | 7.16 | 1.65 | 0.78 | 3.39 | 18.01 | 3.30 | 2.24 | 6.03 | ||
| 2019 | 0.19 | 0.02 | 0.05 | 0.15 | 7.36 | 1.69 | 0.78 | 3.52 | 17.79 | 3.26 | 2.15 | 6.02 | ||
| 2020 | 0.19 | 0.02 | 0.05 | 0.16 | 7.56 | 1.74 | 0.78 | 3.65 | 17.56 | 3.22 | 2.07 | 6.01 | ||
| 2021 | 0.19 | 0.02 | 0.05 | 0.16 | 7.76 | 1.79 | 0.78 | 3.80 | 17.34 | 3.19 | 1.98 | 6.00 | ||
| 2022 | 0.19 | 0.02 | 0.04 | 0.16 | 7.97 | 1.85 | 0.78 | 3.94 | 17.12 | 3.15 | 1.91 | 6.00 | ||
| 2023 | 0.19 | 0.03 | 0.04 | 0.17 | 8.19 | 1.90 | 0.78 | 4.09 | 16.91 | 3.12 | 1.83 | 5.99 | ||
| 2024 | 0.20 | 0.03 | 0.04 | 0.17 | 8.41 | 1.95 | 0.78 | 4.25 | 16.70 | 3.08 | 1.76 | 5.98 | ||
| 2025 | 0.20 | 0.03 | 0.04 | 0.17 | 8.64 | 2.01 | 0.78 | 4.42 | 16.49 | 3.05 | 1.69 | 5.97 | ||
| 2026 | 0.20 | 0.03 | 0.04 | 0.18 | 8.87 | 2.07 | 0.78 | 4.59 | 16.28 | 3.02 | 1.62 | 5.96 | ||
| 2027 | 0.20 | 0.03 | 0.04 | 0.18 | 9.11 | 2.13 | 0.78 | 4.76 | 16.07 | 2.98 | 1.56 | 5.95 | ||
| 2028 | 0.20 | 0.03 | 0.04 | 0.18 | 9.36 | 2.19 | 0.78 | 4.95 | 15.87 | 2.95 | 1.50 | 5.94 | ||
| 2029 | 0.21 | 0.03 | 0.04 | 0.19 | 9.61 | 2.25 | 0.78 | 5.14 | 15.67 | 2.92 | 1.44 | 5.93 | ||
| 2030 | 0.21 | 0.03 | 0.04 | 0.19 | 9.87 | 2.32 | 0.78 | 5.34 | 15.47 | 2.89 | 1.38 | 5.92 | ||
| 2031 | 0.21 | 0.03 | 0.04 | 0.20 | 10.14 | 2.38 | 0.78 | 5.54 | 15.28 | 2.85 | 1.33 | 5.91 | ||
| 2032 | 0.21 | 0.03 | 0.04 | 0.20 | 10.42 | 2.45 | 0.77 | 5.75 | 15.09 | 2.82 | 1.27 | 5.90 | ||
| 2033 | 0.21 | 0.03 | 0.04 | 0.20 | 10.70 | 2.52 | 0.77 | 5.98 | 14.90 | 2.79 | 1.22 | 5.89 | ||
| 2034 | 0.21 | 0.03 | 0.04 | 0.21 | 10.99 | 2.59 | 0.77 | 6.21 | 14.71 | 2.76 | 1.18 | 5.88 | ||
| 2035 | 0.22 | 0.03 | 0.04 | 0.21 | 11.29 | 2.67 | 0.77 | 6.45 | 14.53 | 2.73 | 1.13 | 5.87 | ||
| 2036 | 0.22 | 0.03 | 0.03 | 0.22 | 11.59 | 2.75 | 0.77 | 6.70 | 14.34 | 2.70 | 1.09 | 5.86 | ||
| 2037 | 0.22 | 0.03 | 0.03 | 0.22 | 11.91 | 2.82 | 0.77 | 6.95 | 14.16 | 2.67 | 1.04 | 5.86 | ||
| 2038 | 0.22 | 0.03 | 0.03 | 0.22 | 12.23 | 2.91 | 0.77 | 7.22 | 13.98 | 2.64 | 1.00 | 5.85 | ||
| 2039 | 0.22 | 0.03 | 0.03 | 0.23 | 12.56 | 2.99 | 0.77 | 7.50 | 13.81 | 2.61 | 0.96 | 5.84 | ||
| 2040 | 0.23 | 0.03 | 0.03 | 0.23 | 12.90 | 3.08 | 0.77 | 7.79 | 13.63 | 2.59 | 0.92 | 5.83 | ||
Esophageal squamous cell carcinoma
Interestingly, we found a considerable decrease in the incidence of esophageal squamous cell carcinoma in the current age groups 40–65 (−2.7% per year) and >65 years (−4.6% per year) (Figure 2, Table S2). We observed a similar decrease in incidence of esophageal squamous cell carcinoma between the years 2021 and 2040 in Whites (−60.7%), Blacks (−55.7%), and Asians (−56.3%) (Table 5). We noticed a decreased trend of esophageal squamous cell carcinoma in males across all the current age groups of 40–65 and >65 years (Table 6). A similar trend is predicted in females except Black females of current age group of 40–65 years in which the incidence is marginal raised from (0.87 to 1.01 per 100,000, 16% increase over 2 decades) (Table 7).

Table 5
| Year | White | Black | Asian | Other |
|---|---|---|---|---|
| 2017 | 0.58 | 1.45 | 0.65 | 0.33 |
| 2018 | 0.56 | 1.39 | 0.62 | 0.31 |
| 2019 | 0.55 | 1.33 | 0.59 | 0.29 |
| 2020 | 0.53 | 1.27 | 0.57 | 0.27 |
| 2021 | 0.51 | 1.22 | 0.55 | 0.26 |
| 2022 | 0.50 | 1.17 | 0.52 | 0.24 |
| 2023 | 0.48 | 1.12 | 0.50 | 0.23 |
| 2024 | 0.47 | 1.07 | 0.48 | 0.22 |
| 2025 | 0.46 | 1.03 | 0.46 | 0.21 |
| 2026 | 0.44 | 0.98 | 0.44 | 0.19 |
| 2027 | 0.43 | 0.94 | 0.42 | 0.18 |
| 2028 | 0.42 | 0.90 | 0.40 | 0.17 |
| 2029 | 0.41 | 0.86 | 0.39 | 0.16 |
| 2030 | 0.39 | 0.83 | 0.37 | 0.15 |
| 2031 | 0.38 | 0.79 | 0.35 | 0.15 |
| 2032 | 0.37 | 0.76 | 0.34 | 0.14 |
| 2033 | 0.36 | 0.73 | 0.32 | 0.13 |
| 2034 | 0.35 | 0.70 | 0.31 | 0.12 |
| 2035 | 0.34 | 0.67 | 0.30 | 0.12 |
| 2036 | 0.33 | 0.64 | 0.28 | 0.11 |
| 2037 | 0.32 | 0.61 | 0.27 | 0.10 |
| 2038 | 0.31 | 0.59 | 0.26 | 0.10 |
| 2039 | 0.30 | 0.56 | 0.25 | 0.09 |
| 2040 | 0.20 | 0.54 | 0.24 | 0.09 |
Table 6
| Year | Males, age <40 years | Males, age 40–65 years | Males, age 65+ years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | White | Black | Asian | Other | |||
| 2017 | 0.00 | 0.00 | 0.00 | 0.00 | 0.50 | 2.47 | 0.53 | 0.40 | 1.51 | 5.20 | 1.89 | 1.76 | ||
| 2018 | 0.00 | 0.00 | 0.00 | 0.00 | 0.49 | 2.46 | 0.51 | 0.41 | 1.42 | 4.99 | 1.75 | 1.72 | ||
| 2019 | 0.00 | 0.00 | 0.00 | 0.00 | 0.48 | 2.46 | 0.49 | 0.41 | 1.34 | 4.79 | 1.61 | 1.68 | ||
| 2020 | 0.00 | 0.00 | 0.00 | 0.00 | 0.47 | 2.46 | 0.47 | 0.42 | 1.26 | 4.60 | 1.49 | 1.64 | ||
| 2021 | 0.00 | 0.00 | 0.00 | 0.00 | 0.46 | 2.45 | 0.45 | 0.43 | 1.19 | 4.41 | 1.38 | 1.60 | ||
| 2022 | 0.00 | 0.00 | 0.00 | 0.00 | 0.46 | 2.45 | 0.44 | 0.43 | 1.12 | 4.23 | 1.28 | 1.56 | ||
| 2023 | 0.00 | 0.00 | 0.00 | 0.00 | 0.45 | 2.45 | 0.42 | 0.44 | 1.05 | 4.06 | 1.18 | 1.53 | ||
| 2024 | 0.00 | 0.00 | 0.00 | 0.00 | 0.44 | 2.44 | 0.40 | 0.45 | 0.99 | 3.90 | 1.09 | 1.49 | ||
| 2025 | 0.00 | 0.00 | 0.00 | 0.00 | 0.43 | 2.44 | 0.39 | 0.46 | 0.94 | 3.74 | 1.01 | 1.46 | ||
| 2026 | 0.00 | 0.00 | 0.00 | 0.00 | 0.42 | 2.43 | 0.37 | 0.46 | 0.88 | 3.59 | 0.94 | 1.42 | ||
| 2027 | 0.00 | 0.00 | 0.00 | 0.00 | 0.41 | 2.43 | 0.36 | 0.47 | 0.83 | 3.44 | 0.87 | 1.39 | ||
| 2028 | 0.00 | 0.00 | 0.00 | 0.00 | 0.40 | 2.43 | 0.35 | 0.48 | 0.78 | 3.31 | 0.80 | 1.36 | ||
| 2029 | 0.00 | 0.00 | 0.00 | 0.00 | 0.40 | 2.42 | 0.33 | 0.49 | 0.74 | 3.17 | 0.74 | 1.33 | ||
| 2030 | 0.00 | 0.00 | 0.00 | 0.00 | 0.39 | 2.42 | 0.32 | 0.50 | 0.70 | 3.04 | 0.69 | 1.30 | ||
| 2031 | 0.00 | 0.00 | 0.00 | 0.00 | 0.38 | 2.42 | 0.31 | 0.50 | 0.66 | 2.92 | 0.63 | 1.27 | ||
| 2032 | 0.00 | 0.00 | 0.00 | 0.00 | 0.37 | 2.41 | 0.30 | 0.51 | 0.62 | 2.80 | 0.59 | 1.24 | ||
| 2033 | 0.00 | 0.00 | 0.00 | 0.00 | 0.37 | 2.41 | 0.29 | 0.52 | 0.58 | 2.69 | 0.54 | 1.21 | ||
| 2034 | 0.00 | 0.00 | 0.00 | 0.00 | 0.36 | 2.40 | 0.28 | 0.53 | 0.55 | 2.58 | 0.50 | 1.18 | ||
| 2035 | 0.00 | 0.00 | 0.00 | 0.00 | 0.35 | 2.40 | 0.27 | 0.54 | 0.52 | 2.48 | 0.46 | 1.15 | ||
| 2036 | 0.00 | 0.00 | 0.00 | 0.00 | 0.35 | 2.40 | 0.26 | 0.55 | 0.49 | 2.38 | 0.43 | 1.13 | ||
| 2037 | 0.00 | 0.00 | 0.00 | 0.00 | 0.34 | 2.39 | 0.25 | 0.56 | 0.46 | 2.28 | 0.40 | 1.10 | ||
| 2038 | 0.00 | 0.00 | 0.00 | 0.00 | 0.33 | 2.39 | 0.24 | 0.56 | 0.43 | 2.19 | 0.37 | 1.08 | ||
| 2039 | 0.00 | 0.00 | 0.00 | 0.00 | 0.33 | 2.39 | 0.23 | 0.57 | 0.41 | 2.10 | 0.34 | 1.05 | ||
| 2040 | 0.00 | 0.00 | 0.00 | 0.00 | 0.32 | 2.38 | 0.22 | 0.58 | 0.38 | 2.01 | 0.31 | 1.03 | ||
Table 7
| Year | Females, age <40 years | Females, age 40–65 years | Females, age 65+ years | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| White | Black | Asian | Other | White | Black | Asian | Other | White | Black | Asian | Other | |||
| 2017 | 0.00 | 0.00 | 0.00 | 0.00 | 0.19 | 0.84 | 0.15 | 0.37 | 0.74 | 1.49 | 0.57 | 0.42 | ||
| 2018 | 0.00 | 0.00 | 0.00 | 0.00 | 0.19 | 0.85 | 0.14 | 0.38 | 0.71 | 1.44 | 0.54 | 0.42 | ||
| 2019 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.85 | 0.14 | 0.39 | 0.67 | 1.40 | 0.50 | 0.41 | ||
| 2020 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.86 | 0.14 | 0.40 | 0.64 | 1.35 | 0.47 | 0.41 | ||
| 2021 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.87 | 0.13 | 0.41 | 0.61 | 1.31 | 0.44 | 0.40 | ||
| 2022 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.87 | 0.13 | 0.42 | 0.58 | 1.27 | 0.41 | 0.40 | ||
| 2023 | 0.00 | 0.00 | 0.00 | 0.00 | 0.18 | 0.88 | 0.12 | 0.44 | 0.55 | 1.23 | 0.38 | 0.39 | ||
| 2024 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.89 | 0.12 | 0.45 | 0.53 | 1.19 | 0.36 | 0.39 | ||
| 2025 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.90 | 0.12 | 0.46 | 0.50 | 1.16 | 0.33 | 0.38 | ||
| 2026 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.90 | 0.11 | 0.47 | 0.48 | 1.12 | 0.31 | 0.37 | ||
| 2027 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.91 | 0.11 | 0.48 | 0.45 | 1.09 | 0.29 | 0.37 | ||
| 2028 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.92 | 0.11 | 0.50 | 0.43 | 1.05 | 0.27 | 0.36 | ||
| 2029 | 0.00 | 0.00 | 0.00 | 0.00 | 0.17 | 0.92 | 0.10 | 0.51 | 0.41 | 1.02 | 0.25 | 0.36 | ||
| 2030 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.93 | 0.10 | 0.52 | 0.39 | 0.99 | 0.24 | 0.35 | ||
| 2031 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.94 | 0.10 | 0.54 | 0.37 | 0.96 | 0.22 | 0.35 | ||
| 2032 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.95 | 0.10 | 0.55 | 0.35 | 0.93 | 0.21 | 0.35 | ||
| 2033 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.96 | 0.09 | 0.56 | 0.34 | 0.90 | 0.19 | 0.34 | ||
| 2034 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.96 | 0.09 | 0.58 | 0.32 | 0.87 | 0.18 | 0.34 | ||
| 2035 | 0.00 | 0.00 | 0.00 | 0.00 | 0.16 | 0.97 | 0.09 | 0.60 | 0.30 | 0.84 | 0.17 | 0.33 | ||
| 2036 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 0.98 | 0.09 | 0.61 | 0.29 | 0.82 | 0.16 | 0.33 | ||
| 2037 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 0.99 | 0.08 | 0.63 | 0.28 | 0.79 | 0.15 | 0.32 | ||
| 2038 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 1.00 | 0.08 | 0.64 | 0.26 | 0.77 | 0.14 | 0.32 | ||
| 2039 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 1.00 | 0.08 | 0.66 | 0.25 | 0.74 | 0.13 | 0.31 | ||
| 2040 | 0.00 | 0.00 | 0.00 | 0.00 | 0.15 | 1.01 | 0.08 | 0.68 | 0.24 | 0.72 | 0.12 | 0.31 | ||
Discussion
Our prediction model noticed interesting findings of estimated dramatic change in the epidemiology of esophageal carcinoma over the next two decades. While esophageal squamous cell histology has historically been the predominant subtype, the critical observation in our prediction showed a uniform decrease in the squamous histology across all age groups and races, except for Black females in which we noticed a stable incidence over the next two decades. Such an increase in the incidence of esophageal adenocarcinoma in the United States and Europe was seen in other studies that utilized regional cancer registries to predict the future incidence of esophageal carcinoma (6). For instance, Arnold et al. predicted an astonishing 214% increase in esophageal adenocarcinoma in the Netherlands. Similar upward trend was noticed in the United States, United Kingdom, and France (6). Similar increased incidence of esophageal adenocarcinoma subtype was noted in another SEER database-based study that calculated the future incidence of esophageal adenocarcinoma based on its incidence between the years 1975–2010 (7). However, the study did not predict the incidence of esophageal squamous cell carcinoma, nor looked various subgroups which we reported in the current study.
The increased incidence of esophageal adenocarcinoma may be attributed to the rising incidence of etiological factors such as gastroesophageal reflux disease, Barrett’s esophagus, metabolic syndrome, obesity, and a decreased incidence of Helicobacter pylori infection (8,9). Barrett’s esophagus and high grade dysplasia are well-establish etiological factors for esophageal adenocarcinoma (10). A nationwide demographic study from Denmark in patients with low-grade dysplasia and non-dysplastic Barret’s esophagus demonstrated a progression to esophageal adenocarcinoma at the rate of 0.12% per person per year (11). In addition, a meta-analysis from Desai et al., reported a progression of Barrett’s esophagus to esophageal adenocarcinoma at the rate of 0.33% per year (10). A cross-sectional study from OneFlorida Clinical Data Research Network electronic health record that covers >40% residents in Florida has demonstrated a roaring 50% increased incidence of Barrett’s esophagus in middle aged adults (45–64-year age group) in the year 2019 as compared to that of 2012 (12). This increased incidence in Barrett’s esophagus may support our prediction of rising incidence of esophageal adenocarcinoma, especially in the population aging 40–65 years. In addition, epidemiological data have shown that gastroesophageal reflux disease and esophageal adenocarcinoma are strongly associated with central adiposity (13). Notably, a prospective study has demonstrated that a body mass index (BMI) > 30 kg/m2 increases the risk of esophageal adenocarcinoma by two-fold and the risk further increased by 2.5-fold in people with BMI >35 kg/m2 (14). Molecular data have shown that abdominal adipose tissue secretes inflammatory cytokines and adipokines that play a significant role in the development of gastroesophageal reflux disease and Barrett’s esophagus and eventually to esophageal adenocarcinoma (15). A cross-sectional National Health and Nutrition Examination Survey (NHANES) revealed an increased trends of obesity in the United States population in the recent years as compared to 2007–2008 (16). Such an increased prevalence of obesity may partly explain the increase in incidence of esophageal adenocarcinoma predicted in our analysis. Interestingly, there seem to be an inverse association of Helicobacter pylori infection and esophageal adenocarcinoma, which may partly be explained by decreased gastric acid secretion caused by the infection (9). A recent cross-sectional study in the United States involving 1,289,641 patients undergoing esophago-duodenoscopy have demonstrated a statistically significant decline in prevalence of Helicobacter pylori infection between the years 2009 and 2018 (17). This decreased prevalence of Helicobacter pylori infection may have contributed to increased gastric acidity further contributing to increased incidence of esophageal adenocarcinoma.
Cigarette smoking and alcohol consumption are well-known risk factors for esophageal squamous cell carcinoma. Recent data from Centers from Diseases Control and Prevention have shown a gradual decline in cigarette smoking in the adult United States population (42.4%, 13.9%, and 12.5% in 1965, 2017, and 2020, respectively) (18). Such a gradual decline in the smoking could partly explain the decline in the incidence of esophageal squamous cell carcinoma.
Study limitations exist and are inherent to registry-based studies and demographics. First, although we built the statistical prediction model using Poisson regression based on the recent epidemiological data, the assumed prediction may involve some degree of uncertainty. Nonetheless, our prediction model has noticed fairly close incidences through the years 2017 through 2022. Second, given the fact that our prediction model is derived from SEER database, possible reporting errors such as under-reporting diagnoses to the database could potentially influence our prediction of future incidence rates. In addition, there could be an under or over-estimation of esophageal adenocarcinoma, especially at the gastro-esophageal junction as there is a possibility of gastric adenocarcinomas being reported as esophageal adenocarcinoma and vice-versa. Third, we did not take into the account of changing technology and guidelines that could lead to enhanced detection of cancers, especially in high-risk individuals such as with gastroesophageal reflux disease could also change the overall incidence of esophageal cancer. Moreover, we did not consider any change in the migration patterns and etiological exposure that could alter the future incidence of esophageal cancer. Furthermore, SEER database does not have information on etiologic risk factors including gastroesophageal reflux disease, smoking and obesity. Nonetheless, our prediction model provides a valuable data on future incidence of esophageal cancer based on the subtype, which helps us in acting up on reducing the etiological factors and focusing on appropriate preventative measures. Behavioral modification in population including weight loss, dietary changes, exercise, decreasing tobacco and alcohol consumption could potentially decrease the development of esophageal cancers.
Conclusions
In summary, over the next two decades, we forecast an increased incidence of adenocarcinoma histology subtype of esophageal cancer while squamous subtype will have a decreased trend. Prevention efforts of esophageal adenocarcinoma such has dietary changes, effective management of obesity, and early treatment of gastroesophageal reflux disease should especially target expected high risk groups like males of age up to 65 years and females of current age 40 to 65 years who will make up the older age group (>65 years) in 2040.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-729/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-729/coif). SC has honoraria from Haliodx, QED Therapeutics, Natera, and speakers’ bureau for Natera. ZJ has consulting or advisory role for Novartis (Inst), QED Therapeutics (Inst), Lilly (Inst), GlaxoSmithKline (Inst), and Daiichi Sankyo/Astra Zeneca (Inst). AM serves on the advisory Board for Taiho oncology, Astrazeneca and QED Therapeutics. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). As the Surveillance, Epidemiology, and End Results (SEER) Program contains de-identified data, individual consent for this retrospective analysis was waived by the Mayo Clinic Institutional Review Board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Napier KJ, Scheerer M, Misra S. Esophageal cancer: A Review of epidemiology, pathogenesis, staging workup and treatment modalities. World J Gastrointest Oncol 2014;6:112-20. [Crossref] [PubMed]
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Cook MB, Chow WH, Devesa SS. Oesophageal cancer incidence in the United States by race, sex, and histologic type, 1977-2005. Br J Cancer 2009;101:855-9. [Crossref] [PubMed]
- Lambert R, Hainaut P. The multidisciplinary management of gastrointestinal cancer. Epidemiology of oesophagogastric cancer. Best Pract Res Clin Gastroenterol 2007;21:921-45. [Crossref] [PubMed]
- Edgren G, Adami HO, Weiderpass E, et al. A global assessment of the oesophageal adenocarcinoma epidemic. Gut 2013;62:1406-14. [Crossref] [PubMed]
- Arnold M, Laversanne M, Brown LM, et al. Predicting the Future Burden of Esophageal Cancer by Histological Subtype: International Trends in Incidence up to 2030. Am J Gastroenterol 2017;112:1247-55. [Crossref] [PubMed]
- Kong CY, Kroep S, Curtius K, et al. Exploring the recent trend in esophageal adenocarcinoma incidence and mortality using comparative simulation modeling. Cancer Epidemiol Biomarkers Prev 2014;23:997-1006. [Crossref] [PubMed]
- Ryan AM, Duong M, Healy L, et al. Obesity, metabolic syndrome and esophageal adenocarcinoma: epidemiology, etiology and new targets. Cancer Epidemiol 2011;35:309-19. [Crossref] [PubMed]
- Islami F, Kamangar F. Helicobacter pylori and esophageal cancer risk: a meta-analysis. Cancer Prev Res (Phila) 2008;1:329-38. [Crossref] [PubMed]
- Desai TK, Krishnan K, Samala N, et al. The incidence of oesophageal adenocarcinoma in non-dysplastic Barrett's oesophagus: a meta-analysis. Gut 2012;61:970-6. [Crossref] [PubMed]
- Hvid-Jensen F, Pedersen L, Drewes AM, et al. Incidence of adenocarcinoma among patients with Barrett's esophagus. N Engl J Med 2011;365:1375-83. [Crossref] [PubMed]
- Qumseya BJ SR. Alarming increase in prevalence of esophageal cancer and Barrett’s esophagus in middle-aged patients: findings from a statewide database of over five million patients. Presented at: DDW 2022; May 21-24, 2022; San Diego, CA. Abstract 671.
- Chang P, Friedenberg F. Obesity and GERD. Gastroenterol Clin North Am 2014;43:161-73. [Crossref] [PubMed]
- Abnet CC, Freedman ND, Hollenbeck AR, et al. A prospective study of BMI and risk of oesophageal and gastric adenocarcinoma. Eur J Cancer 2008;44:465-71. [Crossref] [PubMed]
- Runge TM, Abrams JA, Shaheen NJ. Epidemiology of Barrett's Esophagus and Esophageal Adenocarcinoma. Gastroenterol Clin North Am 2015;44:203-31. [Crossref] [PubMed]
- Hales CM, Fryar CD, Carroll MD, et al. Trends in Obesity and Severe Obesity Prevalence in US Youth and Adults by Sex and Age, 2007-2008 to 2015-2016. JAMA 2018;319:1723-5. [Crossref] [PubMed]
- Sonnenberg A, Turner KO, Genta RM. Low Prevalence of Helicobacter pylori-Positive Peptic Ulcers in Private Outpatient Endoscopy Centers in the United States. Am J Gastroenterol 2020;115:244-50. [Crossref] [PubMed]
- CDC. Burden of Cigarette Use in the United States. Available online: https://www.cdc.gov/tobacco/campaign/tips/resources/data/cigarette-smoking-in-united-states.html. Accessed July 15, 2022.


