
Application of the intestine diversion tube with a double-balloon without ileostomy in low rectal cancer
Highlight box
Key findings
• The intestine diversion tube with a double-balloon was found to be safe and effective in animal experiments. Its use removes the need for ostomy and reduces surgical trauma.
What is known and what is new?
• Terminal ileostomy is often required for low rectal cancer surgery to prevent the occurrence of anastomotic leakage and protect the rectal anastomotic stoma. Patients require a second surgery for the closure of the stoma.
• We designed an intestine diversion duct. This double-balloon device can be inserted into the end ileum during the operation and removes the need for a second operation and reduces trauma.
What is the implication, and what should change now?
• The diversion tube removes the need for a second operation for patients with low rectal cancer and reduces the trauma and pain of patients. We will continue to examine its clinical application in subsequent experiments and optimize and improve the diversion tube to ensure the safety of its clinical application.
Introduction
Colorectal cancer is one of the most common malignant tumors and is the 3rd most common cancer worldwide (1). There are >1.2 million new cases of colorectal cancer every year worldwide, and about 600,000 patients die from colorectal cancer, making it the 4th leading cause of cancer-related deaths worldwide (1). Rectal cancer accounts for about 50–60% of all cancers in China, while low and super-low rectal cancer accounts for about 40–50%. Thus, rectal cancer represents a serious threat to people’s survival and health (2).
Surgery is the primary treatment for rectal cancer, and laparoscopic colorectal surgery is widely used in clinical settings. Total mesorectal excision, the development of laparoscopic techniques, the improvement of surgical instruments, and a rise in the technical level of surgeons have enhanced the rate of anus reservation for low rectal cancer significantly (3,4). However, the incidence of anastomotic leakage after rectal cancer is high, and leads to pelvic infection, sepsis, and even death in serious cases. For patients at high risk of anastomotic leakage, ileostomy is usually selected to reduce the occurrence of anastomotic leakage, and a second operation is then performed 6 months later. Stoma often places severe psychological and social pressure on the patient (5-9). Thus, a new technique or method is required.
Currently, a common catheter is usually placed into the end of ileum to divert the intestinal contents (10-12). There have been sporadic reports of diversion by catheter or tracheal catheter around the world, but presently, there is no special diversion tube for the ileum. The clinical products currently available have the following shortcomings: (I) they have poor flow conversion effects and cumbersome procedures; (II) they have limited side holes; (III) they are difficult to fix in the intestine; and (IV) they require cumbersome cleaning that leads to infection. Previously, a side hole with a one-way valve effect between the 2 airbags could not be developed, as the production process prevented the product from being released. Our research on an intestine diversion tube began in 2010. We used a catheter as the diversion tube and inserted it into the terminal ileum through the ileocecum to divert the intestinal contents (13). This tube is mainly used in anus preservation operations of low rectal cancer and temporary enterostomy for various traumas. An intestine diversion tube with a double-balloon was designed instead of the traditional tube or catheter. It removes the need for enterostomy and reduces the medical costs and patients’ burden. Pigs are closely related to humans, and their digestive system is very similar to that of humans. Thus, we chose experimental pigs as the research objects to verify the safety and effectiveness of the diversion tube. We present the following article in accordance with the ARRIVE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-1284/rc).
Methods
We designed an intestine diversion tube with a double-balloon without a stoma for rectal cancer surgery and conducted an animal experiment. This technology could greatly improve the quality of life of rectal cancer patients and have significant clinical application value. In the past 2 years, an intestine diversion tube with a double-balloon has finally been developed, and its use has been confirmed in animal experiments by 3 generations of sample testing. The relevant data from the animal experiments are shown in Table 1. The experimental results showed that the device has a number of advantages, including a high success rate of flow diversion and low complication rate. It not only removes the need for stoma in lower rectal cancer operations, but also has a simple procedure. The tube and method have no effect on postoperative bowel function of animals and human beings, without any side effects and damage. This method only carries on the diversion of intestinal contents without increasing any associated side effects.
Table 1
| Variables | Group | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Animal species | Pig | Pig | Pig | Pig | Pig |
| Sex (M/F) | M | F | M | F | M |
| Age (month) | 4 | 4.2 | 4.5 | 4 | 4.5 |
| Weight (kg) | 40 | 45 | 41 | 45 | 40 |
| Operation time (min) | 115 | 105 | 90 | 86 | 102 |
| Blood loss (mL) | 10 | 15 | 25 | 18 | 22 |
| Volume of drainage (mL) | 200 | 180 | 210 | 148 | 205 |
| Postoperative complications | N | N | N | N | N |
| Anastomotic leakage | N | N | N | N | N |
| Abdominal or pelvic infection | N | N | N | N | N |
| Anastomotic stenosis | N | N | N | N | N |
| Postoperative bleeding | N | N | N | N | N |
| Intestinal obstruction | N | N | N | N | N |
| Reoperation | N | N | N | N | N |
| Electrolyte disorder | N | N | N | N | N |
| Drainage tube blockage | N | N | Y | N | N |
| Drainage tube off | N | Y | N | N | N |
| Drainage tube removal time (d) | 14 | 11 | 14 | 14 | 14 |
| Time of first defecation (d) | 3 | 2 | 3 | 2 | 3 |
M, male; F, female; N, no; Y, yes.
A total of 5 experimental pigs [provided by Silver Snake (Shanghai) Medical Tech Ltd., Shanghai, China] were included in the experiment. The purpose of this study was to preliminarily verify the effectiveness and safety of the diversion tube. In our previous clinical studies, we used similar devices for clinical trials. The control group comprised ileostomy animals, but it was meaningless to set an ostomy control group in this experiment. Thus, only an experimental group was used in this study, and we selected 5 animals to verify the effectiveness of the tube, which was sufficient for the purpose of the experiment.
To be selected for inclusion in this study, the experimental pigs had to meet the following inclusion criteria: (I) be aged 4 to 6 months; (II) be healthy; (III) have no history of gastrointestinal surgery; (IV) be free of gastrointestinal and other special diseases; and (V) have normal eating and defecation habits. Pigs were excluded from the study if they met any of the following exclusion criteria: (I) had a previous history of gastrointestinal surgery; (II) had difficulty eating or defecating; and/or (III) could not tolerate surgery.
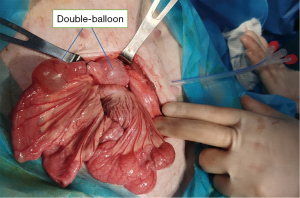
After general anesthesia and surgical antisepsis, a part of the rectum resection and anastomosis was finished. Next, the cecum was incised. An intestine diversion tube with a double-balloon [26 French (Fr)] was inserted into the ileum through the cecum of about 15 cm depth. The 2 balloons were injected with 8–12 mL of saline. An absorbable suture with a loose ligation between the balloon was used to prevent the tube entering the cecum (Figure 1). The end side of the tube was pulled out of the right lower abdominal wall, and the tube was fixed by the peritoneum. A drainage bag was connected to the end of the tube.
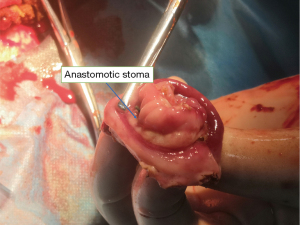
Tube drainage was recorded every 24 hours. After the recovery of intestinal function (exhaust or defecation), the fluid could be taken. The intestinal fluid or fecal juice could be discharged through the tube. About 2 weeks later, saline in the balloon was drawn out to restore the unobstructed of the ileum. If the pigs defecated normally 1–2 times and there was no fecal-like drainage fluid in the drainage tube around the anastomosis, the tube was removed because the anastomosis had healed. The wound was then spontaneously closed after 2–3 days. If a suspicious anastomotic fistula appeared when the saline in the balloon was drawn out, a further 6–10 mL of saline was injected into the balloon to reduce the colonic content until the anastomosis had healed. The animal experiments with 5 groups were all performed by the same group of physicians. All the pigs were operated on according to uniform standards and procedures, and uniform postoperative management was used to reduce any confounding bias. All the animals were anatomized after being anesthetized on the 14th day after the operation to check the anastomosis and abdominal cavity (Figure 2). During the experiment, a full-time staff member was responsible for animal feeding, and recording the data and observation indicators.
Experiments were performed under a project license (No. 202009003S) granted by Experimental Animal Science Department of Fudan University, in compliance with institutional guidelines for the care and use of animals. A protocol was prepared before the study without registration. The pigs were provided by Silver Snake (Shanghai) Medical Tech Ltd. [license number: SYXK(Shanghai)2017-0001]. The animals were white pigs, aged from 4–6 months, and weighing 35–50 kg. They were fed in a single cage in a common feeding mode. Their feed, drinking water, and daily activities were monitored each day.
Our experiments were conducted in accordance with Good Laboratory Practice and the Standard Operating Procedure. We also sought to reduce the use of animals in scientific research activities for the purpose of scientific research. An optimization method was employed to improve the quality of life of the animals and all feasible techniques and means were used to free them from the suffering, discomfort, and pain caused by the experiments and/or to improve their living environment. This study was carried out in strict accordance with the operation standards and principles for animal experiments. The disinfection of animal feed, bedding, and drinking water was the focus of the disinfection management, and space, table, equipment, and cage disinfection was performed to maintain good animal feed and experimental environment. The awareness of the standard operation of the laboratory animal personnel was performed by their contact with the animals and the various disinfectants and ultraviolet rays used during the work. Preoperative preparation, intraoperative management, and postoperative care were pay more attention to reduce the death of the experimental animals and protect the experimental animals. KCl (potassium chloride, 10%) was used to euthanize the pigs, and the specimens were properly disposed of at the last autopsy. In the study, adverse events, such as massive bleeding, infection, drainage tube loss, and death, were strictly recorded. During the operation and after the operation, 1 researcher monitored the vital signs, daily eating, defecation, and experimental index records of the pigs each day. If an accident had occurred, the experiment would have been terminated immediately and the animals treated in a timely manner.
Statistical analysis
Demographic data were compared using Student’s t-test for continuous variables and chi-square test for categorical variables. The qualitative variables were summarized by simple and relative frequencies. Quantitative variables were expressed as the median and interquartile interval. SPSS 26.0 was used in this study, and a P value <0.05 was considered statistically significant for the intra-group comparisons.
Results
The postoperative complications included anastomotic leakage, abdominal or pelvic infection, anastomotic stenosis, postoperative bleeding, intestinal obstruction, reoperation, electrolyte disorder, drainage tube blockage, and drainage tube fall off (Table 1). The average operation time was 99.6 minutes, the average intraoperative blood loss was 18 mL, the average daily drainage tube volume was 188.6 mL, the average drainage tube removal time was 13.4 days, and the average first defecation time was 2.6 days. One of the animals had a lumen blockage, which was unobstructed after saline irrigation without adverse events. The diverter tube fell off in 1 animal on the 11th day after surgery because the drainage tube had been improperly fixed and was pulled out of the body. The wound was sterilized and sutured. No adverse reactions were observed.
Discussion
The latest global estimates suggest that there are approximately 1 million new cases of colon and rectal cancer in men. In women, there are 800,000 new cases recorded, making it the second most common cancer. Colon and rectal cancers in men are the second most common cancers in the Southeast and Midwest. Rectal cancer is estimated to account for approximately 30% of all colorectal cancer cases, making it an important public health issue, in addition to being a cancer that requires complex and multidisciplinary treatment (13).
In relation to the diameter of the diverter tube, 18 F (French) catheters were used in 32 patients from 2004 to 2011, and the diverter effect was good without obstruction and any other related problems (14). Kuk et al. (15) reported on the postoperative anastomotic leakage of rectal cancer using a 30-Fr transrectal drainage tube (Sewoon Medical Co., Cheonan, Korea), and noted that the drainage was effective. Chen et al. (16) used a CLINY intestinal drainage tube [length: 300 cm; diameter; 16 Fr, channels: 3 (suction channel, injection channel, and balloon channel); air bags: 2 (1 front and 1 rear); Create Medic, Tokyo, Japan], in a clinical study of patients with adherent intestinal infarction. Tan et al. (17) used a small intestine drainage tube (length: 300 cm; Fr: 16 or 18). The front of the tube had a weighted tip, and it had an anterior balloon, and rear balloon. At the end of the tube, there was an anterior balloon valve (marked “F. Ball”), an air hole (marked “Vent”), and a rear balloon valve (marked “B. Ball”). We reviewed Medic Co., Ltd.’s (French) products related to intestinal double-lumen drainage tubes, all of which were 12–20 Fr models, and determined that the 26 Fr drainage tube was sufficient for intestinal drainage.
No associated obstruction was observed in the animal studies. In relation to the safety of the tube, there were no complications related to the drainage tubes in our experiment. In Sun et al.’s (18) study, 171 patients underwent transcecum catheterization ileostomy (TCI) to prevent anastomotic leakage. TCI is effective in preventing anastomotic leakage, is an alternative option to preventive ileostomy, and does not require secondary operation. TCI is safe and worthy of application. In relation to the effectiveness of the diverting tube, all the 5 tubes had smooth drainage after surgery, and no postoperative complications were caused by intestinal obstruction or anastomotic leakage.
We also considered the size and characteristics of the deflector balloon. Chen et al. (16) injected 20 mL of saline into the balloon. Tan et al. (17) used an intestinal drainage tube in patients with acute intestinal obstruction and injected 15 mL of saline into the balloon. The lumen capacity of intestine double-lumen drainage tubes varies from 15 to 60 cc depending on the type. In this experiment, 15 mL of saline was injected into the 2 air sacs, and no intestinal ischemia or necrosis occurred, which shows that the tube is safe. In relation to the side holes of the diverter tube, the diverter tube used in this experiment had 6 long round side holes (3.0 mm × 6.0 mm) and 4 one-way valve side holes (3.0 mm × 6.0 mm) between the double air bags, which increased the safety and diverter effects.
The diverter tube used in this experiment has the following advantages: (I) the double-balloon improves the diverter effect and intestinal fixation. When 1 of the air bags leaks or ruptures, the second air bag provides protection; (II) the use of multiple side holes prevents clogging, and the 4 one-way valve side holes between the air bags prevent reflux and enhance the effect of flow reversal; (III) the metal guide wire plays a guiding role in the operation; (IV) a cleaning brush can be used to keep the inner tube clean; (V) as no second operation is required, the patient’s physical and financial burdens are reduced; (VI) the incidence of anastomosis leakage is reduced; (VII) the procedure is simple. There was no postoperative complications, which included anastomotic leakage, abdominal or pelvic infection, anastomotic stenosis, postoperative bleeding, intestinal obstruction, reoperation, electrolyte disorder, drainage tube blockage and so on. This method can avoid ostomy and reduce the number of operations, which is beneficial to postoperative recovery and reduce surgical trauma.
This study had a number of shortcomings. For example, due to the limited number of animals in this study, our data does not have the accuracy of large-scale animal experimental data. Moreover, no control group was set up, and we conducted an observational animal experimental study and not a randomized controlled study. This study is an animal experiment; thus, clinical experiments need to be conducted.
In the future, we intend to continue to improve the quality and safety of the tube, and the expansion of animal experiments and quantitative verification are also required. We intend to carry out clinical trials in the future to better assess the needs of clinical patients.
Conclusions
The intestine diversion tube with a double-balloon was safe and effective in animal experiments. It removes the need for ostomy and reduces surgical trauma. It is a surgical tool and method worthy of clinical application.
Acknowledgments
Funding: This study was supported by the Science and Technology Commission of Shanghai Municipality (No. 20S31905000).
Footnote
Reporting Checklist: The authors have completed the ARRIVE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-1284/rc
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-1284/dss
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-1284/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-1284/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Experiments were performed under a project license (No. 202009003S) granted by Experimental Animal Science Department of Fudan University, in compliance with institutional guidelines for the care and use of animals.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Qiu H, Cao S, Xu R. Cancer incidence, mortality, and burden in China: a time-trend analysis and comparison with the United States and United Kingdom based on the global epidemiological data released in 2020. Cancer Commun (Lond) 2021;41:1037-48. [Crossref] [PubMed]
- Yang Z, Chunhua G, Huayan Y, et al. Anatomical basis for the choice of laparoscopic surgery for low rectal cancer through the pelvic imaging data-a cohort study. World J Surg Oncol 2018;16:199. [Crossref] [PubMed]
- Sun Y, Wu G, Zhang B, et al. Clinical control study of laparoscopic versus open surgery for rectal cancer. Zhonghua Wei Chang Wai Ke Za Zhi 2014;17:369-72.
- Zhao S, Zhang L, Gao F, et al. Transanal Drainage Tube Use for Preventing Anastomotic Leakage After Laparoscopic Low Anterior Resection in Patients With Rectal Cancer: A Randomized Clinical Trial. JAMA Surg 2021;156:1151-8. [Crossref] [PubMed]
- Matsuda M, Tsuruta M, Hasegawa H, et al. Transanal drainage tube placement to prevent anastomotic leakage following colorectal cancer surgery with double stapling reconstruction. Surg Today 2016;46:613-20. [Crossref] [PubMed]
- Nishizawa Y, Nishigori H, Tsukada Y, et al. A multicentre confirmatory single-arm trial of the safety and efficacy of a transanal drain for prevention of anastomotic leakage after surgery for rectal cancer. Colorectal Dis 2021;23:3196-204. [Crossref] [PubMed]
- Zhang JS, Kong C, Li L. Endoscopic Decompression with a Transanal Drainage Tube for the Treatment of Hirschsprung's Disease in Newborns. J Laparoendosc Adv Surg Tech A 2021;31:959-63. [Crossref] [PubMed]
- Wang YJ, Han ZC, Chen L, et al. Clinical Efficacy of an Indwelling Transanal Tube for the Prevention of Anastomotic Leakage After Hirschsprung's Disease: A Single Center Experience with Chinese Patients. J Laparoendosc Adv Surg Tech A 2022;32:342-6. [Crossref] [PubMed]
- Boccola MA, Lin J, Rozen WM, et al. Reducing anastomotic leakage in oncologic colorectal surgery: an evidence-based review. Anticancer Res 2010;30:601-7.
- Montedori A, Cirocchi R, Farinella E, et al. Covering ileo- or colostomy in anterior resection for rectal carcinoma. Cochrane Database Syst Rev 2010;CD006878. [Crossref] [PubMed]
- Rullier E, Le Toux N, Laurent C, et al. Loop ileostomy versus loop colostomy for defunctioning low anastomoses during rectal cancer surgery. World J Surg 2001;25:274-7; discussion 277-8. [Crossref] [PubMed]
- Valadão M, Cesar D, Véo CAR, et al. Brazilian society of surgical oncology: Guidelines for the surgical treatment of mid-low rectal cancer. J Surg Oncol 2022;125:194-216. [Crossref] [PubMed]
- Zhao J, Cai Y, Cheng Z, et al. Application of selective transcecum tube ileostomy for protecting anastomotic stoma with high risk in colorectal. J Surg Concepts Pract 2012;17:5.
- Kuk JC, Lim DR, Shin EJ. Effect of transanal drainage tube on anastomotic leakage following low anterior resection for rectal cancer without a defunctioning stoma. Asian J Surg 2022;45:2639-44. [Crossref] [PubMed]
- Chen XL, Ji F, Lin Q, et al. A prospective randomized trial of transnasal ileus tube vs nasogastric tube for adhesive small bowel obstruction. World J Gastroenterol 2012;18:1968-74. [Crossref] [PubMed]
- Tan Y, Chen H, Mao W, et al. Short-Term Clinical Outcomes after Using Novel Deeper Intubation Technique (DIT) of Ileus Tube for Acute Bowel Obstruction Patients. Gastroenterol Res Pract 2020;2020:1625154. [Crossref] [PubMed]
- Sun H, He Y, Li X, et al. Transcecum catheterization ileostomy is safe and effective to prevent anastomotic leakage in post-laparoscopic rectal cancer surgery: a single-center retrospective study. J Gastrointest Oncol 2022;13:1818-31. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)


