
Impact of caregiver burden on caregiver mental health in patients with esophageal cancer: chain mediating effects of benefit finding and rumination, a cross-sectional study
Introduction
According to estimates, esophageal cancer is the sixth most frequent cancer in the world and the ninth most common cause of cancer-related deaths (1). China has a high incidence of esophageal cancer, accounting for 53.7% of new cases and 55.7% of deaths in the world (2). The results of the annual report of the Chinese tumor registry showed that the incidence rate of esophageal cancer in China reached 13.9/100,000 and the mortality rate reached 12.7/100,000 in 2015 (3). It ranks 6th and 4th in the spectrum of malignant tumor incidence and death in China, respectively (4). The degree of prognosis of patients with esophageal cancer is not optimistic, with 5-year survival rate not exceeding 20% (5).
A cancer diagnosis can have a huge impact not only on an individual patient, but also on the entire family. esophageal cancer patients often suffer from reflux, wasting and malnutrition (6). The long-term and repeated treatment process can impose a heavy burden, economic pressure, and psychological pressure to patients and their families [such as anxiety, depression (7,8)]. Multiple studies have shown that caregiver burden and mental health status can affect the quality of care caregivers provide to patients (9,10), which in turn affects patient recovery. Previous studies of caregivers of patients with esophageal cancer have reported significant levels of psychological distress (11,12), that 30% of caregivers had moderate/high anxiety, 10% had moderate/high depression, and a fairly high level of fear of re-occurrence. Regression analysis showed that the variables evaluated (illness, cognition, and coping) accounted for 35–49% of the variance in caregiver psychological distress in a research of 382 family carers of patients with esophageal cancer (12).
Previous researches (13,14) have found that some caregivers experience not only negative emotions but also positive psychological experiences when caring for cancer patients. The caregivers’ mental health is greatly affected their nursing quality, a negative mental condition would reduce their patience, and resulted in a worse service, while a positive emotion can bring a more careful take care, and eventually affected the patient’s life quality. The mental health of tumor patients are greatly noticed by the researchers for it obviously affected the mortality rate, Less study has been done on the mental health of those who care for someone with esophageal cancer, though. The positive factors that affecting the caregivers mental health should be carefully studied to maintain the caregivers’ mental health and promote their service quality and benefit the patients. Antoni et al. (15) define this positive personal change, benefit finding, as a reappraisal and positive change in an individual’s perception of a negative event after experiencing a stressful or negative life event. Previous research has found that positive coping, positive reappraisal, optimism, social support (16,17), and social constraints (18) are significantly associated with these positive changes. Benefit finding has indirect effects on mental health by finding positive meaning for events (19).
Rumination (20) refers to the cognitive process of an individual after experiencing a significant stressful life event, where the experience of a stressful event requires the individual to engage in cognitive activities with the purpose of better understanding the event. Rumination related to specific events is thought to play 2 possible roles. The more destructive form, namely intrusive rumination, manifests itself as thoughts that appear automatically beyond the control of the individual and are also unrelated to attempts to solve the problem. The second form, referred to as deliberate, reflective, or intentional rumination, is a form of constructive rumination that is thought perform two potential functions. Intrusive rumination, which is more harmful, appears as automatic thoughts that come to mind without one’s conscious control and are also unconnected to efforts to fix the issue. The second type of rumination is regarded to be more helpful and is referred to as deliberate, introspective, or intentional rumination (21). The process of addressing the difference between the unfavorable event experience and the collapse of basic beliefs includes intrusive on negative incident. Deliberate rumination, on the other hand, can assist individuals in making meaning of trauma, integrating new understandings into their beliefs, and processing the powerful emotions created by the experienced event between the experience of the unfavorable event and the collapse of basic beliefs. In turn, deliberate rumination can help individuals make meaning of the trauma and incorporate new ideas into their beliefs while dealing with the negative emotions caused by the experienced event (22). The first to emerge was intrusive rumination, which was perceived as a direct response to the negative events experienced. Later, purposeful rumination became more crucial, since it allowed individuals to retake control of the situation and establish coping strategies. Rumination appears to be especially crucial in the start of constructive transformation following a negative incident. Several studies have shown a positive correlation between rumination, especially intentional rumination, and the onset of positive self-growth. This kind of positive correlation has been noted in women with cancer (23), as well as others (24) who have experienced various forms of cancer. Multiple studies (25-27) have explored the effects of rumination on posttraumatic growth (PTG), showing that rumination after a traumatic event can promote PTG, and deliberate rumination is thought to restore the traumatic event and rebuild personal belief on the world (28). The 2 concepts of BF and PTG share related characteristics, so the terms are often used interchangeably (16,29-31).
Multiple studies (28,32) have found that good cognitive processing of stressful events can promote effective individual coping. Fletcher et al. (33) established “The Cancer Family Caregiving Experience Model” for caregivers. This model believes that in the dynamic change trajectory of cancer, the diagnosis of cancer initiates the individual’s cognitive evaluation and coping process of stress. When the caregiver adopts a positive way to deal with stress, it will lead to individual physical and mental health and well-being.
According to “The Cancer Family Caregiving Experience Model”, the primary stressor is the burden placed on cancer family carers, while the individual’s cognition and coping style serve as mediating factors and the caregiver’s physical and mental health and well-being as outcome variables. Previous research has revealed a relationship between benefit finding and intrusive thinking (18), but the mechanisms of how benefit finding and rumination affect caregiver burden and mental health have not been elucidated. Therefore, this study explores the chain mediating effect of benefit finding and rumination on caregiver burden and mental health, and provides theoretical support for carrying out caregiver mental health intervention. We present the following article in accordance with the STROBE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-884/rc).
Methods
Study design and participants
Cross-sectional, descriptive, and correlational designs were used in this investigation. From May 2020 to December 2020, esophageal cancer patients who were hospitalized in the oncology department and cardiothoracic surgery department of 2 tertiary hospitals (The Third Affiliated Hospital of Soochow University and Affiliated Hospital of Jiangnan University) in Jiangsu Province, as well as their family care members, were chosen for the survey.
The inclusion criteria for patients and caregivers were as follows: (I) patients with primary esophageal cancer diagnosed by pathology; (II) caregiver age ≥18 years old; (III) the patient’s primary caregiver cares for ≥4 hours/day and has cared for the patient for at least ≥4 weeks; (IV) the caregiver has no mental illness or intellectual disability, and has normal language expression and reading.
The following were the exclusion criteria: (I) Patients with end-stage cancer or other critical illnesses, such as renal failure, respiratory failure; (II) the caregiver and patient have an employment relationship; (III) the caregiver has a serious medical condition (e.g,, malignancy, depression.); (IV) patients and caregivers are being investigated in other research.
GPower software was used to calculate sample size (version 3.1.9). With 134 responses, the sample size has a 95.1% validity rate, a 0.3 effect size, and a 5% significance level (two-sided) (34). This study was carried out in two tertiary hospitals, in Jiangsu Province, China, in which 202 patients and caregivers were consented to engage (the response rate was 89.1%), and 180 questionnaires were finally returned. The research team evaluated the validity of the questionnaires gathered that day and distributed all of them to team members who had received questionnaire management training for safekeeping. The research team evaluated the questionnaires, and there were 166 valid complete questionnaires (the effective rate was 92.2%).
The members of the study team were mainly nursing graduate students, and the team received relevant training for 1 week before the start of the study, including the research background, purpose, and significance. Researchers read relevant medical records, selected eligible patients, and helped participants who had difficulty reading questionnaires. The researcher explained the purpose of the investigation to the respondents, and all were told to voluntarily participate in the study and to withdraw from the study at any time without affecting the care of the participants.
This study follows the Declaration of Helsinki (as revised in 2013) (35) and adheres to the principles of informed consent, security protection, privacy and confidentiality, and fairness and transparency. The study was approved by the ethics committees of the Third Affiliated Hospital of Soochow University (No. 2020-CL003-01) and the Affiliated Hospital of Jiangnan University (No. LS2020010). All participants gave informed consent before participation.
Measures
The researchers reviewed the literature and set up group discussions, mainly to investigate the demographic data of patients and caregivers such as gender, age, education level, family economic status, relationship with patients. Simultaneous collection of clinical data from patients was performed, including the stage of cancer.
This study adopted the Chinese version of the revised version of the Benefit Finding Scale (BFS) (36) to assess caregivers’ BFS scores. The scale has 22 items in 5 dimensions, including acceptance (3 items), family relationships (6 items), personal growth (7 items), social relations (3 items), and health behaviors (3 items). The Likert 5-level scoring method was used, and the score ranged from 22 to 110 points. The scores of each dimension were added to obtain the total score of the scale. The total score of the scale is the sum of the scores for each of its dimensions. A higher overall score indicates a greater degree of benefit finding for the carer. The Chinese version of the scale has good reliability and validity, the Cronbach’s coefficient of the total scale is 0.933, and it has been validated in cancer family caregivers (36).
This study adopted the Chinese version of the Event-Related Rumination Inventory (ERRI) to assess the rumination levels of caregivers. The questionnaire has 20 items, including 2 dimensions: intrusive rumination and deliberate rumination. Intrusive rumination can lead to individual psychological distress and hinder growth thinking. Deliberate rumination promotes individual active thinking and adaptive thinking for growth. A total of 20 items on a four-point scale, with from zero to three representing “not at all,” “sometimes,” “often,” and “almost always” respectively. The higher the score, the higher the individual’s tendency to rumination. The Chinese version of ERRI was validated and had reliable reliability (37).
The level of caregiver burden was evaluated using the Zarit Burden Interview (ZBI) (38) 22 items total, with two dimensions—personal burden and responsibility burden—are included in the questionnaire. A score of <21 indicates no burden or a mild burden, a score of 21–39 indicates a moderate burden, and a score of ≥40 indicates a severe burden on each scale, which includes five grades from 0 (none) to 4 (always) (39). The Chinese version of the ZBI has good reliability and validity for caregiver burden surveys, and the Cronbach’s coefficient of the scale is 0.86 (40).
The mental health of caregivers was assessed using the Hospital Anxiety and Depression Scale (HADS) (41). It consists of 14 items, 7 of which are used to assess anxiety (HADS-A) and 7 of which are used to assess depression (HADS-D). Each item is scored on a 4-point scale from 0 to 3. The Cronbach’s coefficients for the anxiety and depression subscales of the Chinese version of the HADS were 0.83 and 0.82, respectively (42). For both HADS-A and HADS-D, we divided respondents into subgroups by using a ≥9-point depression or anxiety cut-off to define pathological and non-pathological values, as suggested in a previous study (43).
Statistical analysis
IBM’s SPSS 26.0 software was used to analyze the data, and the results of common method bias (44) were examined using the Harman one-way test, which indicates a serious common bias if one factor explains more than 50% (45) of the common variance (the result is 33.3%). Measurement data conforming to a normal distribution are expressed as (Mean ± SD), and count data were described using frequency and composition ratios. Bivariate relationships between variables were detected using Pearson correlation analysis. The method of testing mediation uses the currently recommended bias-corrected percentile bootstrap method for testing the hypothesized chain mediation model. Chain mediated effect implementation (Model 6, the Process Macro) (46) was performed by repeated sampling 5,000 times and 95% corrected confidence interval (CI) methods. Mediated effects are considered statistically significant if the 95% bootstrap CI for the indirect effect does not contain zero (47,48). The direct effect is that the independent variable direct affect the dependent variable, and when the 95% confidence interval of bootstrap test does not include 0, the effect is valid. The indirect effect is that the independent variable has an effect on the dependent variable through the intermediary variable, and when the 95% confidence interval does not include 0 via the bootstrap method, the indirect effect is valid.
Study hypothesis
Intrusive rumination and deliberate rumination reflect negative and positive cognitive processes, respectively. Therefore, we divided rumination into 2 variables, namely intrusive rumination and deliberate rumination, to test for chain mediated effects. We also established 2 chain mediated models with caregiver burden as the independent variable (X), caregiver anxiety and depression as the dependent variable (Y), caregiver deliberate rumination/intrusive rumination as the 1st mediating variable (M1), and caregiver’s benefit finding as the 2nd mediating variable (M2). In addition, we used caregiver education level and patient cancer stage as covariates in the chain mediating model.
Results
Participant characteristics
In this study, data were collected from 166 pairs of hospitalized patients with esophageal cancer and their caregivers. The mean age of the caregivers was 59.96±11.48 years, the caregivers were predominantly women [142 (85.5%)], the majority of the caregivers had secondary school education or less [122 (73.5%)], and the caregivers were mostly spouses of the patients [130 (78.3%)], as shown in Table 1. The analysis showed that mean value of the overall ZBI was 31.39±9.99, as shown in Table 2.
Table 1
| Category | Value |
|---|---|
| Gender, n (%) | |
| Male | 24 (14.5) |
| Female | 142 (85.5) |
| Mean age (years), mean ± SD | 59.96±11.48 |
| <40, n (%) | 13 (7.8) |
| 40–60, n (%) | 57 (34.3) |
| >60, n (%) | 96 (57.8) |
| Education levels, n (%) | |
| Primary school and below | 69 (41.6) |
| Junior school | 53 (31.9) |
| High school | 20 (12.0) |
| Diploma and above | 24 (14.5) |
| Relationship with patients, n (%) | |
| Spouse | 130 (78.3) |
| Offspring | 31 (18.7) |
| Other | 5 (3.0) |
| Other caregiver, n (%) | |
| None | 74 (44.6) |
| 1 | 75 (45.2) |
| ≥2 | 17 (10.2) |
| Having chronic diseases, n (%) | |
| None | 92 (55.4) |
| One kind | 50 (30.1) |
| Two kind and above | 24 (14.5) |
| Per capita monthly income (CNY), n (%) | |
| 1,000–3,000 | 85 (51.2) |
| 3,001–5,000 | 33 (19.9) |
| 5,001–8,000 | 31 (18.7) |
| 8,001–10,000 | 11 (6.6) |
| >10,000 | 6 (3.6) |
CNY, China yuan.
Table 2
| Variables | Scores (mean ± SD) | ZBI | Intrusive rumination | Deliberate rumination | BFS | HADS |
|---|---|---|---|---|---|---|
| ZBI | 31.39±9.99 | 1 | ||||
| Intrusive rumination | 16.61±6.50 | 0.858** | 1 | |||
| Deliberate rumination | 16.46±7.16 | −0.879** | −0.948** | 1 | ||
| BFS | 73.92±18.12 | −0.873** | −0.901** | 0.904** | 1 | |
| HADS | 13.98±6.09 | 0.822** | 0.748** | −0.758** | −0.782** | 1 |
**, P<0.01 (two-tailed). ZBI, Zarit Burden Interview; BFS, Benefit Finding Scale; HADS, Hospital Anxiety and Depression Scale.
Pearson correlation analysis
Pearson correlation analysis showed a positive correlation between ZBI and HADS (r=0.882, P<0.01), such that caregivers who scored higher on ZBI reported greater HADS. Further, a negative correlation between ZBI and BFS (r=−0.873, P<0.01). Intrusive rumination and BFS scores in caregivers were negatively correlated (r=−0.901, P<0.01), while deliberate rumination and BFS scores in caregivers were positively correlated (r=0.904, P<0.01). All specific data are listed in Table 2.
Mediation effects analysis
To determine the role of rumination and benefit finding in the chain mediating between caregiver burden and caregiver mental health, the implementation method was bias-corrected percentile Bootstrap (5,000 replicate samples).
Chain mediation effects 1
The findings in Figure 1 demonstrate a statistically significant overall impact of caregiver burden on caregiver anxiety and depression (c=0.5011, P<0.01), the direct effect of the path was c’=0.3564 (P<0.01), and the effect of caregiver intrusive rumination on caregiver benefit finding was negative (β=−1.6138, P<0.01).
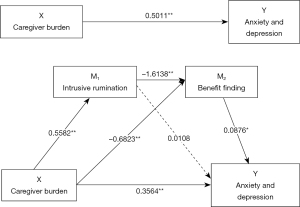
As shown in Table 3, the path of the single mediating variable M1 [intrusive rumination; point estimate =0.006; 95% Bias-corrected confidence interval (95% BC CI): −0.1065, 0.1171] was not statistically significant and the path of the single mediating variable M2 (benefit finding; point estimate =0.0598; 95% BC CI: 0.0093, 0.1201) was statistically significant. In addition, the pathway of intrusive rumination and benefit finding as a chain mediating effect of caregiver burden on caregiver anxiety and depression was statistically significant (point estimate =0.0789; 95% BC CI: 0.0138, 0.1551).
Table 3
| Effect | Product of coefficients | Bootstrap 95% CI | |||
|---|---|---|---|---|---|
| Point estimate | Boot SE | Boot LL (CI) | Boot UL (CI) | ||
| Total indirect effect of X on Y | 0.1447 | 0.0539 | 0.0427 | 0.2512 | |
| Indirect effect 1: X→M1→Y | 0.006 | 0.0569 | −0.1065 | 0.1171 | |
| Indirect effect 2: X→M2→Y | 0.0598 | 0.0278 | 0.0093 | 0.1201 | |
| Indirect effect 3: X→M1→M2→Y | 0.0789 | 0.0354 | 0.0138 | 0.1551 | |
Number of bootstrap samples for bias corrected bootstrap confidence intervals: 5,000. Level of confidence for all confidence intervals: 95%. X = caregiver burden; M1 = intrusive rumination; M2 = benefit finding; Y = anxiety depression; SE, standard error; LL, lower limit; UL, upper limit; CI, confidence interval.
Chain mediation effects 2
The results in Figure 2 show that the total effect of caregiver burden on caregiver anxiety and depression was statistically significant (c=0.5011, P<0.01), and the direct effect of the path was c’=0.3607 (P<0.01). This result is the same as the result of model 1. Caregiver deliberate rumination had a positive effect on the benefit finding of caregivers (β=1.5237, P<0.01).
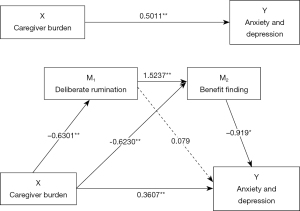
As shown in Table 4, the path of the single mediating variable M1 (deliberate rumination; point estimate =−0.005; 95% BC CI: −0.1167, 0.1059) was not statistically significant and the path of the single mediating variable M2 (benefit finding; point estimate =0.0572; 95% BC CI: 0.01, 0.1125) was statistically significant. In addition, the pathway of deliberate rumination and benefit finding as a chain mediating effect of caregiver burden on caregiver anxiety and depression was statistically significant (point estimate =0.0882; 95% BC CI: 0.0167, 0.171).
Table 4
| Effect | Product of coefficients | Bootstrap 95% CI | |||
|---|---|---|---|---|---|
| Point estimate | Boot SE | Boot LL (CI) | Boot UL (CI) | ||
| Total indirect effect of X on Y | 0.1405 | 0.0532 | 0.0374 | 0.2467 | |
| Indirect effect 1: X→M1→Y | −0.005 | 0.0574 | −0.1167 | 0.1059 | |
| Indirect effect 2: X→M2→Y | 0.0572 | 0.0263 | 0.01 | 0.1125 | |
| Indirect effect 3: X→M1→M2→Y | 0.0882 | 0.0391 | 0.0167 | 0.171 | |
Number of bootstrap samples for bias corrected bootstrap confidence intervals: 5,000. Level of confidence for all confidence intervals: 95%. X = caregiver burden; M1 = deliberate rumination; M2 = benefit finding; Y = anxiety depression. SE, standard error; LL, lower limit; UL, upper limit; CI, confidence interval.
Discussion
Using the conceptual “model of cancer family caregiving experience” (33) as a theoretical basis (33), this study investigated the direct relationship and pathways of influence between caregiver burden and caregiver mental health in caregivers of Chinese patients with esophageal cancer. The impacts of caregiver burden, rumination, and benefit finding on caregiver anxiety and depression were investigated using a chain mediation model. The findings support the theoretical hypothesis and validate the mediating role of rumination and benefit finding in the relationship between caregiver burden and mental health.
The results of this study showed that the benefit finding of caregivers was a mediating variable of caregiver burden and caregiver mental health. Family caregivers of multiple cancer patients reported (49,50) changes in individual cognitive behaviors in response to negative events while accompanying cancer patients during treatment: appreciation and acceptance of life, improved interpersonal relationships, spiritual growth, and improved health behaviors. Benefit finding as a cognitive-behavioral process for individuals to cope with stress and negative events can help individuals to re-build positive coping mechanisms (14,51,52). Studies on caregivers of esophageal cancer suggested (12,53) that family caregivers of esophageal cancer survivors may benefit from cognitive-based therapies by alleviating their emotional turmoil. The results of previous intervention studies have shown that health care professionals can use meaning-centered psychotherapy (54), cognitive-behavioral stress management intervention (55), brief writing intervention (56), and guided self-disclosure intervention (57) to increase the benefit finding of caregivers, reduce caregiver burden, and promote caregiver mental health.
The relationship between caregiver burden and caregiver psychological wellbeing is mediated by caregiver rumination and benefit finding. Cognitive processing (rumination) is considered an important part of the process of coping with negative events, and rumination is recurrent, event-related thinking (37) that includes comprehension, problem solving, recall, and anticipation. In the early stages of experiencing a stressful event, rumination is often automatic and intrusive, evoking negative emotions (37). The diagnosis of cancer triggers the stress coping process, and cognitive process, thus enhances the deliberate rumination of caregivers, such as why their beloved suffers from cancer, how it will affect their future family life, and feelings about the experience. When this kind of cognitive processing develops over time, intrusive rumination is gradually replaced by deliberate rumination, which incorporates the traumatic event into the cognitive schematic structure, constructive reconstruction of the stressful event (58), and caregivers develop new worldviews and goals to adapt to the consequences caused by the illness, implying that they acquire positive changes (37). According to the findings of a survey of cancer patients and their caregivers (58), the spouses of patients experienced higher levels of psychological discomfort and intrusive thoughts than the patients themselves. Influenced by the traditional Chinese culture and the concept of filial piety (59), caring for cancer patients is an unshirkable responsibility of family members even if the caregivers themselves have health problems or face various difficulties. In particular, in caring for patients, caregivers tend to put the patient’s needs above their own (60). In this study, most of the caregivers were the patients’ spouses, and the patients’ spouses were intimate partners (61) who cared for and accompanied the patients for a long time. Family support plays an important role in the disease treatment process, and when patients and spouses cope with stressful events together, stress perceptions are reciprocal, and joint positive coping by both spouses helps buffer the impact of stressful events. Studies have found that effective self-analysis (32) and timely self-disclosure (57) of stressful events can effectively facilitate gradual changes in cognitive processes from intrusive rumination to deliberate rumination. Medical professionals can intervene with patients and their spouses (62-64) to help improve caregivers’ negative emotions and promote positive adaptation and coping. The shortcoming of this study was that, it was a cross-sectional study and can not answer the clinical question of mediating roles of variables including the chain mediating relationships, while it suggested that the proposed mechanism in that buffering against negative emotions (anxiety, depression) is an approach in which benefit finding and rumination may play important roles. Our study provided descriptive information in this fields and raised the concerns of caregivers’ mental health.
Conclusions
The present study confirms that rumination and benefit finding play a chain mediating role in family caregiver burden and caregiver mental health. Rumination, as an individual’s cognitive process in response to a traumatic negative event, facilitates the generation of positive ways of coping, rearranging life, and deciding on priorities. Medical professionals can provide caregivers of cancer patients with measures based on rumination to promote positive coping and improve quality of life and psychological well-being, which has important implications for clinical practice.
Acknowledgments
We thank all the patients and their caregivers who participated in this study.
Funding: This study was funded by the Wuxi Grant (No. MS201945).
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-884/rc
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-884/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-884/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. This study follows the Declaration of Helsinki (as revised in 2013) and adheres to the principles of informed consent, security protection, privacy and confidentiality, and fairness and transparency. The study was approved by the ethics committees of The Third Affiliated Hospital of Soochow University (No. 2020-CL003-01) and the Affiliated Hospital of Jiangnan University (No. LS2020010). All participants gave informed consent before participation.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ohmori M, Ishihara R, Morishima T, et al. Excessive risk of second-cancer incidence and cancer mortality in patients with esophageal cancer. J Gastroenterol 2021;56:434-41. [Crossref] [PubMed]
- Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394-424. [Crossref] [PubMed]
- He F, Wang J, Liu L, et al. Esophageal cancer: trends in incidence and mortality in China from 2005 to 2015. Cancer Med 2021;10:1839-47. [Crossref] [PubMed]
- Mao YS, Gao SG, Wang Q, et al. Epidemiological characteristic and current status of surgical treatment for esophageal cancer by analysis of national registry database. Zhonghua Zhong Liu Za Zhi 2020;42:228-33. [PubMed]
- Merkow RP, Bilimoria KY, Keswani RN, et al. Treatment trends, risk of lymph node metastasis, and outcomes for localized esophageal cancer. J Natl Cancer Inst 2014;106:dju133. [Crossref] [PubMed]
- Lagergren J, Smyth E, Cunningham D, et al. Oesophageal cancer. Lancet 2017;390:2383-96. [Crossref] [PubMed]
- Donnelly M, Anderson LA, Johnston BT, et al. Oesophageal cancer: caregiver mental health and strain. Psychooncology 2008;17:1196-201. [Crossref] [PubMed]
- Haj Mohammad N, Walter AW, van Oijen MG, et al. Burden of spousal caregivers of stage II and III esophageal cancer survivors 3 years after treatment with curative intent. Support Care Cancer 2015;23:3589-98. [Crossref] [PubMed]
- Li Q, Lin Y, Xu Y, et al. The impact of depression and anxiety on quality of life in Chinese cancer patient-family caregiver dyads, a cross-sectional study. Health Qual Life Outcomes 2018;16:230. [Crossref] [PubMed]
- Best AL, Shukla R, Adamu AM, et al. Impact of caregivers' negative response to cancer on long-term survivors' quality of life. Support Care Cancer 2021;29:679-86. [Crossref] [PubMed]
- Graham-Wisener L, Collins L, Hanna J, et al. The need for enhanced psychological support in esophageal cancer-an exploratory study of the perception of HCPs, patients, and carers. Dis Esophagus 2019;32:doy076. [Crossref] [PubMed]
- Dempster M, McCorry NK, Brennan E, et al. Psychological distress among family carers of oesophageal cancer survivors: the role of illness cognitions and coping. Psychooncology 2011;20:698-705. [Crossref] [PubMed]
- Xiaoyun C, Fenglan L. The relationships among insecure attachment, social support and psychological experiences in family caregivers of cancer inpatients. Eur J Oncol Nurs 2020;44:101691. [Crossref] [PubMed]
- Li Q, Loke AY. The positive aspects of caregiving for cancer patients: a critical review of the literature and directions for future research. Psychooncology 2013;22:2399-407. [Crossref] [PubMed]
- Antoni MH, Lehman JM, Kilbourn KM, et al. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychol 2001;20:20-32. [Crossref] [PubMed]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. J Consult Clin Psychol 2006;74:797-816. [Crossref] [PubMed]
- Sears SR, Stanton AL, Danoff-Burg S. The yellow brick road and the emerald city: benefit finding, positive reappraisal coping and posttraumatic growth in women with early-stage breast cancer. Health Psychol 2003;22:487-97. [Crossref] [PubMed]
- Dunn J, Occhipinti S, Campbell A, et al. Benefit finding after cancer: the role of optimism, intrusive thinking and social environment. J Health Psychol 2011;16:169-77. [Crossref] [PubMed]
- McLennon SM, Habermann B, Rice M. Finding meaning as a mediator of burden on the health of caregivers of spouses with dementia. Aging Ment Health 2011;15:522-30. [Crossref] [PubMed]
- Kiełb K, Bargiel-Matusiewicz KM, Pisula E. Posttraumatic Stress Symptoms and Posttraumatic Growth in Mothers of Children With Intellectual Disability - The Role of Intrusive and Deliberate Ruminations: A Preliminary Report. Front Psychol 2019;10:2011. [Crossref] [PubMed]
- Cann A, Calhoun LG, Tedeschi RG, et al. Assessing posttraumatic cognitive processes: the Event Related Rumination Inventory. Anxiety Stress Coping 2011;24:137-56. [Crossref] [PubMed]
- Ogińska-Bulik N, Kobylarczyk M. The role of rumination in posttraumatic growth in people struggling with cancer. J Psychosoc Oncol 2019;37:652-64. [Crossref] [PubMed]
- Chan MW, Ho SM, Tedeschi RG, et al. The valence of attentional bias and cancer-related rumination in posttraumatic stress and posttraumatic growth among women with breast cancer. Psychooncology 2011;20:544-52. [Crossref] [PubMed]
- Morris BA, Shakespeare-Finch J. Rumination, post-traumatic growth, and distress: structural equation modelling with cancer survivors. Psychooncology 2011;20:1176-83. [Crossref] [PubMed]
- Lianchao A, Tingting M. Mindfulness, rumination and post-traumatic growth in a Chinese cancer sample. Psychol Health Med 2020;25:37-44. [Crossref] [PubMed]
- Koutrouli N, Anagnostopoulos F, Griva F, et al. Exploring the relationship between posttraumatic growth, cognitive processing, psychological distress, and social constraints in a sample of breast cancer patients. Women Health 2016;56:650-67. [Crossref] [PubMed]
- Soo H, Sherman KA. Rumination, psychological distress and post-traumatic growth in women diagnosed with breast cancer. Psychooncology 2015;24:70-9. [Crossref] [PubMed]
- Huh HJ, Kim KH, Lee HK, et al. Attachment Style, Complicated Grief and Post-Traumatic Growth in Traumatic Loss: The Role of Intrusive and Deliberate Rumination. Psychiatry Investig 2020;17:636-44. [Crossref] [PubMed]
- Sawyer A, Ayers S, Field AP. Posttraumatic growth and adjustment among individuals with cancer or HIV/AIDS: a meta-analysis. Clin Psychol Rev 2010;30:436-47. [Crossref] [PubMed]
- Shand LK, Cowlishaw S, Brooker JE, et al. Correlates of post-traumatic stress symptoms and growth in cancer patients: a systematic review and meta-analysis. Psychooncology 2015;24:624-34. [Crossref] [PubMed]
- Harding S, Sanipour F, Moss T. Existence of benefit finding and posttraumatic growth in people treated for head and neck cancer: a systematic review. PeerJ 2014;2:e256. [Crossref] [PubMed]
- Hirooka K, Fukahori H, Taku K, et al. Quality of death, rumination, and posttraumatic growth among bereaved family members of cancer patients in home palliative care. Psychooncology 2017;26:2168-74. [Crossref] [PubMed]
- Fletcher BS, Miaskowski C, Given B, et al. The cancer family caregiving experience: an updated and expanded conceptual model. Eur J Oncol Nurs 2012;16:387-98. [Crossref] [PubMed]
- Torres GCS, Relf MV, Tuazon JA. The mediating role of pre-operative patient readiness on surgical outcomes: A structural equation model analysis. J Adv Nurs 2020;76:1371-83. [Crossref] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191-4. [Crossref] [PubMed]
- Wen X, Wang D, Li N, et al. The construction of the structural equation model of burden, benefit finding, and anxiety-depression of esophageal cancer caregivers based on Lazarus stress and coping theory. Ann Palliat Med 2021;10:7644-52. [Crossref] [PubMed]
- Peng ZY, Wan LH. Posttraumatic Growth of Stroke Survivors and Its Correlation With Rumination and Social Support. J Neurosci Nurs 2018;50:252-7. [Crossref] [PubMed]
- Zarit SH, Femia EE, Kim K, et al. The structure of risk factors and outcomes for family caregivers: implications for assessment and treatment. Aging Ment Health 2010;14:220-31. [Crossref] [PubMed]
- Lu L, Wang L, Yang X, et al. Zarit Caregiver Burden Interview: development, reliability and validity of the Chinese version. Psychiatry Clin Neurosci 2009;63:730-4. [Crossref] [PubMed]
- Zhao M, Zhu Z, Kong C, et al. Caregiver burden and parenting stress among left-behind elderly individuals in rural China: a cross-sectional study. BMC Public Health 2021;21:846. [Crossref] [PubMed]
- Olssøn I, Mykletun A, Dahl AA. The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry 2005;5:46. [Crossref] [PubMed]
- Li Q, Lin Y, Hu C, et al. The Chinese version of hospital anxiety and depression scale: Psychometric properties in Chinese cancer patients and their family caregivers. Eur J Oncol Nurs 2016;25:16-23. [Crossref] [PubMed]
- Han Y, Yuan J, Luo Z, et al. Determinants of hopelessness and depression among Chinese hospitalized esophageal cancer patients and their family caregivers. Psychooncology 2013;22:2529-36. [Crossref] [PubMed]
- Podsakoff PM, MacKenzie SB, Lee JY, et al. Common method biases in behavioral research: a critical review of the literature and recommended remedies. J Appl Psychol 2003;88:879-903. [Crossref] [PubMed]
- Akdoğan R, Çimşir E. Linking inferiority feelings to subjective happiness: Self-concealment and loneliness as serial mediators. Pers Individ Dif 2019;149:14-20. [Crossref]
- Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behav Res Ther 2017;98:39-57. [Crossref] [PubMed]
- Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput 2004;36:717-31. [Crossref] [PubMed]
- Hayes AF, Preacher KJ. Quantifying and Testing Indirect Effects in Simple Mediation Models When the Constituent Paths Are Nonlinear. Multivariate Behav Res 2010;45:627-60. [Crossref] [PubMed]
- Lassmann I, Dinkel A, Marten-Mittag B, et al. Benefit finding in long-term prostate cancer survivors. Support Care Cancer 2021;29:4451-60. [Crossref] [PubMed]
- Wepf H, Joseph S, Leu A. Pathways to Mental Well-Being in Young Carers: The Role of Benefit Finding, Coping, Helplessness, and Caring Tasks. J Youth Adolesc 2021;50:1911-24. [Crossref] [PubMed]
- Pascoe L, Edvardsson D. Benefit finding in cancer: a review of influencing factors and health outcomes. Eur J Oncol Nurs 2013;17:760-6. [Crossref] [PubMed]
- Parveen S, Morrison V. Predicting caregiver gains: a longitudinal study. Br J Health Psychol 2012;17:711-23. [Crossref] [PubMed]
- Dempster M, McCorry NK, Brennan E, et al. Illness perceptions among carer-survivor dyads are related to psychological distress among Oesophageal cancer survivors. J Psychosom Res 2011;70:432-9. [Crossref] [PubMed]
- Applebaum AJ, Buda KL, Schofield E, et al. Exploring the cancer caregiver's journey through web-based Meaning-Centered Psychotherapy. Psychooncology 2018;27:847-56. [Crossref] [PubMed]
- McGregor BA, Antoni MH, Boyers A, et al. Cognitive-behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. J Psychosom Res 2004;56:1-8. [Crossref] [PubMed]
- Gallagher S, O'Sullivan L, Hughes Z, et al. Building Resources in Caregivers: Feasibility of a Brief Writing Intervention to Increase Benefit Finding in Caregivers. Appl Psychol Health Well Being 2020;12:513-31. [Crossref] [PubMed]
- Zhang MM, Chen JJ, Zhang T, et al. Feasibility and effect of a guided self-disclosure intervention designed to facilitate benefit finding in breast cancer patients: A pilot study. Eur J Oncol Nurs 2021;50:101879. [Crossref] [PubMed]
- Chambers SK, Girgis A, Occhipinti S, et al. Psychological distress and unmet supportive care needs in cancer patients and carers who contact cancer helplines. Eur J Cancer Care (Engl) 2012;21:213-23. [Crossref] [PubMed]
- Mok E, Chan F, Chan V, et al. Family experience caring for terminally ill patients with cancer in Hong Kong. Cancer Nurs 2003;26:267-75. [Crossref] [PubMed]
- Graham L, Dempster M, McCorry NK, et al. Change in psychological distress in longer-term oesophageal cancer carers: are clusters of illness perception change a useful determinant? Psychooncology 2016;25:663-9. [Crossref] [PubMed]
- Kayser K, Acquati C, Reese JB, et al. A systematic review of dyadic studies examining relationship quality in couples facing colorectal cancer together. Psychooncology 2018;27:13-21. [Crossref] [PubMed]
- Lin Y, Luo X, Li J, et al. The dyadic relationship of benefit finding and its impact on quality of life in colorectal cancer survivor and spousal caregiver couples. Support Care Cancer 2021;29:1477-86. [Crossref] [PubMed]
- Schulz R. The Future of Caregiver Efficacy Research: Commentary on "Long-Term Outcomes of the Benefit-Finding Group Intervention for Alzheimer Family Caregivers". Am J Geriatr Psychiatry 2019;27:995-7. [Crossref] [PubMed]
- Mavandadi S, Dobkin R, Mamikonyan E, et al. Benefit finding and relationship quality in Parkinson's disease: a pilot dyadic analysis of husbands and wives. J Fam Psychol 2014;28:728-34. [Crossref] [PubMed]


