
Stenting versus surgery in obstructed malignant colorectal cancer—a review of short and long-term results
Introduction
Colorectal cancer (CRC) is one of the commonest cancers in the world. Emergency presentations of CRC include perforation, obstruction and bleeding. Options for perforated CRC are rather limited. In the presence of peritonitis, laparotomy with washout and resection of the primary is often required to control the sepsis (1) Extraperitoneal/retroperitoneal perforation will invariably require sepsis control, eventual resection of the cancer or proximal diversion of faecal stream. Oncological outcomes of perforated CRCs are dismal. Patients presenting with massive lower gastrointestinal haemorrhage from CRC is uncommon. Resuscitation with blood products is key in the initial stages. At the same time, control of the bleeding source is imperative. If surgical resection is not preferred in the acute setting, mesenteric embolization is an alternative option to control the massive haemorrhage prior to definitive surgery (2).
In patients presenting with intestinal obstruction, several options are available to deal with the crisis depending on the site of obstruction, presence of metastatic disease as well as patients’ pre-morbid conditions (3). The advent of self-expanding metallic stents (SEMS) has also opened a whole new paradigm in the management of intestinal obstruction. In this article, we seek to review the various options and focusing in particular the role of SEMS in obstructed CRC.
Before we delve further into the role of SEMS, surgery is obstructed CRC stills play an important role. In patients with right sided colonic obstruction (proximal to splenic flexure), the role of SEMS is less evaluated. This is probably contributed by the relatively lower morbidity in surgery for right sided CRC versus left sided ones (4). Stoma were also more frequently created in surgery for left sided colonic obstruction. However, emergency right hemicolectomy for right sided colonic obstruction is not without risks (5). A mortality rate of 10% with an acceptable leak rate of 4% has been reported. Stomas following right hemicolectomy have also been created, and notably in sicker patients.
Stenting for right sided colonic obstructions has been reported in smaller series than for left sided pathologies (6,7). Intuitively, stenting for right sided obstructions would be slightly tougher as there is the need to traverse a longer segment of colon before reaching the pathology. In addition, with the relatively good outcomes for emergency right hemicolectomy procedure, including the adoption of laparoscopic procedures in certain instances, preference for stenting over surgery in right sided colonic obstructions is not clear (8,9).
For patients with left sided colonic obstructions, numerous surgical options have been described. These could range from simply a proximal defunctioning stoma, resection of the primary with or without primary anastomosis and with or without a protecting stoma. However, any emergency resection procedures are associated with far higher rates of morbidity compared with similar surgery under an elective setting. Mortality rates in patients who undergo emergency surgery (ES) for an obstructing lesion may be as high as 30%, compared with <5% in patients who undergo elective surgery (10,11).
The placement of a SEMS has been proposed as a “bridge-to-surgery” in patients who present with obstructing left sided colon cancers. First described in 1994 by Tejero et al. (12), the purported benefits of stenting include converting an ES into an elective one, therefore allowing for more complete staging and optimization of the patient’s pre-morbid conditions (13,14), as well as reduction in stoma creation rates and increased usage of a laparoscopic approach. This is however balanced against the concern of increased perforation which may result in dissemination of disease and worse outcomes.
A number of randomized controlled trials have sought to evaluate both short term outcomes, as well as long term outcomes comparing SEMS with upfront ES in non-metastatic obstructing left sided CRC. This review will analyze the results from these RCTs and evaluate the evidence for SEMS versus ES with reference to these short-term and long-term outcomes.
Results
Overview of RCTs reviewed
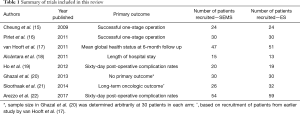
Till date, eight RCTs have been published comparing SEMS with ES in obstructing left sided CRC (15-22). A summary of these trials can be found in Table 1. In all of these trials, short-term data relating to the safety of SEMS is reported, with all but two trials using short-term outcomes as the primary outcome for the study (15-19,22). Only three trials have attempted to address the concern of long-term recurrence (20-22), however none of these measured oncologic outcomes as their primary outcome. Notably, Sloothaak et al. (21) utilized a subgroup of patients originally recruited for the Dutch Stent-In 2 trial (17) for their oncologic analysis.
Full table
Numbers in each arm of the trials published were generally small, with none achieving more than a hundred patients in either arm. Importantly, two trials were stopped prematurely, albeit for different reasons.
Short-term outcomes
Almost all trials performed to evaluate SEMS versus ES evaluated the short-term outcomes of SEMS. Taking a composite average of all trials performed, the overall technical success was 81.1% and the clinical success was 76.1% (23). The much-feared complication of colonic perforation during the deployment of SEMS only occurred in 5.0% of patients. This statistic however may under report the overall perforation rates, as not all studies reported “silent perforations”, which are detected only on pathological examination. In addition, 76.1% of patients proceeded to elective surgery, and the success of performing elective laparoscopic surgery was 41.0% (23).
Proponents of SEMS discuss its advantages being a reduction in the permanent stoma rate, as well as being able to use the intervening time from stenting to surgery to optimize the patient’s comorbidities, thereby resulting in reduced mortality rates. Comparing SEMS to ES, the combined permanent stoma rate was statistically significantly lower (8.7% vs. 20.0%, P=0.0027, 95% CI, 3.96–18.6%). There was however no difference in mortality rates (4.0% vs. 4.6%, P=0.783, 95% CI, –4.02–5.3%).
In spite of this, two studies were stopped prematurely, albeit for polar reasons. The Dutch Stent-In 2 trial by van Hooft et al. (17) was stopped prematurely due to increased 30-day morbidity amongst patients who underwent SEMS. The study by Alcántara et al. (18) was also stopped prematurely due to increased complications amongst the ES group. Out of 13 patients, four patients suffered from an anastomotic leak and patients who underwent ES suffered from an overall morbidity of 53.8%.
Together, these findings suggest that there are short-term advantages in patients who undergo SEMS. In particular, there is an increased usage of laparoscopic surgery in patients who successfully undergo stenting as well as a significant reduction in permanent stoma rates.
Long-term outcomes
Compared with short-term outcomes, only three trials published encountered for long-term oncologic outcomes in patients who underwent SEMS. The first trial to publish long-term oncologic outcomes was by Alcántara et al. In this study which had a mean follow-up period of 37.6 months, there was no statistically significant reduction in overall survival between patients who underwent SEMS and ES (P=0.876) although it must be noted that this study was stopped early, and as such, recruited few patients in each group.
The next trial to report on oncologic outcomes was the Stent-In 2 trial (21). After the trial was stopped prematurely due to increased complications amongst patients who had undergone ES, patients with benign, as well as incurable disease were excluded. The authors then analysed the outcomes of patients remaining, and showed that while there was no difference in outcomes between patients who had SEMS and ES in terms of disease-free survival (P=0.149), disease-specific survival (P=0.061) and overall survival (P=0.468), there was however a statistically significant difference if patients who had undergone SEMS were divided into patients that suffered from a perforation and those who did not. The authors noted that 4-year disease free survival in the six patients who had suffered a perforation was zero. This was statistically significant compared to patients who did not suffer from a perforation. Although not statistically significant, patients who suffered from a stent perforation performed worse than patients who did not suffer from a stent perforation and from those who underwent ES. Unsurprisingly, the authors concluded that stent perforations were associated with an increased risk of recurrence, though conceded that the numbers were small.
The ESCO trial by Arezzo et al. was the most contemporary trial evaluating SEMS versus ES (22). Although it was powered to detect a difference in the 60-day morbidity of patients, the authors have followed up patients recruited into the study and report oncological results with a median follow up of 36 months (range, 16–58 months). The authors noted that there was no difference in overall survival (P=0.998) as well as progression-free survival (P=0.893) in both groups. Unlike the Stent-In 2 trial, this trial did not report outcomes specific to patients who had suffered from a perforation.
Metastatic CRC
In contrast to patients without metastatic disease, there if good evidence that SEMS should be utilized in patients who are known to have metastatic disease. Stenting is an alternative to stoma creation in such patients (24), and based on guidelines by the European Society of Gastrointestinal Endoscopy (ESGE), SEMS is the preferred treatment for patients with malignant obstructed who are managed with a palliative intent (25). Compared to patients who undergo stoma creation, patients who undergo stenting experience shorter length of stay within hospital (5 vs. 12 days, P=0.003), earlier commencing of chemotherapy (4 vs. 7 weeks, P=0.02), as well as reduced stoma creation rates (OR 0.19; 95% CI, 0.12–0.28), P<0.01) (26-28).
Conclusions
Numerous trials have been performed evaluating SEMS and ES but most have been small in number. The main concern regarding the use of SEMS has been concerns relating to the increased risk of tumor dissemination occurring in cases of perforation. In particular, there are concerns regarding the safety of stenting in patients who have a silent perforation during pathologic examination. Further trials will need to be performed as our understanding of the implications of SEMS for the oncologic safety of the patient remain unanswered. While SEMS can certainly be performed safely, and portends obvious short-term benefits to the patients, there is insufficient evidence to conclude that SEMS does not result in worse disease-free and overall survival.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Nan Zun Teo, James Chi-Yong Ngu) for the series “Current Strategies in Colon Cancer Management” published in Journal of Gastrointestinal Oncology. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jgo.2020.01.08). The series “Current Strategies in Colon Cancer Management” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Tan KK, Hong CC, Zhang J, et al. Surgery for perforated colorectal malignancy in an Asian population: an institution's experience over 5 years. Int J Colorectal Dis 2010;25:989-95. [Crossref] [PubMed]
- Tan KK, Wong D, Sim R. Superselective embolization for lower gastrointestinal hemorrhage: an institutional review over 7 years. World J Surg 2008;32:2707-15. [Crossref] [PubMed]
- Søreide K. Emergency management of acute obstructed left-sided colon cancer: loops, stents or tubes? Endoscopy 2013;45:247-8. [Crossref] [PubMed]
- Tan KK, Sim R. Surgery for obstructed colorectal malignancy in an Asian population: predictors of morbidity and comparison between left- and right-sided cancers. J Gastrointest Surg 2010;14:295-302. [Crossref] [PubMed]
- Tan KK, Liu JZ, Yeow Y, et al. Is emergency right hemicolectomy still associated with significant morbidity and mortality rates? An institution's experience of 207 cases over 6 years. Int J Colorectal Dis 2011;26:1157-61. [Crossref] [PubMed]
- Morita S, Yamamoto K, Ogawa A, et al. Benefits of using a self-expandable metallic stent as a bridge to surgery for right- and left-sided obstructive colorectal cancers. Surg Today 2019;49:32-7. [Crossref] [PubMed]
- Ji WB, Kwak JM, Kang DW, et al. Clinical benefits and oncologic equivalence of self-expandable metallic stent insertion for right-sided malignant colonic obstruction. Surg Endosc 2017;31:153-8. [Crossref] [PubMed]
- Cirocchi R, Cesare Campanile F, Di Saverio S, et al. Laparoscopic versus open colectomy for obstructing right colon cancer: A systematic review and meta-analysis. J Visc Surg 2017;154:387-99. [Crossref] [PubMed]
- Ng SS, Lee JF, Yiu RY, et al. Emergency laparoscopic-assisted versus open right hemicolectomy for obstructing right-sided colonic carcinoma: a comparative study of short-term clinical outcomes. World J Surg 2008;32:454-8. [Crossref] [PubMed]
- Smith JJ, Cornish J, Tekkis P, et al. The National Bowel Cancer Audit Project 2007: quality improvement and open reporting. 2007 Association of Coloproctology of Great Britain and Ireland, London.
- Hennekinne-Mucci S, Tuech JJ, Bréhant O, et al. Emergency subtotal/total colectomy in the management of obstructed left colon carcinoma. Int J Colorectal Dis 2006;21:538-41. [Crossref] [PubMed]
- Tejero E, Mainar A, Fernández L, et al. New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum 1994;37:1158-9. [Crossref] [PubMed]
- Baron TH, Dean PA, Yates MR 3rd, et al. Expandable metal stents for the treatment of colonic obstruction: techniques and outcomes. Gastrointest Endosc 1998;47:277-86. [Crossref] [PubMed]
- Mainar A, De Gregorio Ariza MA, Tejero E, et al. Acute colorectal obstruction: treatment with self-expandable metallic stents before scheduled surgery--results of a multicenter study. Radiology 1999;210:65-9. [Crossref] [PubMed]
- Cheung HY, Chung CC, Tsang WW, et al. Endolaparoscopic approach vs conventional open surgery in the treatment of obstructing left-sided colon cancer: a randomized controlled trial. Arch Surg 2009;144:1127-32. [Crossref] [PubMed]
- Pirlet IA, Slim K, Kwiatkowski F, et al. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc 2011;25:1814-21. [Crossref] [PubMed]
- van Hooft JE, Bemelman WA, Oldenburg B, et al. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol 2011;12:344-52. [Crossref] [PubMed]
- Alcántara M, Serra-Aracil X, Falcó J, et al. Prospective, controlled, randomized study of intraoperative colonic lavage versus stent placement in obstructive left-sided colonic cancer. World J Surg 2011;35:1904-10. [Crossref] [PubMed]
- Ho KS, Quah HM, Lim JF, et al. Endoscopic stenting and elective surgery versus emergency surgery for left-sided malignant colonic obstruction: a prospective randomized trial. Int J Colorectal Dis 2012;27:355-62. [Crossref] [PubMed]
- Ghazal AH, El-Shazly WG, Bessa SS, et al. Colonic endolumenal stenting devices and elective surgery versus emergency subtotal/total colectomy in the management of malignant obstructed left colon carcinoma. J Gastrointest Surg 2013;17:1123-9. [Crossref] [PubMed]
- Sloothaak DA, van den Berg MW, Dijkgraaf MG, et al. Oncological outcome of malignant colonic obstruction in the Dutch Stent-In 2 trial. Br J Surg 2014;101:1751-7. [Crossref] [PubMed]
- Arezzo A, Balague C, Targarona E, et al. Colonic stenting as a bridge to surgery versus emergency surgery for malignant colonic obstruction: results of a multicentre randomised controlled trial (ESCO trial). Surg Endosc 2017;31:3297-305. [Crossref] [PubMed]
- Boland PA, Kelly ME, Donlon NE, et al. Outcomes following colonic stenting for malignant left-sided bowel obstruction: a systematic review of randomised controlled trials. Int J Colorectal Dis 2019;34:1625-32. [Crossref] [PubMed]
- Zahid A, Young CJ. How to decide on stent insertion or surgery in colorectal obstruction? World J Gastrointest Surg 2016;8:84-9. [Crossref] [PubMed]
- van Hooft JE, van Halsema EE, Vanbiervliet G, et al. Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Endoscopy 2014;46:990-1053. [Crossref] [PubMed]
- Zhao XD, Cai BB, Cao RS, et al. Palliative treatment for incurable malignant colorectal obstructions: a meta-analysis. World J Gastroenterol 2013;19:5565-74. [Crossref] [PubMed]
- Takahashi H, Okabayashi K, Tsuruta M, et al. Self-Expanding Metallic Stents Versus Surgical Intervention as Palliative Therapy for Obstructive Colorectal Cancer: A Meta-analysis. World J Surg 2015;39:2037-44. [Crossref] [PubMed]
- Lim TZ, Tan KK. Endoscopic stenting in colorectal cancer. J Gastrointest Oncol 2019. [Crossref] [PubMed]


