Stomach-partitioning gastrojejunostomy is better than conventional gastrojejunostomy in palliative care of gastric outlet obstruction for gastric or pancreatic cancer: a meta-analysis
Introduction
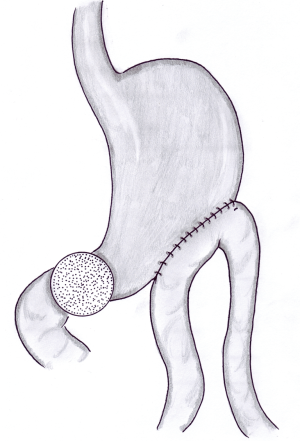
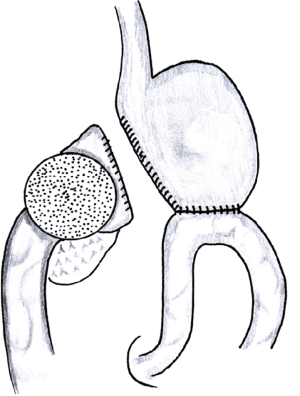
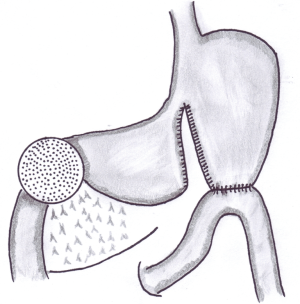
Unresectable distal gastric or pancreatic malignancies are the most common cause of gastric outlet obstruction (GOO). Fourteen-point-nine percent of patients with antral gastric cancer develop signs and symptoms of GOO (1) and 10–25% of patients with pancreatic cancer require intervention for GOO (2-4). The traditional surgical procedure for GOO is a side-to-side gastrojejunal anastomosis approximately 20 to 30 cm distal to the ligament of Treitz (5) (Figure 1). Even though nowadays the palliative care of GOO can also be performed endoscopically by positioning a self-expanding stent (2,6), the gastrojejunal bypass still retains its role in the following situations: (I) surgeons working in hospitals without an advanced interventional endoscopy service; (II) diagnosis of unresectability made during the surgical intervention, considering that up to 10% of patients are still found to have unresectable disease at the time of surgery (2,7). The limit of the conventional gastrojejunostomy (CGJ) is the high postoperative incidence of delayed gastric emptying (DGE) so that 30–50% of these patients continue to have preoperative symptoms: nausea, vomiting, difficulty eating (8-10). Some surgeons added the gastric partitioning to the gastrojejunostomy (GPGJ) to prevent the DGE by ensuring a complete passage of food into the jejunum (11-13). Gastric partitioning was originally described by Devine in 1925 as a method of antral exclusion and complete division of the stomach accompanied by a gastro-entero anastomosis in the proximal gastric pouch (Figure 2) for the management of difficult duodenal ulcers (14). Subsequently, in 1936 Maingot adapted the procedure for the treatment of unresectable antral cancers (15). The risks of Devine’s classic technique are antral stump leak, hemorrhage and rupture. A further limit of this technique is the inability to perform an endoscopic cancer surveillance (8). For the above-mentioned reasons, a modified Devine technique was introduced, which divides partially the stomach, maintaining a passage that is 2 to 3 cm in diameter in the lesser curvature, and connects the jejunum to the proximal part of the stomach (8,16) (Figure 3). Although several authors reported better outcomes in patients submitted to GPGJ compared to CGJ (9,10,17), clinical experience with GPGJ is poor, studies comparing the two techniques are few and no randomized trials were performed.
The aim of the present study is to evaluate the literature comparing GPGJ (partial or complete) with CGJ in patients operated for GOO for gastric or pancreatic cancer to assess if DGE, return to nutrition by oral intake, length of hospital stay and survival are better in GPGJ group compared to CGJ group.
Methods
Data sources and search strategy
A computerized literature search was performed until January 2017 on Medline using the following medical subject headings: “gastrojejunostomy”, “conventional gastrojejunostomy”, “stomach-partitioning”, “partial stomach-partitioning”, “Devine procedure”, “gastric outlet obstruction” and “palliative duodenal bypass”. Only papers published in English were considered while no publication date restrictions were applied. Additional studies were identified by manual search of references of original studies to identify further relevant works not found by the computer search.
Eligibility criteria
Studies meeting inclusion criteria were those comparing GPGJ (partial or complete) with CGJ in patients with GOO for gastric or pancreatic cancer. Both surgical procedures could be performed via open or laparoscopic approaches. Furthermore, the postoperative follow-up had to report at least one of the following primary outcomes: (I) DGE; (II) nutrition by oral intake; (III) length of hospital stay and (IV) survival time.
DGE is a postoperative complication defined by the temporary inability to return to a standard diet after surgery. The definition of DGE may differ according to the researchers. Nobody adopted the definition proposed by the International Study Group of Pancreatic Surgery (ISGPS) (18). Oida et al. (9) used the definition proposed by Yeo and colleagues (19) while Usuba et al. (10) and Yamagishi et al. (20) did not specify the DGE definition used.
Nutrition by oral intake was defined as the postoperative oral intake of regular meals. The length of hospital stay and survival time were expressed in days.
Data extraction
Study selection and data extraction were conducted independently by two investigators (D Lorusso, A Giliberti). Any disagreements or differences in the data extraction between the two authors were resolved through consensus after rechecking the source data and consultations with additional investigators (M Bianco, G Lantone, G Leandro).
Statistical analysis
For dichotomous outcomes formal statistical tests for heterogeneity of the odds ratios (ORs) were performed with the Cochrane Q test, heterogeneity being assumed with a P value ≤0.05. The Q test for heterogeneity was performed to determine whether to use a random-effect model or a fixed-effect model. When a Q test indicated statistical heterogeneity, a random-effect model weighted by the DerSimonian-Laird method must be used. On the other hand, a fixed-effect model weighted by the Mantel-Haenszel method has to be used for pooling the ORs. Results were expressed as OR and 95% confidence interval (95% CI). All procedures and calculations used in the meta-analysis were made following the methodology reported elsewhere (21).
For the continuous outcomes, many authors reported the median value instead of the mean ± SD or reported only the mean value. Given the unavoidable lack or incompleteness of data, the meta-analytical methodology was not applicable. Anyway, we decided to calculate the mean of the measures of central tendency (median and mean) in order to perform a descriptive comparison of the two surgical techniques.
All statistical analyses were performed under Leandro’s supervision, as co-author and medical statistician.
Results
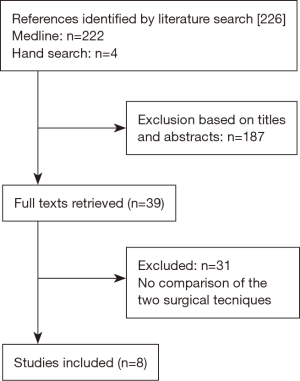
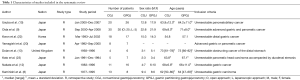
A total of 226 potentially eligible studies were identified, as reported in Figure 4. After reading titles and abstracts, 39 possibly relevant studies were retrieved as full text articles. Based on the full text assessment, 31 studies were excluded because no one compared the two surgical techniques. Eight studies met our eligibility criteria and were included in the systematic review, yielding a total of 226 patients with GOO for gastric or pancreatic cancer. One hundred and seventeen (51.8%) patients underwent GPGJ (partial or complete) while 109 (48.2%) patients were submitted to CGJ. The characteristics of the included studies are summarized in Table 1. The eight included studies followed a retrospective design and had an inherent low methodological quality. Overall, the time period covered was almost 40 years [1977–2008]. Both groups were comparable for age and sex distribution in all the considered studies.
Full table
DGE
The overall DGE rate was 11.6% (8/69) in the GPGJ group and 43.6% (27/62) in the CGJ group, respectively (Figure 5). Data were pooled from four studies and showed a risk significantly reduced by 5-fold in the GPGJ group (OR =4.997, 95% CI: 2.310–10.810). Heterogeneity among the studies was no significant (Q value =2.820; P=0.420), allowing us to use a fixed effect model.

Nutrition by oral intake
The rate of patients able to take regular meals after the surgery was 89.6% (43/48) in the GPGJ group and 56.5% (26/46) in the CGJ group, respectively (Figure 6). Data were pooled from 4 studies that did not show significant heterogeneity (Q value =1.790; P=0.617). By using a fixed-effect model, pooled analysis demonstrated a statistically significant advantage in the GPGJ group compared to CGJ (OR =0.156, 95% CI: 0.055–0.442).

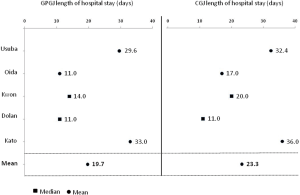
Length of hospital stay
Although the length of hospital stay (days) was reported by five authors, only Usuba et al. (10) and Oida et al. (9) reported completed values as mean ± SD. Two authors used the median value (13,22) while one author (23) mentioned only the mean value. The measure of central tendency for the length of hospital stay was 23.3 days for CGJ and 19.7 days for GPGJ. Although statistical inference was not applicable, CGJ patients seem to be submitted to longer hospital stay (Figure 7).
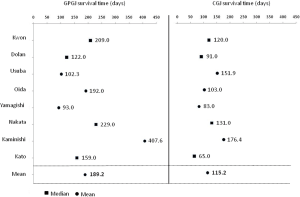
Survival time
The survival time (days) was reported as mean ± SD by Usuba et al. (10) and Oida et al. (9). Four studies used the median value (12,13,22,23) while two studies (8,20) used only the mean value. The measure of central tendency for the survival was 115.2 days for CGJ and 189.2 days for GPGJ. Although statistical inference was not applicable, the survival trend is clearly in favor of the GPGJ group (Figure 8).
Discussion
The World Health Organization (WHO) asserts that the goal of palliative care is achievement of the best quality of life for patients and their families (5). GOO treatment in patients with unresectable gastric or pancreatic cancer plays a key role because vomiting and inability to eat can significantly impair quality of life and accelerate death in these patients. Subsequently, surgeons have the challenge of choosing the best surgical technique to achieve WHO goal.
Recently, the endoscopic placement of self-expanding metal stents (SEMS) has been proposed. Complications related to SEMS are reported in about a quarter of patients and include late complications as migration and obstruction of the stent (2). Furthermore, a randomized controlled trial comparing CGJ with stent placement in patients with malignant GOO found that patients submitted to SEMS placement had a faster return to oral intake (5 vs. 8 days) but surgery had a significantly better oral intake with more total days tolerating oral intake. For this reason, the authors recommended to perform CGJ in patients with a life expectancy of 2 months or longer (24).
Therefore, gastrojejunostomy still retains its role in the palliative treatment of GOO, even because sometimes patients are found to have an unresectable gastric or pancreatic tumor at laparotomy and because the palliative treatment of these cancers could be performed in hospitals that do not have advanced endoscopy.
The traditional gastrojejunostomy shown in Figure 1 is certainly the most widely surgical technique used worldwide. However, DGE characterized by nausea, vomiting and lack of oral intake persists after surgery in 30–50% of patients (9,10). To prevent such a complication, several authors performed a technical variant of the CGJ based on the partial or complete stomach-partitioning (8-13,16,17). Although better outcomes were reported with the stomach-partitioning technique, GPGJ is still a little-used surgery due to the small number of studies and the lack of prospective clinical studies.
Our meta-analysis compared for the first time GPGJ to CGJ and showed that GPGJ is better for all the outcomes considered: rate of DGE (11.6% after GPGJ and 43.6% after CGJ, OR =4.997) and rate of regular oral intake (89.6% after GPGJ and 56.5% after CGJ, OR =0.156); furthermore, the measure of central tendency for the survival was 189.2 days for GPGJ and 115.2 days for CGJ.
The most extensive experience on GPGJ was reported by Arrangoiz et al. (16) which included 55 patients with locally advanced or metastatic tumours submitted to GPGJ. In agreement with our meta-analysis, no patient developed signs of GOO after surgery and at last follow-up 95% were tolerating their enteral diet with a median overall survival time of 9 months. However, as their study did not compare the two techniques, it was not included in the meta-analysis.
A recent retrospective study (17) compared ten patients submitted to GPGJ with 14 patients submitted to CGJ for GOO. However, it was not included in our meta-analysis because patients were operated not only for gastric or pancreatic cancer but also for colon cancer, jejunal cancer, rectal cancer with carcinosis and benign diseases. The incidence of DGE grade B-C was significantly lower in the GPGJ group (0%) compared with the CGJ group (42.9%, P=0.024) and at follow-up oral nutrition was possible in the 100% of GPGJ patients (9/9) versus the 30.8% of CGJ patients (4/13) (P=0.002). These results are in agreement with our meta-analysis.
The higher DGE frequency after CGJ, associated with vomiting persistence and no regular food intake, is generally attributed to the persistence of gastric movement towards the distal part of the stomach with ingested food retained in the antrum (8) while with the GPGJ technique the distal stomach is completely excluded from food’s transit (Figures 2,3).
The results of our study showed a survival improvement in the GPGJ patients. Despite the lack of homogeneity of the reported survival data, the mean length of survival was 74 days longer in patients submitted to this technique compared to the CGJ group.
Modern chemotherapy has improved the median survival time in both gastric (25) and pancreatic cancer (26). The nutritional state and the general conditions are interdependent factors which influence chemotherapy tolerance. Although studies included in our meta-analysis do not mention chemotherapy, the highest survival after GPGJ compared to CGJ (189.2 versus 115.2 days) could be explained with better nutritional conditions due to proper nutrition which is a necessary condition to tolerate chemotherapy. Therefore, our meta-analysis highlighted that GPGJ is more useful than CGJ in order to eliminate main symptoms associated with GOO and to improve patient’s quality of life, as recommended by WHO.
Over recent years, laparoscopic GPGJ has been demonstrated as a good alternative to open technique with comparable outcomes (27,28). Only one study (9) included in our meta-analysis also comprehended five patients submitted to laparoscopic surgery. However, the small number of reported cases did not allow us to perform a subgroup analysis to compare the two surgical techniques.
Some of the results of our meta-analysis should be interpreted with caution for some biases: presence in the literature of only retrospective studies, wide variability of these studies, wide span of time in which the data were collected [1977–2008] and, above all, the patients’ selection bias which could have influenced the results. Finally, the use of the mean of the measures of central tendency (median and mean) to compare the two surgical techniques is unconventional but was necessary to by-pass the heterogeneity and the lack of completeness of continuous data.
Even though many of the studies included in our meta-analysis conclude that GPGJ is useful and ensures better functional results than CGJ, due to the small number of patients, it will be required to assess GPGJ efficacy in a larger number of patients and/or in randomized controlled trials. Moreover, a multicenter design for randomized controlled trials should be required to achieve a large number of included patients.
Despite the above-mentioned limits, our meta-analysis provides a further contribution to the definition of the best technique for the palliative care of GOO for advanced gastric or pancreatic cancer and confirms that GPGJ is associated with lower rates of DGE and higher rates of normal oral intake compared to CGJ with a tendency towards better survival in the GPGJ group. Pending further evidence, we believe that GPGJ should be considered the treatment of choice of GOO in patients with unresectable gastric or pancreatic cancer.
Acknowledgements
We would like to acknowledge Dr. Angelo Santorelli for drawing the illustrations of the different surgical procedures.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Watanabe A, Maehara Y, Okuyama T, et al. Gastric carcinoma with pyloric stenosis. Surgery 1998;123:330-4. [Crossref] [PubMed]
- Stark A, Hines OJ. Endoscopic and operative palliation strategies for pancreatic ductal adenocarcinoma. Semin Oncol 2015;42:163-76. [Crossref] [PubMed]
- Nakakura EK, Warren RS. Palliative care for patients with advanced pancreatic and biliary cancers. Surg Oncol 2007;16:293-7. [Crossref] [PubMed]
- Schmidt C, Gerdes H, Hawkins W, et al. A prospective observational study examining quality of life in patients with malignant gastric outlet obstruction. Am J Surg 2009;198:92-9. [Crossref] [PubMed]
- Perone JA, Riall TS, Olino K. Palliative Care for Pancreatic and Periampullary Cancer. Surg Clin North Am 2016;96:1415-30. [Crossref] [PubMed]
- Maire F, Sauvanet A. Palliation of biliary and duodenal obstruction in patients with unresectable pancreatic cancer: endoscopy or surgery? J Visc Surg 2013;150:S27-31. [Crossref] [PubMed]
- Kneuertz PJ, Cunningham SC, Cameron JL, et al. Palliative surgical management of patients with unresectable pancreatic adenocarcinoma: trends and lessons learned from a large, single institution experience. J Gastrointest Surg 2011;15:1917-27. [Crossref] [PubMed]
- Kaminishi M, Yamaguchi H, Shimizu N, et al. Stomach-partitioning gastrojejunostomy for unresectable gastric carcinoma. Arch Surg 1997;132:184-7. [Crossref] [PubMed]
- Oida T, Mimatsu K, Kawasaki A, et al. Modified Devine exclusion with vertical stomach reconstruction for gastric outlet obstruction: a novel technique. J Gastrointest Surg 2009;13:1226-32. [Crossref] [PubMed]
- Usuba T, Misawa T, Toyama Y, et al. Is modified Devine exclusion necessary for gastrojejunostomy in patients with unresectable pancreatobiliary cancer? Surg Today 2011;41:97-100. [Crossref] [PubMed]
- Kwok SP, Chung SC, Griffin SM, et al. Devine exclusion for unresectable carcinoma of the stomach. Br J Surg 1991;78:684-5. [Crossref] [PubMed]
- Nakata Y, Kimura K, Tomioka N, et al. Gastric exclusion for unresectable gastric cancer. Hepatogastroenterology 1999;46:2654-7. [PubMed]
- Dolan K, Sue-Ling H. Proximal gastric exclusion for unresectable gastric cancer. ANZ J Surg 2003;73:929-31. [Crossref] [PubMed]
- Devine HB. Basic principles and supreme difficulties in gastric surgery. Surg Gynecol Obstet 1925;40:1-16.
- Maingot R. The surgical treatment of irremovable cancer of the pyloric segment of the stomach. Ann Surg 1936;104:161-6. [Crossref] [PubMed]
- Arrangoiz R, Papavasiliou P, Singla S, et al. Partial stomach-partitioning gastrojejunostomy and the success of this procedure in terms of palliation. Am J Surg 2013;206:333-9. [Crossref] [PubMed]
- Ernberg A, Kumagai K, Analatos A, et al. The Added Value of Partial Stomach-partitioning to a Conventional Gastrojejunostomy in the Treatment of Gastric Outlet Obstruction. J Gastrointest Surg 2015;19:1029-35. [Crossref] [PubMed]
- Wente MN, Bassi C, Dervenis C, et al. Delayed gastric emptying (DGE) after pancreatic surgery: a suggested definition by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 2007;142:761-8. [Crossref] [PubMed]
- Yeo CJ, Barry MK, Sauter PK, et al. Erythromycin accelerates gastric emptying after pancreaticoduodenectomy. A prospective, randomized, placebo-controlled trial. Ann Surg 1993;218:229-37. [Crossref] [PubMed]
- Yamagishi F, Arai H, Yoshida T, et al. Partial separating gastrojejunostomy for incurable cancer of the stomach or pancreas. Hepatogastroenterology 2004;51:1623-5. [PubMed]
- Leandro G. Meta-analysis in Medical Research. Oxford, UK: Blackwell Publishing, 2004.
- Kwon SJ, Lee HG. Gastric partitioning gastrojejunostomy in unresectable distal gastric cancer patients. World J Surg 2004;28:365-8. [Crossref] [PubMed]
- Kato K, Morita T, Miyasaka Y, et al. Modified Devine exclusion for unresectable pancreatic head carcinoma. Hepatogastroenterology 2001;48:569-71. [PubMed]
- Jeurnink SM, Steyerberg EW, van Hooft JE, et al. Surgical gastrojejunostomy or endoscopic stent placement for the palliation of malignant gastric outlet obstruction (SUSTENT study): a multicenter randomized trial. Gastrointest Endosc 2010;71:490-9. [Crossref] [PubMed]
- Ohashi M, Kanda T, Hirota M, et al. Gastrojejunostomy as induction treatment for S-1-based chemotherapy in patients with incurable gastric cancer. Surg Today 2008;38:1102-7. [Crossref] [PubMed]
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817-25. [Crossref] [PubMed]
- Suzuki O, Shichinohe T, Yano T, et al. Laparoscopic modified Devine exclusion gastrojejunostomy as a palliative surgery to relieve malignant pyloroduodenal obstruction by unresectable cancer. Am J Surg 2007;194:416-8. [Crossref] [PubMed]
- Hirahara N, Matsubara T, Hyakudomi R, et al. Laparoscopic stomach-partitioning gastrojejunostomy with reduced-port techniques for unresectable distal gastric cancer. J Laparoendosc Adv Surg Tech A 2014;24:177-82. [Crossref] [PubMed]