
Short course radiation therapy for rectal cancer in the elderly: can radical surgery be avoided?
Introduction
Rectal cancer is a disease of the elderly, with the median age at diagnosis 69 years in men and 73 years in women per the American Cancer Society 2010–2014 data. The standard treatment for stage II and III disease in the United States typically consists of neoadjuvant long course chemoradiation therapy followed by surgical resection (1). An alternative is short course radiation therapy (SCRT), which has shown to be comparable in effectiveness (2). In elderly patients with multiple comorbidities, the potential toxicities of chemoradiation therapy followed by surgery can be prohibitive. Further, population based data has shown higher peri-operative complications specifically following definitive surgery specifically for rectal cancer in patients >70 years of age (3). In our institution, SCRT has been used, sometimes alone, to treat elderly patients who were not suitable candidates for chemoradiation neoadjuvant therapy.
Methods
Patients
Under an institutional review board approved protocol patients >70 years of age with pathologic diagnosis of rectal cancer who received SCRT were retrospectively identified. Majority of patients were staged by endorectal ultrasound (EUS) or magnetic resonance imaging (MRI).
Radiation treatment
SCRT was delivered in 5 fractions. Treatment was delivered by intensity modulated radiation therapy (IMRT) with 20 Gy/5 fractions to the mesorectum PTV and 25 Gy/5 fractions to the primary tumor PTV. No treatment was directed to the iliac nodes. Acute toxicities were graded by Common Terminology Criteria for Adverse Events (CTCAE) version 4.
Surgery
Surgery was either abdominoperineal resection (APR), low anterior resection (LAR), or trans-anal endoscopic microsurgery (TEMS) performed in a high volume, tertiary hospital.
Response assessment
Pathologic response was assessed by quantitation of residual tumor, necrosis, and lymphocyte infiltrate as per practice of the pathology department. Clinical tumor response was assessed by MRI, CT or PET-CT scans using RECIST criteria, colonoscopy, and/or digital rectal examination. Symptomatic response of SCRT monotherapy patients was assessed by radiation oncology or colorectal surgery providers.
Statistical methods
Overall and progression free survival were evaluated by Kaplan-Meier and compared by log-rank, with a P value <0.05 set as significant.
Results
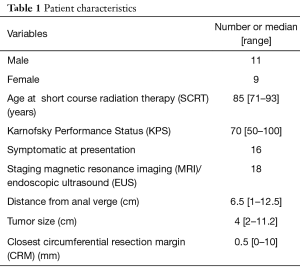
Twenty patients were identified (Table 1). Median follow up with clinical exam including CEA, imaging, or colonoscopy was 12 months No patient had metastatic disease at time of radiation. Rationale for SCRT was frailty (at least 2 significant co-morbidities) in 7 patients, cardio-pulmonary comorbidity in 5, quality of life concerns/lack of social support in 3, dementia with residence in a skilled nursing facility in 3, and chronic kidney disease in 2.
Full table
Median overall and local progression-free survival at 1 and 2 years was 75% and 54%, and 70% and 54% respectively. There was no significant different in survival between patients who received surgery, and those treated with SCRT alone (P=0.8).
Patients treated with SCRT monotherapy
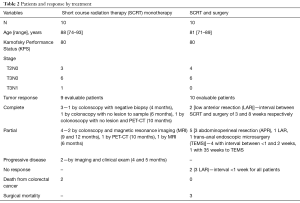
Ten patients were treated with SCRT alone (Table 2). One was planned for LAR but had a complete response by colonoscopy. Two patients died as a result of progressive colorectal cancer at ages 90 and 93, respectively both approximately 5 months after SCRT.
Full table
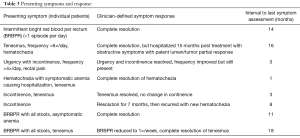
Of the 8 SCRT monotherapy patients symptomatic at presentation, 5 had a clinician determined symptomatic response (Table 3). The two asymptomatic patients did not develop symptoms post-treatment. No patient developed isolated pelvic node recurrence.
Full table
Patients treated surgically
Ten patients underwent surgery (Table 3). Surgery was not implemented as salvage. One patient classified as a pCR received SCRT and subsequent LAR after an up-front TEMS left gross residual disease. Five patients were deemed to have down-staging. Three patients had post-surgical complications; 2 with partial small bowel obstruction, one requiring ileostomy, and third with hemorrhage requiring adrenalectomy. No patient who underwent surgery died from colorectal cancer, and 1 developed oligometastatic disease to the liver. Three patients died from surgical complications; two at age 83 and 79 secondary to post-operative myocardial infarction, both during the admission for surgery, and one at age 87 due to infection within 2 weeks. There were no intra-operative complications noted for these 3 patients.
Radiation related toxicity
Fifteen patients reported no toxicity, three had exacerbation of diarrhea consistent with CTCAE Grade 2 proctitis, and one patient with severe baseline symptoms developed Grade 3 proctitis. One patient had symptoms consistent with CTCAE Grade I cystitis. No patient required hospitalization for toxicity management.
Discussion
Rectal cancer is often symptomatic (80% of patients in this series were symptomatic at presentation) and presents difficult management decisions. Unlike symptoms from prostate cancer, also common in the elderly, which may have urinary side effects or even metastatic disease managed with relatively well tolerated hormonal therapy, the choice of therapy for frail patients with rectal cancer is more onerous. This short series is the first report to our knowledge demonstrating the potential utility of SCRT monotherapy as up-front therapy in elderly patients.
Previous reports have shown that SCRT decreases the local recurrence rate with the use of total mesorectal excision (4); however, population-based analyses of have not shown a benefit of TME surgery in elderly patients (>74 years of age), which correlated with increased 30- and 60-day mortality (3). Our data support the vulnerability of older patients, with a quite high rate of complications and 3 peri-operative deaths. Generalization is limited with small number of patients, but even in a tertiary hospital with a multidisciplinary team it is difficult to predict which patients will tolerate intensive therapy.
The anti-tumor effect of SCRT in rectal cancer also increases with time. A report of older patients with T4 lesions showed high rates of R0 resection and pathologic down staging in at least 58% of patients who did not receive systemic therapy with mean time to surgery approximately 6 weeks (5). Analysis of the Stockholm III trial, a randomized trial with 2 arms of different intervals between SCRT and resection, reported an 11.8% complete pathologic response rate with surgery delayed 4–8 weeks post treatment, compared to 1.7% for immediate surgery (6). In this series the patients who had a complete response all had an interval of at least 3 weeks post SCRT, and the patients who had a complete response in the non-surgical group maintained this for at least 6 months. The fact that there was progression in 2 patients also highlights that there are risks.
Reports also show the efficacy in symptomatic management with SCRT. A prospective trial of 18 patients with obstructive disease reported excellent patient-identified symptomatic response following SCRT as monotherapy with low rates of acute toxicities, though a slightly higher rate of grade 3 proctitis compared to this series (16% vs. 5%) (7). Patients in this series were in less dire circumstances, but also had favorable symptomatic responses. Blood loss either completely resolved or substantially improved in 5/8 monotherapy patients with this symptom, and no patient required transfusions after SCRT. Radiation was well tolerated with minimal acute effects and no hospitalizations, including 3 patients with dementia already in a skilled facility.
A less invasive surgical procedure, TEMS, has been studied as an alternative option and comes with some risks. TEMS is inadequate control as monotherapy for T2 lesions (8), and interest in combining SCRT with TEMS has been tempered by high wound dehiscence rates of 13–50% (9,10).
We acknowledge the limitations our study, including the retrospective nature, lack of uniform follow up, and small numbers. However, the tolerability, symptomatic improvement, and proportion of patients needing no further intervention support SCRT as initial therapy in elderly patients, followed by scheduled surveillance. A prospective trial is being developed to address this question in elderly patients.
Conclusions
SCRT is a well-tolerated, effective regimen for rectal cancer in the very elderly with a small but real pathologic complete response rate and symptom improvement without further local therapy. SCRT followed by a watch and wait warrants further evaluation in prospective trials.
Acknowledgements
We would like to acknowledge Laura Finger for assistance in preparing this manuscript.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004;351:1731-40. [Crossref] [PubMed]
- Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 2012;30:3827-33. [Crossref] [PubMed]
- Rutten HJ, den Dulk M, Lemmens VE, et al. Controversies of total mesorectal excision for rectal cancer in elderly patients. Lancet Oncol 2008;9:494-501. [Crossref] [PubMed]
- Kapiteijn E, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001;345:638-46. [Crossref] [PubMed]
- Radu C, Berglund A, Påhlman L, et al. Short-course preoperative radiotherapy with delayed surgery in rectal cancer - a retrospective study. Radiother Oncol 2008;87:343-9. [Crossref] [PubMed]
- Pettersson D, Lörinc E, Holm T, et al. Tumour regression in the randomized Stockholm III Trial of radiotherapy regimens for rectal cancer. Br J Surg 2015;102:972-8; discussion 978. [Crossref] [PubMed]
- Picardi V, Deodato F, Guido A, et al. Palliative Short-Course Radiation Therapy in Rectal Cancer: A Phase 2 Study. Int J Radiat Oncol Biol Phys 2016;95:1184-90. [Crossref] [PubMed]
- Elmessiry MM, Van Koughnett JA, Maya A, et al. Local excision of T1 and T2 rectal cancer: proceed with caution. Colorectal Dis 2014;16:703-9. [Crossref] [PubMed]
- Smart CJ, Korsgen S, Hill J, et al. Multicentre study of short-course radiotherapy and transanal endoscopic microsurgery for early rectal cancer. Br J Surg 2016;103:1069-75. [Crossref] [PubMed]
- Arezzo A, Arolfo S, Allaix ME, et al. Results of neoadjuvant short-course radiation therapy followed by transanal endoscopic microsurgery for t1-t2 n0 extraperitoneal rectal cancer. Int J Radiat Oncol Biol Phys 2015;92:299-306. [Crossref] [PubMed]


