Ethnic disparities in the risk of colorectal adenomas associated with aspirin and statin use: a retrospective multiethnic study
Introduction
Colorectal adenocarcinoma is the third most common cancer and the third leading cause of cancer-related deaths in both men and woman. In 2011, there were 141,210 new cases of colorectal cancer and 49,380 colorectal cancer-related deaths. It is estimated that a previous colorectal adenocarcinoma diagnosis was present in almost 1.2 million men and women living in the U.S. as of January 1, 2012, with 1- and 5-year relative survival rates of 83% and 64%, respectively (1). One of the unique aspects of colon cancer is that most arise from pre-malignant adenomas in an adenoma-carcinoma sequence. Initially, the colonic mucosa undergoes chromosomal mutations involving genes such as APC, k-ras and DCC, among others. The mucosa then proliferates into an adenoma and after additional mutations in genes such as p53, the adenoma transforms in a carcinoma (2). Since most colorectal cancers follow this adenoma-carcinoma time sequence, colonoscopy has become an intervention to detect and remove colorectal adenomas (CRA) before they become cancerous. While the use of screening tests prevention of colorectal cancer or detection and at an earlier stage is recommended, only 59% of men and women 50 years of age and older receive colorectal cancer screening according to published guidelines. Less than 40% of these cases are diagnosed at a local stage when treatment has a higher success rate. The benefits of early detection are documented in the medical literature. One study showed that colonic polypectomy through colonoscopy reduced colon cancer mortality by 53% (3).
In comparison to whites, all other racial and ethnic groups are less likely to be diagnosed with colorectal cancer at an early stage when treatment is more successful. Whether this discrepancy is due to true difference between these groups or is secondary to lack of access of care remains undetermined. Epidemiological studies that assess this discrepancy are crucial to determining the true nature of this racial disparity. According to the U.S. Census Bureau, Hispanics currently comprise 17% of the United States population at 53 million, and is projected to grow to 31% of the U.S. population by 2060 to an estimated 128.8 million people (4). In the US, Hispanics are the largest and fastest growing minority group. In the total Hispanic population, the incidence of colorectal cancer is 46.9 per 100,000 with a mortality of 15.3 per 100,000 (1).
Aspirin and statins may both reduce the incidence of colorectal cancer (5). Although data on the inverse association of daily aspirin and statin therapy exists in white and black patients, scarce data exists on their effect on the incidence of CRA in the Hispanic patient population. In this study we assessed whether reported use of these medications was associated with the incidence of CRA in our multi-racial hospital.
Methods
Patients
Following Institutional Review Board (IRB) approval at Nassau University Medical Center, a 530-bed tertiary care teaching hospital in East Meadow, New York, a retrospective chart review was performed between July 1, 2009 and March 21, 2011. We established a database of 1,843 patients undergoing screening or diagnostic colonoscopy. Only patients with listed medications were used for analysis. Patients with colon cancer, inflammatory bowel disease, or incomplete colonoscopies were excluded from this study. A total of 1,495 patients were included in the analysis on statin use, 1,038 patients were included in the analysis on aspirin use and 672 patients were included in the analysis of use of both statin and aspirin. Data were collected on patient demographics and potential risk factors for adenoma including age, sex, race, body mass index (BMI), diabetes, hypertension, smoking, alcohol, and family history of colorectal cancer along with aspirin and/or statin use. Recorded colonoscopy findings included presence of adenoma, adenoma ≥10 mm, two or more adenomas, adenoma present in proximal colon, adenoma present in distal colon, largest adenoma in the proximal colon and largest adenoma in the distal colon.
Statistical analysis
Comparisons between categorical variables were made using a chi square test and a t-test was used for comparisons between continuous variables. Unconditional logistic regression was used to generate age-, gender-and race-adjusted odds ratios and their 95% confidence intervals (CI) comparing medication users with non-users. Statistical analyses were performed with SAS 9.3 software.
Results
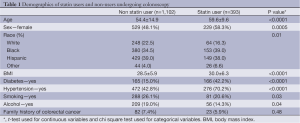
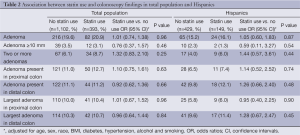
Table 1 shows the demographic characteristics of statin users and non-users. The mean age was higher among statin users than non-users (59.6 vs. 54.4, P<0.0001). A larger proportion of the statin users (58.3%, n=229) vs. non-users (48.1%, n=529) were female (P=0.0005). Users and non-users also differed in their racial breakdown (P=0.01), all metabolic and environmental factors including BMI (P<0.0001), presence of diabetes (P<0.0001), hypertension (P<0.0001), smoking status (P=0.03) and alcohol use (P=0.04). Statin users and non-users did not differ in their family history of colorectal cancer. Table 2 shows the association between statin use and colonoscopy findings, adjusted for age, sex, race, BMI, diabetes, hypertension and smoking or alcohol use. No associations were seen between any of colonoscopy findings and use of statin in the total population or in Hispanics
Full table
Full table
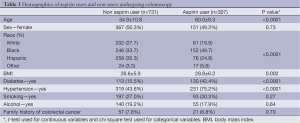
Table 3 shows the demographic characteristics of aspirin users and non-users. The mean age was higher among aspirin users than non-users (60.0 vs. 54.9, P<0.0001). There was no significant difference between the groups in terms of gender breakdown. Users and non-users also differed in their racial breakdown (P<0.0001), BMI (P=0.002), presence of diabetes (P<0.0001) and hypertension (P<0.0001). Aspirin users and non-users did not differ in any other factors. Table 4 shows the association between aspirin use and colonoscopy findings, adjusted for age, sex, race, BMI, diabetes, hypertension and smoking or alcohol use. Compared to non-users of aspirin, those who used aspirin had an increased risk for having two or more adenomas [odds ratio (OR) =1.73, 95% CI: 1.00, 2.99, P=0.05] and presence of an adenoma in the proximal colon (OR =1.66, 95% CI: 1.07, 2.58, P=0.02). No associations were seen between any other colonoscopy findings and aspirin use in the total population. There were no significant associations between aspirin use and colonoscopy findings in Hispanics.
Full table

Full table
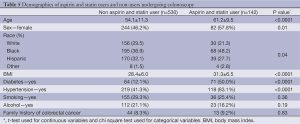
Table 5 shows the demographic characteristics of statin and aspirin users and non-users. The mean age was higher among users of both medications than users of neither (61.2 vs. 54.1, P<0.0001). There was a difference between the groups in terms of gender breakdown (P=0.01), racial breakdown (P=0.04), BMI (P=0.002), presence of diabetes (P<0.0001) and hypertension (P<0.0001). Medication users and non-users did not differ in any other factors. Table 6 shows the association between users of both medications and colonoscopy findings, adjusted for age, sex, race, BMI, diabetes, hypertension and smoking or alcohol use. Compared to non-users of either medication, those who used both had an increased risk for having two or more adenomas (OR =2.56, 95% CI: 1.21, 5.39, P=0.01). No associations were seen between any other colonoscopy findings and aspirin use in the total population. In the Hispanic population, compared to non-users of either medication, those who used both had an increased risk for having two or more adenomas (OR =19.04, 95% CI: 1.30, 280.09, P=0.03), adenoma present in the distal colon (OR =5.75, 95% CI: 1.64, 20.21, P=0.01) and largest adenoma in distal colon (OR =5.75, 95% CI: 1.64, 20.21, P=0.01). No other associations were seen in the Hispanic population.
Full table
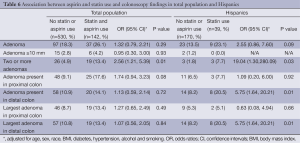
Full table
Discussion
To our knowledge this is the first study assessing aspirin and statin use in a Hispanic population. We found that statin use was not associated with any colonoscopy findings, though aspirin use increased the risk for two or more adenomas and adenoma in the proximal colon in our total population, but did not see the same results when restricting the analysis to Hispanics. An increased risk for two or more adenomas was also seen in the total population for users of both statins and aspirin. In Hispanics, use of both medications was associated with two or more adenomas, adenoma present in the distal colon and largest adenoma in distal colon.
There have been many trials discussing the relationship between aspirin/non-steroidal anti-inflammatory drugs (NSAIDs) and colorectal adenoma/carcinomas in predominant white patient populations. One recent meta-analysis combined four randomized double-blinded placebo trials that evaluated aspirin and prevention of CRA. The results showed that aspirin users had a pooled risk ratio of 0.83 (95% CI: 0.72, 0.96) for any adenoma, with an absolute risk reduction of 6.7% compared to placebo (6). They concluded that aspirin is effective for the prevention of CRA in patients with a history of these lesions. There have also been studies looking specifically at NSAIDS and colon cancer. Patients taking 200mg BID of Celecoxib had a reduced rate of sporadic CRA (RR: 0.67, 95% CI: 0.59, 0.77), while those taking 400 mg BID also had a reduced risk of sporadic CRA (RR: 0.55, 95% CI: 0.48, 0.64) (7). Unfortunately, there are limited randomized trials looking at non-COX-2 selective NSAIDS. One study showed that the NSAID, sulindac, reduced the risk of polyp formation in patients with familial adenomatous polyposis (8).
There are some trials showing that aspirin did not reduce the incidence of colon cancer and none demonstrating an association with the presence of adenomas. One study showed that alternate day 100 mg aspirin did not reduce the risk of colon cancer (9), while another trial revealed that aspirin given for five years of duration did not reduce the risk of colon cancer (10). It is theorized that these trials did not show risk reduction because of low doses of ASA (11). Though it is theorized that the mechanism stems from aspirin/NSAIDs ability to block COX-2 enzymes, which are expressed in the majority of colonic adenomas and not in normal colonic tissue, it should be noted that the mechanism of colon cancer prevention through aspirin/NSAIDs use is unclear (12).
There have also been many studies looking at the relationship between statins and colorectal cancer risk. One case-control study showed that statin use for five years was associated with a 47 percent relative risk reduction of colorectal cancer (13). The proposed anti-tumor mechanism of statins is likely due to a pleiotropic effect on cells. Statins inhibit HMG-CoA reductase, decreasing cellular levels of melvonate and result in cells unable to generate products involved in cell functioning. Statins have also been shown to induce apoptosis in tumor cells (14). Despite these findings and proposed mechanism for protection, there are several studies showing no reduction of colorectal cancer risk. A meta-analysis including random controlled trials, cohort, and case control studies with more than 1.5 million participants, showed no association with statin use and risk of colorectal cancer. However, sub-group analysis of just case control studies did show a modest reduction in the risk of colon cancer (RR: 0.91; 95% CI: 0.87, 0.96) (15).
Statins have also been reported to increase the risk of adenoma formation with a large prospective randomized trial demonstrating that statin use increased the risk of adenoma formation. However, this was not found among patients also taking Celebrex, and it was suggested that the significant antitumor effect Celebrex produces seemed to counteract the tumor-promoting effect of statins. The results overall showed that statin use for greater than three years showed a 40% increase in adenoma detection during five years of surveillance (RR: 1.39 95% CI: 1.04, 1.86) (16).
Though our study showed increased colonoscopy findings with statin use, there were several limitations to the study. Limitations of our study include a retrospective design and small sample size, particularly in the analysis looking at combined medication use in Hispanics. Some of the OR CIs were wide, most likely due to sample size limitations. Additionally, a further description of Hispanic immigration also was not defined in our study and Hispanics can be represented by a diverse ethnic population. There is always a possibility of selection bias, and that the patients studied were a population preselected to develop adenomas while on statins. Another weakness to our study is that the type of statin used was unknown, as the type of statin may influence tissue response. Lipophilic statins are more likely to achieve higher drug levels in nonhepatic tissues, thus being more likely to alter the biology of colorectal mucosa than hydrophilic statins (16). Strengths include a diverse patient population sample representative of the actual growing US population. Additionally, our analysis controlled for multiple confounding data that could influence adenoma detection.
In summary, we have determined that combined aspirin and statin use, along with the sole use of aspirin, does not protect against CRA and was associated with their presence in the Hispanic population. It is unclear why combined use of aspirin and statin medications was associated with colonoscopy findings in Hispanics. Our findings may be due to environmental factors such as dietary, colonic flora, or genetic susceptibility. Overall, we have demonstrated there is an association with the presence of CRA and aspirin/statin use, and our results support further investigation of this finding in the Hispanic population.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- American Cancer Society. Cancer Treatment and Survivorship Facts & Figures 2012-2013. Atlanta: American Cancer Society, 2012.
- Cho KR, Vogelstein B. Genetic alterations in the adenoma--carcinoma sequence. Cancer 1992;70:1727-31. [PubMed]
- Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687-96. [PubMed]
- United States Census Bureau. Profile America Facts for Features. 30 July, 2013. Available online: www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb13-ff19.html
- Mansouri D, McMillan DC, Roxburgh CS, et al. The impact of aspirin, statins and ACE-inhibitors on the presentation of colorectal neoplasia in a colorectal cancer screening programme. Br J Cancer 2013;109:249-56. [PubMed]
- Cole BF, Logan RF, Halabi S, et al. Aspirin for the chemoprevention of colorectal adenomas: meta-analysis of the randomized trials. J Natl Cancer Inst 2009;101:256-66. [PubMed]
- Bertagnolli MM, Eagle CJ, Zauber AG, et al. Celecoxib for the prevention of sporadic colorectal adenomas. N Engl J Med 2006;355:873-84. [PubMed]
- Giardiello FM, Hamilton SR, Krush AJ, et al. Treatment of colonic and rectal adenomas with sulindac in familial adenomatous polyposis. N Engl J Med 1993;328:1313-6. [PubMed]
- Cook NR, Lee IM, Gaziano JM, et al. Low-dose aspirin in the primary prevention of cancer: the Women’s Health Study: a randomized controlled trial. JAMA 2005;294:47-55. [PubMed]
- Gann PH, Manson JE, Glynn RJ, et al. Low-dose aspirin and incidence of colorectal tumors in a randomized trial. J Natl Cancer Inst 1993;85:1220-4. [PubMed]
- Dubé C, Rostom A, Lewin G, et al. The use of aspirin for primary prevention of colorectal cancer: a systematic review prepared for the U.S. Preventive Services Task Force. Ann Intern Med 2007;146:365-75. [PubMed]
- Chan AT, Ogino S, Fuchs CS. Aspirin and the risk of colorectal cancer in relation to the expression of COX-2. N Engl J Med 2007;356:2131-42. [PubMed]
- Poynter JN, Gruber SB, Higgins PD, et al. Statins and the risk of colorectal cancer. N Engl J Med 2005;352:2184-92. [PubMed]
- Boudreau DM, Yu O, Johnson J. Statin use and cancer risk: a comprehensive review. Expert Opin Drug Saf 2010;9:603-21. [PubMed]
- Bonovas S, Filioussi K, Flordellis CS, et al. Statins and the risk of colorectal cancer: a meta-analysis of 18 studies involving more than 1.5 million patients. J Clin Oncol 2007;25:3462-8. [PubMed]
- Bertagnolli MM, Hsu M, Hawk ET, et al. Statin use and colorectal adenoma risk: results from the adenoma prevention with celecoxib trial. Cancer Prev Res (Phila) 2010;3:588-96. [PubMed]


