Walking to recovery: the effects of missed ambulation events on postsurgical recovery after bowel resection
Introduction
As healthcare in the United States transforms towards an outcomes based reimbursement system, process improvement has become an important aspect for financial sustainability (1,2). The goal of any healthcare process modification is improving the value of the healthcare encounter (3). Value, in medicine, is defined by patient outcomes divided by the overall cost. Efforts to reduce inpatient complications and lengths of stay (LOS) ultimately reduce costs and therefore improve the value quotient. The implementation of an enhanced recovery after surgery (ERAS) protocol, designed in Denmark in the 1990s to streamline processes of the perioperative period for surgical patients, has improved the value in abdominal surgery (4). In the last 15 years, many health systems across the globe have implemented many, if not all, of the ERAS concepts with significant improvement in surgical outcomes (5,6). However, it is not always clear which aspect of the ERAS protocol is the most effective in reducing LOS and/or reducing overall complications.
We sought to focus specifically on the effects of postsurgical ambulation on inpatient LOS for patients undergoing bowel resection surgery. The multiple physiological benefits of patient ambulation have been documented including the prevention of muscular and cardiovascular deconditioning (7), reducing the risk of pulmonary and thromboembolic events (8), and stimulating gastrointestinal recovery through prokinetic effects (9).
We developed a low-cost ambulation team dedicated solely to ensure ambulation goals of 3 times per day were met. These ambulation technicians had no formal training (i.e., physical therapy, nursing, physician assistant, etc.) but were educated on patient safety, fall prevention, and proper lifting techniques. Any patient with ambulation restrictions was seen by the physical therapy team. With the focus on improving the overall value of our process, we evaluated the impact of ambulation participation on post-surgical outcomes.
Methods
Between January 1, 2014 and December 1, 2016, all patients undergoing an elective small intestine or colon resection procedure were offered daily ambulation assistance by dedicated ambulation technicians. Patient’s rights were preserved and were allowed to refuse ambulation if they did not want to participate. Clinical data was gathered prospectively and included patient participation, patient refusal, missed ambulation events, and overall LOS. LOS was recorded as total number of hours admitted to the hospital. An ambulation event was considered successful if a distance greater than 10 feet was achieved. The total distance for each ambulation event and the number of mobilizations per day was recorded. The research was approved by the Institutional Review Board (IRB) and all discharging physicians were blinded to the specific data collected and to ambulation participation. All patients, except for one, were fully ambulatory prior to surgery with one needing assistance to ambulate.
The optimal daily ambulation was determined to be 3 times per day. The three possible scores were an ambulation, a refusal, and a missed opportunity. A refusal was any time an ambulation technician offered to assist the patient to ambulate, but the patient specifically refused. Missed opportunities included a patient absent from his or her room when the ambulation technician arrived, less than 10 feet were ambulated for the session, or the ambulation team was not available.
The ambulation completion percentage, refusal percentage, and missed percentages were compared, to the total possible encounters during the patient’s stay. The refusal to completed ambulation ratio was calculated by comparing refusals against the total number of successful mobilizations. This calculation was performed to compare solely the patient’s participation without regard to absences by the ambulation team. Other data analysis compared the number of mobilizations per LOS day and mobilization distance per LOS day against overall LOS.
Skewness and kurtosis statistics were performed on all continuous variables to assess the assumption of normality. Any skewness or kurtosis statistic above an absolute value of 2.0 was assumed non-normal. Levene’s Test of Equality of Variances was used to test the assumption of homogeneity of variance. In the event that a statistical assumption of a parametric between-subject comparison occurred, a non-parametric Mann-Whitney U test was utilized. Biserial and Spearman’s rho correlations were used to establish associations with ambulation. All analyses were conducted using SPSS Version 22 (Armonk, NY: IBM Corp.) and statistical significance was assumed at a Bonferroni corrected alpha value to adjust for multiple comparisons, when appropriate.
Results
Between January 1, 2014 and December 1, 2016, 127 consecutive patients underwent bowel resection within an ERAS protocol. There were 68 women and 59 men. Ages ranged from 22 to 89 years with a median of 61 years. The 127 patients were divided into 68 laparoscopic procedures and 59 open procedures (see Table 1).

Full table
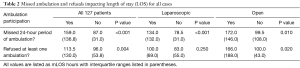
When evaluating the entire cohort, the median LOS (mLOS) for those that missed a day of ambulation (i.e., three consecutive ambulation events) was 159 hours (6.6 days) compared to 87 hours (3.6 days) for those that ambulated every day (P<0.001). When selecting those that underwent a laparoscopic surgery and missed a 24-hour period of ambulation, the mLOS increased from 78.5 hours (3.3 days) to 134.0 hours (5.6 days) (P<0.001), whereas the LOS for the open procedures increased from 99.5 hours (4.1 days) to 172 hours (7.2 days) (P=0.010) (see Table 2). For the cancer vs. noncancer cohorts that similarly missed a full day of ambulation, the cancer patients increased their mLOS from 78.0 hours (3.3 days) to 146.0 hours (6.1 days), P<0.001, and the noncancer patients increased their mLOS from 95.5 hours (4.0 days) to 172.0 hours (7.2 days) (P<0.001) (see Table 3).
Full table
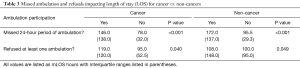
Full table
For those that specifically refused to participate in at least one ambulation event, the LOS increased from 96 hours (4.0 days) to 113.5 hours (4.7 days) for those that did not refuse (P=0.004). When evaluating those that underwent an open procedure, the LOS increased from 100.0 hours (4.2 days) to 166.0 hours (6.9 days) (P=0.020). There was no significant difference in LOS for laparoscopic patients that refused ambulation (see Table 2). When evaluating for cancer patients, mLOS increased from 95.0 hours (4.0 days) to 119.0 hours (5.0 days) (P=0.040), when ambulation was refused compared to an increase in mLOS from 100.0 hours (4.2 days) to 108.0 hours (4.5 days), P=0.049, for noncancer patients (see Table 3).
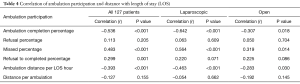
The ambulation completion percentage, defined as the ratio of completed ambulation attempts to the total possible opportunities, was found to have a negative correlation on LOS when comparing all 127 patients (r=−0.536, P<0.001). When comparing laparoscopic patients, the ambulation completion ratio was similar (r=−0.642, P<0.001) to that of the open cohort (r=−0.307, P=0.018) (see Table 4).
Full table
Missed ambulation attempts correlated with greater mLOS. As the ratio of missed ambulation attempts to total ambulation attempts increased, the LOS increased for all patients (r=0.483, P<0.001). As the ratio of refusals to successful ambulation attempts increased for all patients, mLOS increased (r=0.299, P=0.001). Furthermore, as the ratio of the combined refusals and missed ambulation attempts compared to total ambulation attempts increased, LOS increased for all patients (r=0.51, P=0.001). There was no statistical difference when comparing cancer versus non-cancer patients or comparing laparoscopic versus open procedures (see Table 4).
Participation in ambulation for all three ambulation sessions each day was a predictor of a reduced LOS. As the distance mobilized per LOS day while in the hospital increased, LOS subsequently decreased for all patients (r=−0.393, P<0.001). Ambulation distance per LOS day remained a negative predictor for the laparoscopic cohort (r=−0.463, P<0.001) and the open patients (r=−0.283, P=0.030) (see Table 4).
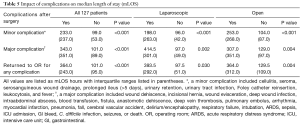
As expected, complications predicted greater mLOS during the hospital stay. The development of a major complication in the recovery period correlated with an increase in mLOS from 101.0 hours (4.2 days) to 343.0 hours (14.3 days), P<0.001. Additionally, patients that returned to the operating room for a similar operation within 90 days were noted to have had an increased mLOS during their initial hospital stay. The initial mLOS was 101 hours (4.2 days) for those with no return to the operating room within 90 days vs. 364 hours (15.2 days) for those that eventually required reoperation, P<0.001 (see Table 5).
Full table
When evaluating inpatient variables, increasing use of narcotics, measured using total morphine equivalence (TME), were found to have a higher mLOS (r=0.548, P<0.001). Additionally, patients who used a patient-controlled analgesia (PCA) pump (r=0.213, P=0.011) correlated with a higher mLOS. Interestingly, patients with a higher average reported pain score (r=−0.284, P=0.006) had a lower mLOS. Clinically, patients with a history of chronic obstructive pulmonary disease (COPD) (r=0.251, P=0.003), and patients with a history of diabetes type I (r=0.160, P=0.041) were all found to have higher mLOS (see Table 6).
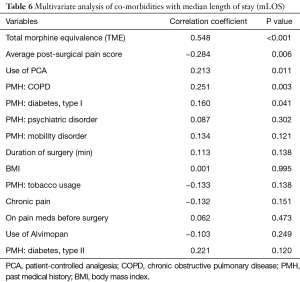
Full table
When clinical variables that impacted the ambulation completion percentage were evaluated, increasing use of narcotics (r=−0.278, P=0.036) and a clinical history of COPD (r=−0.199, P=0.049) both led to a decreased percentage of successful ambulation attempts (see Table 7).
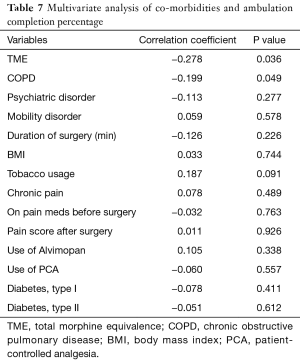
Full table
When comparing refusal percentage, 74 patients (58%) were in the low refusal group (<30%) vs. 53 patients (42%) in the high refusal group (>30%). The laparoscopic group had 22 patients (32%) in the high refusal group vs. 31 patients (53%) in the open group. Notable findings included an increase in mLOS from 100.5 hours (4.2 days) to 143.0 hours (6.0 days) for patients that refused greater than 30% of ambulation attempts. Patients that refused greater than 30% of ambulation attempts were 2.38 times more likely to have a diagnosis of a psychiatric disorder [P=0.03; 95% confidence interval (CI), 1.10–5.14]. Patients who had a complication noted in their discharge summaries tended to refuse greater than 30% of ambulation attempts. Patients in the greater refusal cohort were 2.85 times more likely to experience a minor complication (P=0.02; 95% CI, 1.14–7.14) and 2.79 times more likely to experience either a minor or major complication (P=0.009; 95% CI, 2.79–6.13), (see Table 8).
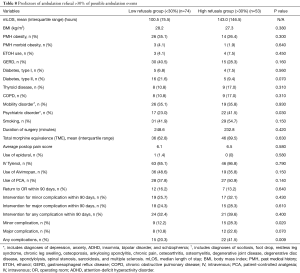
Full table
Discussion
The enhanced recovery philosophy emphasizes a multimodal approach to improve surgical outcomes and reduce cost. This study focuses on one aspect of ERAS; specifically, the impact of ambulation after bowel resection surgery.
Our analysis found a correlation with failure to ambulate and longer mLOS. For those patients that missed at least 1 day of ambulation, their mLOS increased by 2.3 days for the laparoscopic cohort and by 3.1 days for the open surgical cohort. Additionally, as they missed each ambulation attempt, a direct correlation with increased LOS resulted for the laparoscopic cohort (r=0.564, P<0.001) and the open surgical cohort (r=0.319, P=0.014). As a corollary, refusing at least one ambulation in the hospital increased LOS by 2.7 days for the open surgical cohort. As patients refused a greater number of ambulation visits, there was an increased LOS in the hospital for all patients (r=0.299, P=0.001). Conversely, ambulating a greater distance decreased the mLOS in both the laparoscopic cohort (r=−0.463, P<0.001) and the open cohort (r=−0.283, P=0.030).
The amount of narcotic used influenced mLOS and ambulation participation. Both TME narcotic usage (TME) used (r=0.548, P<0.001) and use of a PCA following surgery (r=0.213, P=0.011) were strong predictors for increased LOS. In addition, post-surgical narcotic usage (TME) correlated with decreased participation in ambulation completion (r=−0.278, P=0.036). As a corollary, patients in the low refusal group (see Table 7) received a significantly lower amount of narcotics following surgery when compared to the high refusal group. A higher average post-surgical pain score also correlated with a decreased mLOS (r=−0.284, P=0.006) suggesting that reducing pain scores through increase use of narcotics may prolong mLOS. This data further supports the value of multi-modality pain control including non-narcotic pain medication to decrease narcotic use and still ensure lower pain scores.
Pre-operative health status also influenced mLOS. Those with COPD (r=−0.199, P=0.049) and those with psychiatric disorders (P=0.03; 95% CI, 1.10–5.14) had lower ambulation participation and increased LOS. Those with insulin dependent diabetes mellitus had a longer mLOS (r=0.160, P=0.041). Other co-morbidities including body mass index (BMI), tobacco use, chronic pain, prior narcotic use, and mobility limitations did not impact mLOS. Lee et al. previously observed an impact on surgical outcomes in those with a psychiatric diagnosis (10). In our cohort, those being treated for depression, anxiety, bi-polar disease, attention-deficit hyperactivity disorder (ADHD), insomnia, and schizophrenia were noted to have a longer mLOS and an increased refusal rate .
Refusal to ambulate correlated with those that eventually developed a complication. Those that eventually developed a post-operative complication were more likely to be in the higher refusal group, P=0.009. Thorn et al. suggested that patient compliance may be a marker of underlying complications. If patients are not engaged in their recovery, there may be a physiologic reason for refusal (i.e., a developing abscess). They suggest an active pursuit of the reasons for those not participating in an enhanced recovery program (11). Additionally, all enhanced recovery programs rely on optimally performed surgeries. Intraoperative decisions impact outcomes (12). Ambulation refusal may be an early marker of potential complications along with other physiologic parameters.
Cancer and noncancer cohorts were compared separately to elucidate any differences in outcomes. Overall, a cancer diagnosis did not significantly impact mLOS compared to non-cancer diagnoses, though, in patients that missed a 24-hour period without ambulation, the mLOS for a cancer patient was 6.1 vs. 7.2 days for non-cancer patients. Sixty-five percent of cancer patients refused less than 30% of ambulation attempts compared with only 51% of noncancer patients who refused less than 30% of ambulation attempts.
Active patient participation both mentally and physically in ERAS is important. Forsmo et al. noted engaging their patient cohort significantly contributed to shorter LOS. An active role in recovery reduces LOS vs. a passive approach (13). Bakker et al. highlighted the importance of adherence to the ERAS protocols for optimal success including patient participation. Adherence requires the patient care team, the patient, and the patient’s social support team to be engaged in all aspects of recovery (14). A recent study which focused solely on laparoscopic colorectal surgery by Pisarska et al. (15) found positive correlations between increasing compliance in mobilization and decreases in complication rate. Additionally, they found evidence suggesting compliance in early ambulation improved tolerance of oral diet on the first postoperative day and a decreased LOS. Delaney et al. highlighted the impact of ERAS for both open and laparoscopic colon surgery. LOS and complications were reduced by entering all colon resection patients into an ERAS protocol and ensuring compliance across the multidisciplinary spectrum (16).
From a financial perspective, reduced postsurgical complications and decreased LOS decrease the resource use of additional inpatient days. In our current diagnosis-related group (DRG) formula for reimbursement, loss of revenue for the hospital system is determined by missed opportunities for income often caused by prolonged LOS. In 2010, the reimbursement for the hospital system for a partial colectomy was approximately $19,000 (17). Reduction in LOS in a DRG reimbursement model increases the opportunity for additional procedures to be performed and indirectly increases hospital income. However, the DRGs for a specific procedure may also be reduced if the LOS is not long enough (i.e., it is greater than 1 day less than geometric mean for that DRG). Recent data released by Becker’s Healthcare estimates the cost for an inpatient stay in Tennessee varies from $1280 to $1880 per day as an inpatient (18). A reduction in only 1 day from the LOS for calendar day for the surgical floor would still add significant value to the process and could be used to justify the cost of dedicated ambulation resources (19).
Our study also revealed three areas to improve compliance of our ERAS protocol. First, ambulation resources are critical to ensure ambulation compliance. Daily ambulation requires collaboration between hospital resources, patient education and available personnel. Second, aggressive non-opioid pain medication regimens are critical to maintain a low mLOS. The increasing use of narcotics especially with a PCA prolonged the LOS. Third, refusal of ambulation often predicted the development of a post-operative complication. The ambulation team does need to alert the surgical team of patient refusals as underlying complications may be identified in a more-timely fashion.
Our study does have several weaknesses. First, the study focused on a single surgical floor with a dedicated ambulation technician. The total number of cases was limited secondary to this limited focus and other bowel resection cases were not included if recovered on other floors. Second, we did not record the reason for patient refusal. Therefore, we cannot say if the refusal was due to poor pain control, active complications (fever, emesis, increasing oxygen dependence), patient choice or lack of effort by the ambulation team. Regardless of the reason, we focused on ambulation as a binary event that either occurred or did not. Patients were encouraged to ambulate beyond the 3 formal times with the ambulation team, but, if they occurred, we did not capture them. Finally, documentation of reasons for increased narcotic use was limited. The narcotic use was based on patient request and reported pain score though the higher pain scores were associated with lower mLOS.In summary, in our analysis of patients undergoing bowel resection surgery, participation in daily ambulation had a significant impact on ensuring a reduced LOS. Patient refusal to ambulate or missing an entire day of ambulation significantly increased the LOS. A dedicated ambulation team has allowed our institution to improve the value of care offered by improving clinical outcomes at minimal cost. Continued improvement in outcomes within an enhanced recovery program may come through focusing on ambulation participation, reducing narcotic use, and focusing on high-risk clinical groups.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The research was approved by the University of Tennessee Health Sciences Center Institutional Review Board (IRB) (No. 3983).
References
- Coffron MR. What’s next? The future of Medicare physician payment in the post-SGR era. Available online: http://bulletin.facs.org/2015/07/whats-next-the-future-of-medicare-physician-payment-in-the-post-sgr-era/
- Gottlober P. Medicare Hospital Prospective Payment System: How DRG Rates Are Calculated and Updated. Available online: http://oig.hhs.gov/oei/reports/oei-09-00-00200.pdf.
- ACS National Surgical Quality Improvement Program® (ACS NSQIP®). 2016. Available online: https://www.facs.org/quality-programs/acs-nsqip
- Kehlet H. Multimodal approach to control postoperative pathophysiology and rehabilitation. Br J Anaesth 1997;78:606-17. [Crossref] [PubMed]
- Lassen K, Soop M, Nygren J, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) Group recommendations. Arch Surg 2009;144:961-9. [Crossref] [PubMed]
- Spanjersberg WR, Reurings J, Keus F, et al. Fast track surgery versus conventional recovery strategies for colorectal surgery. Cochrane Database Syst Rev 2011. [PubMed]
- Killewich LA. Strategies to minimize postoperative deconditioning in elderly surgical patients. J Am Coll Surg 2006;203:735-45. [Crossref] [PubMed]
- Allen C, Glasziou P, Del Mar C. Bed rest: a potentially harmful treatment needing more careful evaluation. Lancet 1999;354:1229-33. [Crossref] [PubMed]
- Story SK, Chamberlain RS. A comprehensive review of evidence-based strategies to prevent and treat postoperative ileus. Dig Surg 2009;26:265-75. [Crossref] [PubMed]
- Lee DS, Marsh L, Garcia-Altieri MA, et al. Active Mental Illnesses Adversely Affect Surgical Outcomes. Am Surg 2016;82:1238-43. [PubMed]
- Thorn CC, White I, Burch J, et al. Active and passive compliance in an enhanced recovery programme. Int J Colorectal Dis 2016;31:1329-39. [Crossref] [PubMed]
- Oh HK, Ihn MH, Son IT, et al. Factors associated with failure of enhanced recovery programs after laparoscopic colon cancer surgery: a single-center retrospective study. Surg Endosc 2016;30:1086-93. [Crossref] [PubMed]
- Forsmo HM, Pfeffer F, Rasdal A, et al. Compliance with enhanced recovery after surgery criteria and preoperative and postoperative counselling reduces length of hospital stay in colorectal surgery: results of a randomized controlled trial. Colorectal Dis 2016;18:603-11. [Crossref] [PubMed]
- Bakker N, Cakir H, Doodeman HJ, et al. Eight years of experience with Enhanced Recovery After Surgery in patients with colon cancer: Impact of measures to improve adherence. Surgery 2015;157:1130-6. [Crossref] [PubMed]
- Pisarska M, Pedziwiatr M, Malczak P, et al. Do we really need the full compliance with ERAS protocol in laparoscopic colorectal surgery? A prospective cohort study. Int J Surg 2016;36:377-82. [Crossref] [PubMed]
- Delaney CP, Brady K, Woconish D, et al. Towards optimizing perioperative colorectal care: outcomes for 1,000 consecutive laparoscopic colon procedures using enhanced recovery pathways. Am J Surg 2012;203:353-5; discussion 355-6. [Crossref] [PubMed]
- Birkmeyer JD, Gust C, Baser O, et al. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health Serv Res 2010;45:1783-95. [Crossref] [PubMed]
- Rappleye E. Average cost per inpatient day across 50 states. Available online: http://www.beckershospitalreview.com/finance/average-cost-per-inpatient-day-across-50-states.html
- Stone AB, Grant MC, Pio Roda C, et al. Implementation Costs of an Enhanced Recovery After Surgery Program in the United States: A Financial Model and Sensitivity Analysis Based on Experiences at a Quaternary Academic Medical Center. J Am Coll Surg 2016;222:219-25. [Crossref] [PubMed]


