|
Original Article
Increasing disparity in colorectal cancer incidence and mortality among African Americans and whites: A state’s experience
Noelle K LoConte1,2, Amy Williamson1, Arlene Gayle2, Jennifer Weiss2, Ticiana Leal1,2, Jeremy Cetnar1,2, Tabraiz Mohammed2, Amye Tevaarwerk1,2, Nathan Jones1
1University of Wisconsin Carbone Cancer Center, Madison, WI; 2University of Wisconsin School of Medicine and Public Health, Madison, WI
Corresponding to: Noelle LoConte, MD. University of Wisconsin Hospital and Clinics 600 Highland Ave, CSC K4/548, Madison, WI 53792. Tel: 608-265-5883; Fax: 608-265-5883. Email: Ns3@medicine.wisc.edu.
|
|
Abstract
Objectives: To measure disparities between African Americans and whites in colorectal cancer incidence and mortality rates between 1995-2006 in Wisconsin.
Methods: Cancer incidence data were obtained from the Wisconsin Cancer Reporting System. Cancer mortality data were accessed from the SEER. Trends in incidence and mortality rates were calculated and changes in relative disparity were measured using rate ratios.
Results: The relative disparity in incidence grew from 1.0 in 1995 and 1.3 in 2006. The relative disparity in death rates for African Americans widened as well, from 1.2 to 1.5.
Conclusion: A persistent and widening colorectal cancer racial disparity exists.
Key words
colorectal cancer, epidemiology, disparities
J Gastrointest Oncol 2011; 2: 85-92. DOI: 10.3978/j.issn.2078-6891.2011.014
|
|
Introduction
Cancer health disparities, defined by the National Cancer
Institute (NCI) as “differences in the incidence, prevalence,
mortality, and burden of cancer and related adverse health
conditions that exist among specific population groups”
( 1), are an important and growing concern. Although
treatments for cancer are improving and cancer mortality
is decreasing, not all Americans benefit equally from these
successes ( 2). National organizations such as the NCI, US
Department of Health and Human Services, and American
Cancer Society have targeted the elimination of cancer
health disparities, as have many state comprehensive cancer
control plans ( 3). Disparities in colorectal cancer (CRC) are often highlighted as being a particular source of concern.
Nationwide CRC is the second leading cause of cancer
mortality and the fourth leading source of new cancer cases
( 4). African Americans experience higher CRC incidence
rates, leading some organizations to recommend screening
African Americans at age 45 ( 5). The most recent national
data from NCI’s Surveillance, Epidemiology, and End
Results (SEER) program shows that from 2002 to 2006 the
CRC incidence rate among white males was 58.2 cases per
100,000, while among African American men, the rate was
68.4. There is a similar disparity in mortality nationally
(death rate among white men of 21.4 per 100,000, compared
to 31.4 per 100,000 among African American men) ( 6).
Although national incidence and mortality rates for CRC
have been decreasing in recent years, the decrease has not
been as pronounced among African Americans as it has
been in whites ( 7, 8). There is also evidence that African
Americans present with more advanced stage disease at
diagnosis, and at a younger age ( 7, 9-11). Other studies have
identified disproportionate survival differences by race,
despite equal treatment ( 10, 12-15). Some authors have
suggested that these differences may reflect variations in
tumor biology and genetics by race ( 7, 8, 16). Additional
causes of CRC disparities by race are thought to be multifactorial and include differences in socioeconomic status ( 8,
9), rates of obesity ( 17), screening rates ( 18), and health care
utilization ( 19), as well as a trend towards more right-sided
(proximal) tumors among African Americans ( 13, 20-24). The purpose of this study is to present trends in African
American/white disparities in CRC incidence and mortality
in Wisconsin. Monitoring trends in cancer incidence and
mortality is an important part of any coordinated state
plan to reduce disparities, providing critical information
to cancer prevention programs, clinicians, and policy
makers who seek to reduce the burden of cancer. While
there is evidence of trends in African American/white CRC
disparities at the national level, there are no such trend
data for Wisconsin, as previously published reports ( 25-28)
have combined several years of data in order to present data
for multiple ethnic groups. By filling these gaps, the paper
provides an example of state-level surveillance required for
CRC control.
|
|
Methods
Data sources
We obtained incidence data from the Wisconsin Cancer
Reporting System (WCRS) for the period 1995 to 2006,
the most recent year for which data were available. As
required by state law, cancer cases are reported to WCRS
by Wisconsin hospitals, clinics, and physician offices. All
invasive and noninvasive malignant tumors, except basal
and squamous cell carcinomas of the skin and in situ cancers
of the cervix uteri, are reportable to WCRS. Incidence rates
were age-adjusted using the 2000 US standard population
and calculated using NCI’s SEER*Stat software.
Mortality data used in this study reflect Wisconsin
resident death records from the Vital Records Section,
Wisconsin Department of Health Services. We accessed
mortality data from the National Center for Health
Statistics (NCHS) public use data file of Wisconsin deaths
covering the period 1995 to 2006. Population data used in
calculating cancer rates are obtained periodically by NCHS
from the Census Bureau; those used in this study were ageadjusted
to the 2000 US standard population. We used
SEER*Stat software to calculate mortality rates. We also
applied race categories used by NCHS (“White” and “Black
or African American”) ( 29). Stage of diagnosis was obtained from WCRS, which
codes cases based on SEER staging guidelines. Precise
American Joint Committee on Cancer TNM staging ( 30) is
not currently available from WCRS; cancers are described
as “localized” (invasive tumor that is confined to the organ
of origin), “regional” (tumor spread beyond the organ of
origin to adjacent organs or tissue by direct extension, or through the regional lymph nodes, or both, but appears
to have spread no further) or “distant” (tumor has spread
to parts of the body remove from the primary organ, or a
systemic malignancy) ( 28). Some cases are unstaged, due
to insufficient information. The stage data are not ageadjusted.
Analysis
The observed annual incidence and mortality rates were
plotted over the period 1995 to 2006 for all Wisconsin
residents, by race and gender. (Due to data variability
resulting from small populations, averages over three
years are presented in the figures below.) Using slopes and
intercepts derived from ordinary least squares regressions,
trend lines of the incidence and mortality data were then
plotted. The ratio of the African American rate to the
white rate (rate ratio) in 1995 and 2006, based on the
1995-2006 trend line, was calculated. This ratio constitutes
the measure of relative disparity ( 31), and was compared
between the beginning and the end of the period. Due to limited number of African American cases
in some years, we combined stage data in three-year
increments: 1995-1997, 1998-2000, 2001-2003, and
2004-2006. Due to the small number of distant cases among
African Americans (fewer than 30 per year in the state),
only localized and regional disease were analyzed.
|
|
Results
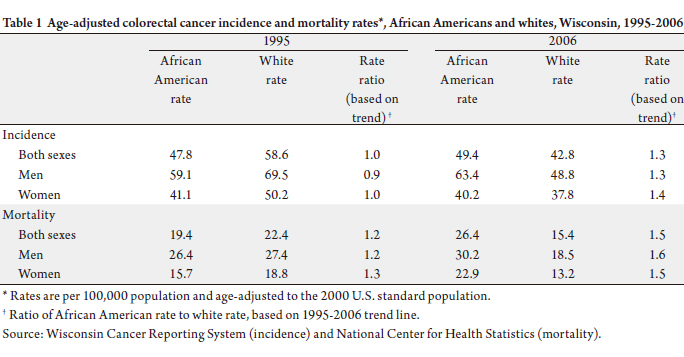
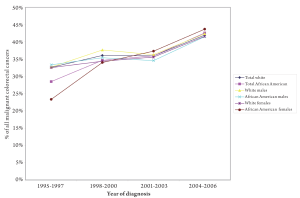
Stage at diagnosis
Among white and African American men and women of
both races, the percentage of malignant CRC cases which
were localized at diagnosis increased over the period
1995-2006, with the percentage for all groups reaching
nearly 40% in 2004-2006 (Figure 1). In contrast, the
percentage of cases which involved regional tumors at
diagnosis decreased for all groups, falling to approximately
30% of all cases in 2004-2006 (Figure 2). There were 20
or fewer cases of distant disease annually among African
Americans in Wisconsin (45 in 1995-1997, 52 in 1998-2000,
61 in 2001-2003, and 81 in 2004-2006). Due to the small
number of distant cases over these periods, it is difficult to
draw conclusions about the trends in these advanced cases
relative to earlier staged CRC among African Americans,
however, the number of distant cases increased over time.
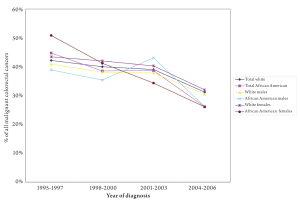
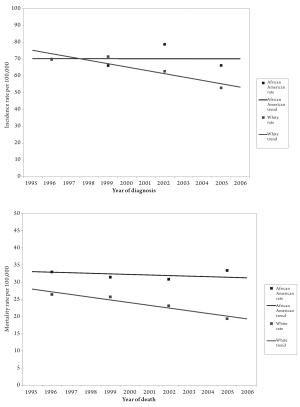
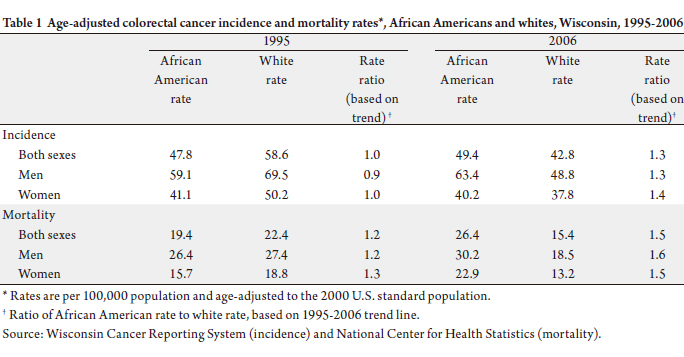
Mortality and incidence, both sexes combined
Incidence: During 1995-2006, CRC was diagnosed in
36,877 Wisconsin residents, including 35,108 whites and
1,192 African Americans. Age-adjusted CRC incidence
decreased 26% from 59 per 100,000 in 1995 to 44 per 100,000 in 2006. Incidence decreased quite dramatically
for whites over the period, but not for African Americans.
Moreover, an absolute disparity in rates persisted, with
African American rates higher than white rates over
virtually the entire period (Figure 3). Relative disparity,
measured using the rat io of the Af r ican Amer ican
incidence rate to the white incidence rate based on the
1995-2006 trend line, grew from 1.0 in 1995 and 1.3 in
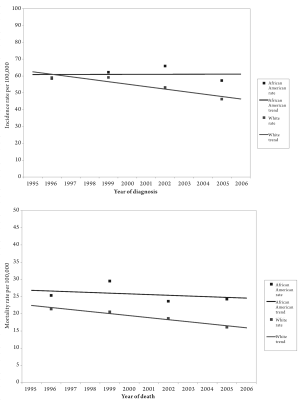
2006 (Table 1).
Mortality: From 1995-2006, there were 13,207 deaths
due to CRC among Wisconsin residents, including 12,645
whites and 450 African Americans. Age-adjusted CRC
mortality declined 29% from 22 per 100,000 in 1995 to 16
per 100,000 in 2006. Mortality decreased markedly over the period among whites, but not for African Americans,
and an absolute disparity in rates persisted over the period
(Figure 3). The relative disparity in death rates grew over
the period, with the rate ratio increasing from 1.2 in 1995 to
1.5 in 2006 (Table 1).
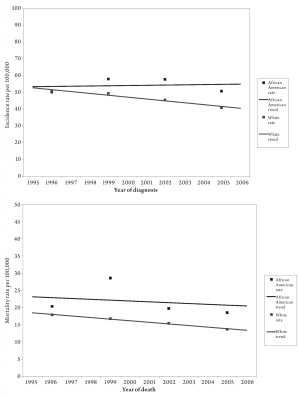
Mortality and incidence, males
Incidence: During 1995-2006, CRC was diagnosed in
18,645 Wisconsin men (including 17,746 whites and 585
African Americans). Over this period, age-adjusted CRC
incidence among men decreased 29% from 70 per 100,000
in 1995 to 50 per 100,000 in 2006. Incidence among
African Americans was higher than that of whites over most
of the period. In addition, while white rates fell, rates for African Americans remained stable (Figure 4). The relative
disparity in male incidence rates grew from a rate ratio of 0.9
in 1995 to 1.3 in 2006 (Table 1).
Mortality: Between 1995 and 2006, there were 6,594
deaths due to CRC among Wisconsin men (including 6,309
whites and 224 African Americans). Over this period, ageadjusted
male CRC mortality decreased 31% from 27.4
per 100,000 in 1995 to 19.0 per 100,000 in 2006. CRC
mortality among African American men was consistently
higher than that among white men. Over the period,
the disparity in CRC mortality rates between African
Americans and white men increased due to the sharper
decline in white rates compared to African American rates
(Figure 4). The ratio between African American and white
CRC mortality rates increased from 1.2 in 1995 to 1.6 in
2006 (Table 1).
Mortality and incidence, females
Incidence: From 1995-2006, CRC was diagnosed in
18,232 Wisconsin women (including 17,362 whites and
607 African Americans). During this period, age-adjusted
CRC incidence among women decreased 24% from 51 per
100,000 in 1995 to 38 per 100,000 in 2006. Over this time
frame, the incidence among African American women was
more than that of white women in nearly every year (Figure
5). The relative disparity in female CRC incidence also
increased as African American rates increased and white
rates decreased. The ratio between African American and
white rates was 1.0 in 1995 and 1.4 in 2006 (Table 1).
Mortality: Between 1995 and 2006, there were 6,613
deaths due to CRC among Wisconsin women (including
6,336 whites and 226 African Americans). During this
period, age-adjusted CRC mortality decreased 28% from 19
per 100,000 in 1995 to 14 per 100,000 in 2006. In this time frame, the disparity in female CRC mortality rates between
African Americans and whites persisted (Figure 5), and the
ratio between African American and white CRC mortality
rates increased from 1.3 in 1995 to 1.5 in 2006 (Table 1).
|
|
Discussion
The results indicate that disparities in CRC incidence
and mortality between African Americans and whites in
Wisconsin are large and have increased over the last decade.
These results are similar in trajectory to those observed at
the national level over the same period, although the scale
of change in Wisconsin was much larger. For the U.S. as
a whole, CRC mortality rates decreased for both whites
and African Americans from 1999 to 2006, but the rate
ratio increased from 1.4 to 1.5. National CRC incidence
rates have also decreased, but the relative disparity has remained stable at 1.2 ( 32). The state-level data are critical
to understanding where Wisconsin is in its effort to
reduce the burden of CRC, and to informing research and
interventions for CRC prevention and control. The reasons for the alarming increase in disparities in
CRC mortality and incidence between African Americans
and whites in Wisconsin are unknown, but may be due to
changes in risk factors in these two populations, such as
obesity. Results from the Wisconsin Behavioral Risk Factor
Survey reveal that between 2000 and 2009, overweight/obesity rates among African Americans increased 26%
(from 64% to 86%). Overweight/obesity rates also
increased among whites, but the increase was much smaller
(11%, from 58% to 65%) ( 33). Low socioeconomic status has been shown to be
associated with an increase in the incidence of and poorer
survival from CRC ( 34, 35). The fact that in Wisconsin,
African Americans are more likely to live in poverty and
less likely to have graduated from high school than whites
( 36) may explain some of the observed CRC disparities.
Cancer disparities have also been explained by differential
access to screening, diagnosis, and treatment ( 2). African
American residents of Wisconsin are twice as likely to be
uninsured as whites ( 36). It is thus possible that African
Americans are less likely to receive appropriate CRC
screening ( 18, 19), appropriate, timely treatment for CRC
( 15, 37-40), or services known to prevent CRC ( 41, 42). The
staging distribution presented here shows that there have
been increasing numbers of limited stage CRC diagnosed
amongst African Americans, suggesting a possible screening
effect. Finally, health care access has also improved for
African Americans. In 1996-2000, the uninsurance rate
among African Americans was 17% ( 47), compared to 13%
in 2001-2005 ( 46). A number of limitations should be considered when
interpreting the results of this study. First, the scope is
limited to differences in CRC incidence and mortality
rates between African American and whites. The decision
to focus on these two groups was determined by the
demographic composition of Wisconsin and the rarity of
cancer events. Wisconsin has relatively small non-white
populations, making the comparisons in the present study
difficult to replicate between other racial or ethnic groups
in the state. Cancer incidence and mortality rates among
many minority populations vary widely from year to year.
However, this variation is likely due to the small size of
the population groups rather than real changes in disease
burden. The African American population in Wisconsin
has been stable in numbers for some time in Wisconsin, and
is concentrated in larger urban areas, chiefly Milwaukee.
This is in contrast to southern United States where African Americans are distributed in rural and urban areas and not
heavily concentrated. Thus, in Wisconsin migration is not
a large issue for the African American population in such a
way to make raise concern about selection bias.
Second, WCRS, as a central state cancer registry
participating in the National Program of Cancer Registries,
maintains a passive system of data collection and therefore,
the various reporting facilities are largely responsible for the
quality and timeliness of the data submissions to WCRS.
Reporting variability may impact the relatively small annual
numbers reported in this analysis. WCRS has made data
collection improvements and suggestions in determining
the race and ethnicity of cancer cases (the numerator for
incidence rates). However, it is likely that an unknown
degree of misclassification or under-reporting of race still
exists. There are no national standards for collecting race
data, and facilities vary in the methods used for collecting
racial and ethnic data. Especially when the number of
cases is relatively small, the quality of data collection and
reporting can greatly impact annual incidence numbers
and rates. Cancer registry stage is also reported in a format
different from the American Joint Commission on Cancer
TNM staging that clinicians use in practice, so one cannot
compare the two directly. The WCRS does not report data
on geographic location, age distribution or socioeconomic
status. Additionally, the treatment data collected in the
WCRS is not reliably validated and so is not reported.
In summary, disparities in CRC incidence and mortality
between African Americans and whites in Wisconsin are
large and have worsened over the period 1995 to 2006.
Statewide action to reduce CRC disparities must start with
this evidence. First, African Americans may fall into a
higher risk group warranting earlier initiation of colorectal
screening than the currently recommended starting age
for all average risk adults. There is also promise in efforts
to reduce exposure to risk factors and improve access
to appropriate screening, treatment, and prevention ( 2)
among all Wisconsin residents, and in particular among
African Americans. Patient navigation is one such tool
( 43-45). Care must be taken that any plan carefully balance
resources and set appropriate priorities to target inequities
in CRC burden.
|
|
Conflict of interest/study support
Guarantor of the article: Noelle LoConte, MD.
Specific author contributions: All authors participated
in the design and analysis of the study and in the writing of
the paper. Nathan Jones and Amy Williamson conducted
the data analyses.
Financial support: This project was supported by grant P30 CA014520 from the National Cancer Institute and
by grant T32HS000083 from the Agency for Healthcare
Research and Quality National Research Award (J.W.).
Potential competing interests: None.
|
|
Acknowledgements
The authors would like to acknowledge Mary Foote of the
Wisconsin Cancer Registry for assisting with data access
and interpretation.
|
|
References
- National Cancer Institute [Internet]. Center to Reduce Cancer Health
Disparities. Health disparities defined [updated 2010 Aug 25; cited
2010 Jun 16]. Available from: http://crchd.cancer.gov/disparities/defined.html.[LinkOut]
- American Cancer Society. Cancer Facts & Figures 2010. Atlanta:
American Cancer Society; 2010.
- Centers for Disease Control and Prevention[Internet]. National
Comprehensive Cancer Control Program.[updated 2011 March 16;
cited 2010 June 7] Available from: http://www.cdc.gov/cancer/ncccp/.[LinkOut]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ. Cancer Statistics,
2009. CA Cancer J Clin 2009;59:225-49.[LinkOut]
- Rex DK, Johnson DA, Anderson JC, Schoenfeld PS, Burke CA,
Inadomi JM, et al. American College of Gastroenterology guidelines
for colorectal cancer screening 2009 [corrected]. Am J Gastroenterol
2009;104:739-50.[LinkOut]
- Edwards BK, Ward E, Kohler BA, Eheman C, Zauber AG, Anderson RN,
et al. Annual report to the nation on the status of cancer, 1975-2006,
featuring colorectal cancer trends and impact of interventions (risk
factors, screening, and treatment) to reduce future rates. Cancer
2010;116:544-73.[LinkOut]
- Polite BN, Dignam JJ, Olopade OI. Colorectal cancer and race:
understanding the differences in outcomes between African Americans
and whites. Med Clin N Am 2005;89:771-93.[LinkOut]
- Polite BN, Dignam JJ, Olopade OI. Colorectal cancer model of
health disparities: understanding mortality differences in minority
populations. J Clin Oncol 2006;24:2179-87.[LinkOut]
- Marcella S, Miller JE. Racial differences in colorectal cancer mortality.
The importance of stage and socioeconomic status. J Clin Epidemiol
2001;54:359-66.[LinkOut]
- Mayberry RM, Coates RJ, Hill HA, Click LA, Chen VW, Austin DF, et
al. Determinants of black/white differences in colon cancer survival. J
Natl Cancer Inst 1995;87:1686-93.[LinkOut]
- Jessup JM, McGinnis LS, Steele GD Jr, Menck HR, Winchester DP.
The National Cancer Data Base. Report on colon cancer. Cancer
1996;78:918-26.[LinkOut]
- Alexander D, Jhala N, Chatla C, Steinhauer J, Funkhouser E, Coffey
CS, et al. High-grade tumor differentiation is an indicator of poor
prognosis in African Americans with colonic adenocarcinomas. Cancer 2005;103:2163-70.[LinkOut]
- Alexander D, Chatla C, Funkhouser E, Meleth S, Grizzle WE, Manne
U. Postsurgical disparity in survival between African Americans and
Caucasians with colonic adenocarcinoma. Cancer 2004;101:66-76.[LinkOut]
- Dayal H, Polissar L, Yang CY, Dahlberg S. Race, socioeconomic status,
and other prognostic factors for survival from colo-rectal cancer. J
Chronic Dis 1987;40:857-64.[LinkOut]
- Potosky AL, Harlan LC, Kaplan RS, Johnson KA, Lynch CF. Age,
sex, and racial differences in the use of standard adjuvant therapy for
colorectal cancer. J Clin Oncol 2002;20:1192-202.[LinkOut]
- Katkoori VR, Jia X, Shanmugam C, Wan W, Meleth S, Bumpers H, et al.
Prognostic significance of p53 codon 72 polymorphism differs with race
in colorectal adenocarcinoma. Clin Cancer Res 2009;15:2406-16.[LinkOut]
- Dignam JJ, Polite BN, Yothers G, Raich P, Colangelo L, O’Connell MJ,
et al. Body mass index and outcomes in patients who receive adjuvant
chemotherapy for colon cancer. JNCI 2006;98:1647-54.[LinkOut]
- Swan J, Breen N, Coates RJ, Rimer BK, Lee NC. Progress in cancer
screening practices in the United States: results from the 2000 National
Health Interview Survey. Cancer 2003;97:1528-40.[LinkOut]
- Laiyemo AO, Doubeni C, Pinsky PF, Doria-Rose VP, Bresalier R,
Lamerato LE, et al. Race and colorectal cancer disparities: healthcare
utilization vs different cancer susceptibilities. J Natl Cancer Inst
2010;102:538-46.[LinkOut]
- Cheng X, Chen VW, Steele B, Ruiz B, Fulton J, Liu L, et al. Subsitespecific
incidence rate and stage of disease in colorectal cancer by
race, gender, and age group in the United States, 1992-1997. Cancer
2001;92:2547-54.[LinkOut]
- Rabeneck L, Davila JA, El-Serag HB. Is there a true “shift” to the
right colon in the incidence of colorectal cancer? Am J Gastroenterol
2003;98:1400-9.[LinkOut]
- Dominitz JA, Samsa GP, Landsman P, Provenzale D. Race, treatment,
and survival among colorectal carcinoma patients in an equal-access
medical system. Cancer 1998;82:2312-20.[LinkOut]
- Dignam JJ, Colangelo L, Tian W, Jones J, Smith R, Wickerham DL, et al.
Outcomes among African-Americans and Caucasians in colon cancer
adjuvant therapy trials: findings from the National Surgical Adjuvant
Breast and Bowel Project. J Natl Cancer Inst 1999;91:1933-40.[LinkOut]
- Nelson RL, Persky V, Turyk M. Determination of factors responsible
for the declining incidence of colorectal cancer. Dis Colon Rectum
1999;42:741-52.[LinkOut]
- American Cancer Society. Wisconsin Cancer Facts & Figures 2007.
Atlanta, GA: American Cancer Society; 2007.
- Wisconsin Department of Health and Family Services. The Health
of Racial and Ethnic Populations in Wisconsin. In:Minority Health
Program.The Health of Racial and Ethnic Populations in Wisconsin
1996–2000. Madison, Wisconsin: Wisconsin Department of Health
and Family Services, Division of Public Health; 2004. 22-6.
- Wisconsin Department of Health Ser vices[Internet]. Wisconsin
Minority Health Program. Updated tables for the Wisconsin Minority
Health Report (January 2007)[updated 2010 July 12;cited 2010 June
30. Available from: http://dhs.wisconsin.gov/wcrs/pubs.htm.[LinkOut]
- Wisconsin Department of Health and Family Services. Wisconsin
Cancer Incidence and Mortality. Madison, Wisconsin: Wisconsin
Department of Health and Family Services, Division of Public Health,
Bureau of Health Information and Policy; 2007.
- Surveillance Epidemiology and End Results (SEER) Program, National
Cancer Institute[Internet]. Race recode changes[cited 2010 June
30]. Available from: http://seer.cancer.gov/seerstat/variables/seer/yr1973_2005/race_ethnicity/.[LinkOut]
- O’Connell JB, Maggard MA, Ko CY. Colon cancer survival rates with
the new American Joint Committee on Cancer sixth edition staging. J
Natl Cancer Inst 2004;96:1420-5.[LinkOut]
- Carter-Pokras O, Baquet C. What is a “health disparity”? Public Health
Rep 2002;117:426-34.[LinkOut]
- Centers for Disease Control and Prevention, National Center for Health
Statistics[Internet]. Compressed Mortality File 1999-2007[cited 2010
June 25]. Available from: http://wonder.cdc.gov/cmf-icd10.html.[LinkOut]
- Office of Health Informatics[Internet]. Wisconsin Interactive Statistics
on Health (WISH) data query system, BRFS Module[updated 2011
March 9;cited 2011 March 8]. Available from: http://dhs.wisconsin.gov/wish/.[LinkOut]
- Siegel RL, Jemal A, Thun MJ, Hao Y, Ward EM. Trends in the incidence
of colorectal cancer in relation to county-level poverty among blacks
and whites. J Natl Med Assoc 2008;100:1441-4.[LinkOut]
- Kinsey T, Jemal A, Liff J, Ward E, Thun M. Secular trends in mortality
from common cancers in the United States by educational attainment,
1993-2001. J Natl Cancer Inst 2008;100:1003-12.[LinkOut]
- Wisconsin Department of Health and Family Services. Wisconsin
Minority Health Report, 2001-2005. Madison, Wisconsin: Wisconsin
Department of Health and Family Services, Division of Public Health,
Bureau of Health Information and Policy; 2008.
- Schrag D, Rifas-Shiman S, Saltz L, Bach PB, Begg CB. Adjuvant
chemotherapy use for Medicare beneficiaries with stage II colon cancer.
J Clin Oncol 2002;20:3999- 4005.[LinkOut]
- Demissie K, Oluwole OO, Balasubramanian BA, Osinubi OO, August
D, Rhoads GG. Racial differences in the treatment of colorectal cancer:
a comparison of surgical and radiation therapy between Whites and
Blacks. Ann Epidemiol 2004;14:215-21.[LinkOut]
- Baldwin LM, Dobie SA, Billingsley K, Cai Y, Wright GE, Dominitz JA,
et al. Explaining black-white differences in receipt of recommended
colon cancer treatment. J Natl Cancer Inst 2005;97:1211-20.[LinkOut]
- Ayanian JZ, Zaslavsky AM, Fuchs CS, Guadagnoli E, Creech CM,
Cress RD, et al. Use of adjuvant chemotherapy and radiation therapy
for colorectal cancer in a population-based cohort. J Clin Oncol
2003;21:1293-300.[LinkOut]
- Chlebowski RT, Wactawski-Wende J, Ritenbaugh C, Hubbell FA,
Ascensao J, Rodabough RJ, et al. Estrogen plus progestin and colorectal
cancer in postmenopausal women. N Engl J Med 2004;350:991-1004.[LinkOut]
- Robertson DJ, Greenberg ER, Beach M, Sandler RS, Ahnen D, Haile
RW, et al. Colorectal cancer in patients under close colonoscopic
surveillance. Gastroenterology 2005;129:34-41.[LinkOut]
- Myers RE, Hyslop T, Sifri R, Bittner-Fagan H, Katurakes NC, Cocroft J, et al. Tailored navigation in colorectal cancer screening. Med Care
2008;46:S123-31.[LinkOut]
- Christie J, Itzkowitz S, Lihau-Nkanza I, Castillo A, Redd W, Jandorf
L. A randomized controlled trial using patient navigation to increase
colonoscopy screening among low-income minorities. J Natl Med Assoc
2008;100:278-84.[LinkOut]
- Chen LA, Santos S, Jandorf L, Christie J, Castillo A, Winkel G, et al. A
program to enhance completion of screening colonoscopy among urban
minorities. Clin Gastroenterol Hepatol 2008;6:443-50.[LinkOut]
- Wisconsin Department of Health and Family Services. The Health of Racial and Ethnic Populations in Wisconsin. In:Minority Health
Program.The Health of Racial and Ethnic Populations in Wisconsin
1996–2000. Madison, Wisconsin: Wisconsin Department of Health
and Family Services, Division of Public Health; 2004. 22-6.
- Wisconsin Department of Health and Family Services. Wisconsin
Minority Health Report, 2001-2005. Madison, Wisconsin: Wisconsin
Department of Health and Family Services, Division of Public Health,
Bureau of Health Information and Policy; 2008.
Cite this article as:
LoConte N, Williamson A, Gayle A, Weiss J, Leal T, Cetnar J, Mohammed T, Tevaarwerk A, Jones N. Increasing disparity in colorectal cancer incidence and mortality among African Americans and whites: A state’s experience. J Gastrointest Oncol. 2011;2(2):85-92. DOI:10.3978/j.issn.2078-6891.2011.014
|