Viral hepatitis and hepatocellular carcinoma: etiology and management
Hepatitis B virus (HBV) risk and hepatocellular carcinoma (HCC)
Epidemiology
It is estimated that over 50% of HCC cases worldwide are related to chronic HBV (1,2). Since the implementation of worldwide HBV vaccination there has been an overall decline in the burden of HBV, yet the HBV burden remains quite high in various parts of the world. There are approximately 350–400 million people across the world infected with HBV, the majority reside in or originate from Asia. Each year HBV accounts for 749,000 new cases of HCC and 692,000 HCC-related deaths (3). The annual incidence of HCC is estimated to be <1% for non-cirrhotic HBV infected patients and 2–3% for those with cirrhosis. Because of worldwide and geographic variations in HBV incidence, the burden of HBV related HCC also varies. Asian-Pacific and sub-Saharan Africa represent the highest incidence of HCC worldwide. Much lower risk of HBV associated HCC is seen in the United States with less than 20% incidence. Due to its diversity, Europe has different areas: low risk (18%) in West and North and high risk (51%) East and South (4). Occult HBV or subclinical infection as defined by detectable HBV DNA in the liver but hepatitis B surface antigen (HBsAg) seronegativity is now recognized as increased risk for HCC. The risk is most notable in those over the age of 50 (5,6). Recently published data reveal that in China, the age-standardized death due to HBV-related HCC and cirrhosis in 2013 was 10.95 and 4.91 per 100,000 people (7). Fifty-five percent of all HCC cases worldwide are reported from China (8).
In 1991, the WHO recommended the integration of the HBV vaccine into national immunization programs in countries with an HBV carrier prevalence of 8% or higher by 1995 and in all other countries by 1997 (9). The universal infant vaccination rate in sub-Saharan Africa was initially quite low at 5% in 2000 but increased to 72% by 2012. Parts of the Pacific region had the lowest immunization rates, but by 2012 had increased to the highest rates at 91%. Taiwan has an exceptionally higher rate of HCC in HBV infected children. Thirteen years after the introduction of universal infant vaccination, the annual incidence of HCC dropped in several groups of children: per 100,000 decline from 0.7 to 0.36 in children ages 6–14; decline 0.52 to 0.13 in ages 6–9 (10,11). The introduction of universal HBV vaccination in the 1980s for newborns has begun to modify the natural history of HCC. Studies from Taiwan, which introduced vaccination and post-exposure prophylaxis with HBV immunoglobulin in 1984 for high-risk patients [surface antigen positive (HBsAg) and HBV e antigen (HBeAg) positive mothers], have demonstrated a 65–75% reduction in the incidence of HCC in children aged 6–14 years. However, the current preventive strategy does not address older adult HBV patients, most of whom were infected at birth prior to the availability of the HBV vaccine.
Risk factors
The risk of HCC in those infected by HBV is influenced by virus-related, host-related, dietary and lifestyle factors. Of note in HBV-related HCC, cirrhosis is absent in up to one-third of patients. This is in contrast to other etiologies of liver disease, whereby cirrhosis is the background liver histology in the vast majority (80%) (11,12). Older age and male gender are well established factors that carry higher risk of HCC. Perhaps this gender difference is driven by the protective effects of estrogen interacting with the hepatocyte nuclear factor 4 α (13) and IL-6 signaling (12). Coinfection with other liver specific viruses has been noted to increase HCC risk: chronic hepatitis C virus (HCV) and human immunodeficiency virus (HIV). Hepatitis D virus (HDV) or hepatitis delta is a virus that only exists in the setting of HBV infection as a co-existing infection because of its reliance on HBV for its propagation. There is heterogeneity as risk of HCC with HDV. Similarly, those infected co-infected with HBV and HDV have a 3-fold higher risk of progressing to cirrhosis more rapidly as compared to HBV monoinfected; the Eurohep cohort also predicts a 3.2-fold increase in HCC risk in those co-infected with HDV-HBV (14). This was replicated in a large US veteran cohort as well (15). While some studies showed the risk of HCC was higher in the absence of cirrhosis, raising the possibility of direct oncogenic activity of HDV (16). Alcohol use is strongly synergistic in raising risk for HCC in those with HBV; it has been noted to double risk of HCC (17). Dietary intake of aflatoxin in Asia and Africa is also known to contribute to a higher risk of HCC in those infected with HBV (18). Tobacco use has also been associated with higher rates of HCC in those with HBV.
Evidence mainly from the Far East has demonstrated that there is a family based susceptibility to HCC. Genetic host factors are known to drive this association, with the identification of single nucleotide polymorphisms (SNPs). SNPs have been identified through genome wide association studies (GWAS): STAT4 (19), TPTE2 (20), CTLA-4 (21) and DCL1 (22) genes, as well as in the region containing the UBEB4, KIF1B and PGD genes (23). Additional SNPs have been described, but it is accepted that these identified SNPs only partially account for the variability in HCC susceptibility. Overall they carry a low risk ratio for HCC development as summarized by Iavarone et al. (24).
HBV viral factors
HBV is considered a carcinogenic virus. Chen et al. demonstrated in the largest study to date that the risk of developing HCC was directly proportional to the HBV DNA level (25). 3,653 HBsAg+ subjects were enrolled. The mean follow up period was 11.4 years. After adjusting for all other confounding variables, it was noted that subjects with persistent elevation of serum HBV DNA had a high HCC risk, most notably HBV DNA 10,000 copies/mL. The integration of HBV DNA into the host genome has been well described. Like other viruses, there is a lack of proof-reading ability by the HBV polymerase therefore leading to genomic variability. Ultimately this leads to selection of HBV quasi-species containing several mutations. HBV virions contain a circular partially double-stranded DNA of nearly 3,200 nucleotides. Soon after entry into the hepatocyte, HBV DNA is converted into a covalently closed circular DNA (HBV cccDNA) where it remains stable in the cell nucleus. The viral proteins HBx and HBc are engaged to regulate its transcription and viral replication. This integration of the HBV DNA into the host genome contributes to viral pathogenesis both by cis-acting mechanism and by the continuous expression of trans-acting wild-type and truncated HBx or truncated preS/S polypeptides bearing enhanced transforming properties (26).
Regarding other viral factors, it was reported in a large Taiwanese cohort with HBV related HCC (HBeAg negative), levels of HBV surface antigen were positively correlated with incidence of HCC in those with lower levels of HBV DNA (27).
HBV genotypes A-H have been identified and characterized. HBV genotype C has been associated with a higher risk of HCC (28). Pressures of selection driven by antiviral therapies, vaccinations and duration of HBV infection are what lead to mutations. These mutations are found in a region known as the basal core promoter (BCP)/preCore region and the preS/S region. While data from Asia suggests an increased risk of cirrhosis and HCC from genotype C, other studies have found genotype B to predispose to HCC among children and well as in non-cirrhotic patients (29,30). A high viral load and HBeAg seropositivity also confer increased HCC risk. HBeAg seropositivity, a marker of active viral replication was an independent predictor of HCC in a group of 11,893 Taiwanese patients followed for 10 years (31). The REVEAL-HBV study followed 3,653 Taiwanese patients with HBV and found a proportional increase in risk of cirrhosis and HCC with increased viral load even after adjusting for covariates such as sex, age, smoking, and alcohol use (32). There is a significantly higher risk of HCC with the emergence of the double mutation T1762/A1764 in HBV genotypes B and C (33,34).
The exact oncogenic mechanism of HBV remains a mystery, but certain subsequent events have been characterized: intracellular DNA rearrangement and enhanced mutagenesis; active cell inflammation and proliferation. Following HBV DNA integration into host genome, insertional mutagenesis of cancer related genes and chromosomal instability occur. Persistent hepatocyte inflammation leads to premalignant and malignant characteristics that are associated with oxidative stress, which subsequently incites repeated cycle of apoptosis, necrosis and compensatory regeneration. It has been postulated that HCC develops from ineffective regulation of liver cell senescence, which regulates tumor immune surveillance. Senescence surveillance of pre-malignant hepatocytes is an important step against the development of tumors. Hepatic fibrosis, which is stimulated by hepatic stellate cell activation is another factor that encourages development of HCC, as high-grade dysplastic nodules in fibrotic livers are immediate precursors to HCC (35,36). Additionally, chromosomal aberration and epigenetic modifications such as DNA methylation leading to silencing of tumor suppressor genes have been described in cirrhosis (37,38).
The HBx regulatory protein has been shown to interfere with normal control of cell cycle progression, through its ability to bind different cellular partners and to activate transcription as well as various signaling cascades (39). HBV integration frequently involves the HBx which frequently undergoes deletion at the 3' end, causing expression of C-terminal-truncated HBV protein able to enhance HCC cell invasiveness and metastasis (40). HBx aids in overcoming senescence, a process by which proliferation of damaged cells is limited and risk of malignancy is reduced by triggering expression of tumor suppressors. Several mechanisms have been described by which this occurs: (I) inhibiting the P53 nucleotide excision repair and transcription-coupled repair function; (II) decreasing the expression of the P53 activators ASPP1 and ASPP2; (III) suppressing the cyclin-dependent kinase (CDK) inhibitors INK4A and P21 via promoter methylation that results in inactivation of the RB tumor suppressor (40).
HCC screening in HBV
The majority (70–90%) of patients with HBV who develop HCC have underlying cirrhosis, with the annual incidence of HCC is approximately 2.5% (11), Thus, any patient with HBV related cirrhosis should undergo screening biannually. Importantly however, HCC can develop in HBV patients without cirrhosis. The threshold for screening HBV patients without cirrhosis, which considers the cost effective of screening relative to life years gained by screening, occurs when the annual incidence of HCC is ≥0.2%. Beasley et al. found that Asian men, regardless of their replicative status, begin to meet this threshold at age 40, while the equivalent risk in Asian women occurs at age 50 (41,42). Studies suggest that African/North American Black patients are a population at risk at particularly young age as well (see Table 1). Caucasian patients who lose surface antigen, in contrast to Asian patients, have a reduced risk of HCC. Other specific patients with HBV who are at increased risk of HCC include patients co-infected with HIV with a family history of HCC.
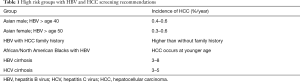
Full table
Population based studies have also identified specific HBV viral factors predictive of HCC development. The consensus is that HBV patients with active viral replication as denoted by high HBV DNA, HBeAg positivity, and active inflammation [elevated alanine aminotransferase (ALT)] should clearly undergo surveillance.
The largest clinical trial to demonstrate a benefit of HCC surveillance with respect to survival was performed in Shanghai, China, in 18,816 patients with current or prior HBV infection. Patients were randomized to screening with liver ultrasound and alpha-fetoprotein (AFP) every 6 months or standard of care. Although adherence to screening was less than 60%, HCC mortality was still reduced by 37% in the screening group vs. the control group (43). Ultrasonography (u/s) is the most commonly employed imaging modality for HCC surveillance and has been shown to have acceptable diagnostic accuracy for HCC detection with a sensitivity of 65–80% and specificity greater than 90%. Consensus guidelines from the American Association for the Study of Liver Diseases (AASLD) (44) and the European Association for the Study of Liver Diseases (EASL) (45) recommend 6-month interval screening with ultrasonography, as the cost-effective modality for screening purposes. Multi-phase computed tomography (CT) or magnetic resonance imaging (MRI) have higher diagnostic accuracy for HCC detection and should be performed when ultrasound results are suboptimal or abnormal. Screening with serological testing for AFP is not currently recommended due to poor sensitivity and specificity by the AASLD & EASL, whereas the National Comprehensive Cancer Network (NCCN) suggests that AFP may have utility when combined with ultrasound for at-risk individuals (46). In fact, newer data suggests that the addition of AFP to u/s may enhance the sensitivity of screening in patients with cirrhosis (47). However, the data are less robust in viral induced cirrhosis compared to non-viral induced cirrhosis (48). With regard to surveillance in HBV infection, every 6-month screening for HCC with AFP testing alone is not adequate. Chen et al. compared this screening strategy in 5,581 male HBsAg+ patients and found no difference in overall survival at 5 years compared to a control population undergoing standard of care (49).
Carcinogenic properties of HCV
HCV may have a direct or indirect role in carcinogenesis, mainly through fibrosis. Patients with advanced fibrosis or cirrhosis are at increased risk for carcinogenesis because chromosomal alterations that occur in fibrotic tissue are associated with tumor formation (1,50). In cirrhotic hepatocytes telomere shortening may lead to chromosome uncapping which induces DNA damage and chromosomal fusion (1). Cells with fused chromosomes that enter the cell cycle may develop translocations and chromosomal instability that may lead to carcinogenesis.
HCV may promote carcinogenesis through chronic inflammation or stimulation of hepatic stellate cells with subsequent fibrosis. Chronic liver inflammation has been associated with a shift in signaling from tumor growth factor beta resulting in a change from tumor suppression to fibrosis and carcinogenesis (51). Proliferative changes in hepatic tissue related to ongoing inflammation from hepatitis are associated with repeated cycles of cell death and regeneration (50). Repeated cell cycles are associated with accumulation of mutations that may transform hepatocytes to malignant cells through a multistage process. However, chronic inflammation by itself does not seem to promote carcinogenesis because patients with autoimmune liver disease who have persistent chronic liver inflammation from autoimmune liver disease rarely develop HCC. HCV nonstructural protein genes promote fibrosis partly through inducing transforming growth factor beta and activating hepatic stellate cells (52). This has been demonstrated in cell culture systems when sera from HCV patients stimulate hepatic stellate cell proliferation, which subsequently leads to fibrosis (52). HCV core protein may promote carcinogenesis. In a transgenic mouse model HCV core protein led to the development of HCC without the genetic aberrations typically seen in carcinogenesis, such as in colon cancer (53).
HCV genotype 3 is independently associated with a higher risk of HCC. Nkontchou et al. first described this when comparing HCV subjects and specifically examined differences in HCC incidence amongst various HCV genotypes (54). In multivariate analysis, genotype 3 infection conferred an increased risk of HCC [hazard ratio (HR) 3.54; 95% confidence interval (CI), 1.84–6.81], even after the adjustment was made for alcohol abuse. This was seen again in a large cohort of patients from a United States Veterans Affairs medical system. Of 110,484 patients with HCV viremia, 8,337 (7.5%) were infected with genotype 3. After adjusting for age, diabetes, body mass index or antiviral therapy, HCV genotype patients had a higher risk of developing cirrhosis (unadjusted HR, HR =1.40; 95% CI =1.32–1.50) and HCC (unadjusted HR =1.66; 95% CI =1.48–1.85). Increased hepatic steatosis is seen uniquely in genotype 3 patients because of direct viral effects, and is independent of coexisting obesity, diabetes and alcohol use (55,56). It is postulated that the steatosis may play a role in accelerating fibrosis and/or have a direct oncogenic effect.
Viral hepatitis treatment considerations with HCC
Treatment of viral hepatitis will be discussed here in the setting of HCC; as other contributors will be focusing on treatment of HCC in respective manuscripts.
HBV
Fortunately, antiviral therapy, which can help prevent the development of cirrhosis and HCC, is now the standard of care for patients with chronic active HBV infection. A preponderance of data now confirms a significant benefit of long-term nucleos(t)ide analogue (NA) therapy in preventing HCC in the setting of chronic HBV infection.
Lamivudine, one of the earliest NA’s, has been shown to improve liver function not only in those without HCC but also in those with HCC (57). Furthermore data suggests it may improve liver function and prevent premature liver related mortality in HBV related HCC patients. In a large study of Asian HBV infected cirrhotic/advanced fibrotic patients that received lamivudine, a smaller percentage of treated patients (3.9%) developed HCC as compared to placebo (7.4%) (58). In addition, it has been observed that a higher percentage of patients experience severe flares of hepatitis in those undergoing chemotherapy or locoregional therapy with higher HBV viral loads (59), therefore suppressing viral replication is of paramount importance. It has been well established that acute HBV flares can lead to hepatic decompensation and death. Surgical resection of HCC is a widely-employed modality used to treat HCC. HBV antiviral therapy is essential in preserving function of the remnant liver. Similarly, as described above, higher pre-operative viral loads are associated with worse overall and recurrence free survivals after curative resection (60).
Regarding individual treatments, NA has been shown to lengthen survival in those HBV infected patients with HCC treated with trans-arterial chemoembolization (TACE) (61). A comparison of 472 entecavir (ETV)-treated patients vs. 1,143 untreated patients, the in the cumulative HCC incidence rates were 3.7% and 13.7% respectively (62).
Most expert society guidelines recommend initiating HBV treatment with advance stage fibrosis. Interferon (IFN) based therapies and now NAs are available for the treatment of HBV. Both agents have been shown to improve tests of liver inflammation, liver function and hepatic fibrosis. Patients with cirrhotic stage hepatic fibrosis are less tolerant of IFN based therapy, therefore NA is recommended in the vast majority of these patients (11).
HCV
The goal of antiviral therapy for chronic HCV is to achieve a sustained virologic response (SVR). The long-term goal is to reduce or eliminate complications from cirrhosis, including ideally HCC. Significant improvements have been made in achieving high rates of sustained (SVR) or virologic cure with the introduction of IFN-free direct acting antiviral therapy. Most of the data on reduction of complications from cirrhosis, including HCC is based on the experience with IFN based therapy.
IFN based therapy was one of the original therapies for HCV. While weighed down by toxicities, IFN has been shown to reduce the recurrence of HCC in numerous cohorts of patients that loco-regional therapy: surgical resection, percutaneous ethanol ablation, and radiofrequency ablation in studies. Achieving SVR with IFN based therapy has been noted to be an independent risk factor for a reduction in the risk of HCC recurrence after any such liver directed therapy. Overall improvement in patient survival was noted in SVR achieving patients as well, owing the improvement in liver histology that is seen with SVR (63). Antiviral therapy has been used (I) to achieve a SVR with the goal of reducing or eliminating complications from chronic liver disease including HCC; (II) as maintenance therapy in patients with bridging fibrosis and cirrhosis; (III) as chemotherapy to treat HCC; (IV) to prevent recurrence after resection or ablative therapies.
With regards to HCV and HCC, a similar paradigm was described by Japanese investigators describing a cohort of patients that underwent surgical resection for HCC (64). Advanced age (≥55 years; HR, 3.1) and advanced liver fibrosis (≥F3; HR, 9.0) still were noted in a multivariate analysis to carry higher HCC risk despite SVR (64). This has been replicated in numerous other studies as summarized by Hiramatsu et al. (65). Diabetes as also emerged as independent risk for development of HCC, so attention needs to be turned to the aggressive treatment of his disease as a separate entity.
IFN has been largely replaced by all oral, IFN-free regimens, where available, which are associated with higher rates of virologic cure and improved side effect profile. However, long term follow up after virologic cure is available for patients treated with IFN-free based regimens is limited due to recent availability. Recent findings will be further discussed later in this manuscript.
Anti-carcinogenic properties of interferon
Antiviral therapy may reduce the risk of HCC through anti-fibrotic effects by reducing inflammation or through antineoplastic properties. Antineoplastic properties of IFNs may be demonstrated through their effects on HCV induced fibrinogenesis and hepatic stellate cells. IFN-alpha with ribavirin decreases HCV stimulated hepatic stellate cell proliferation by 50% (66). IFN may promote fibrinolysis by inhibiting tissue inhibitor of metalloproteinase (an inhibitor of fibrin degradation) or promoting hepatic stellate cell death. In a rat model of carbon tetrachloride induced liver fibrosis, significantly lower levels of tissue inhibitor of metalloproteinase were found in rats treated with pegylated-IFN (PEG-IFN) alpha-2b compared to untreated rats, P<0.05 (67). Hepatic stellate cell apoptosis was higher in the animals administered PEG-IFN compared to the control group (P<0.01). IFN free regimens with direct acting antiviral therapy are not believed to affect stellate cell fibrosis formation, but instead may reduce fibrosis by inhibiting viral replication and thus the inflammatory response that stimulates stellate cell fibrogenesis.
Therapy for HCC has been challenging and sorafenib had been the only chemotherapeutic to demonstrate a survival benefit in the past fifty years. IFN has antineoplastic properties that are partly mediated through inhibition of angiogenesis and promoting tumor cell apoptosis. In mice models of HCC IFN-alpha decreases serum vascular endothelial growth factor and microvessel density which is associated with a significantly lower rate of lung metastases and recurrent HCC after resection, P<0.05 (68). IFN may inhibit tumorogenesis through anti-angiogenesis by downregulating vascular endothelial growth factor. A mouse model of HCC demonstrates that animals administered IFN-alpha 2b had decreased gene expression of vascular endothelial growth factor and cyclooxygenase-2 (69). Apoptosis was greater in the tumor cells of mice treated with IFN compared to controls (P<0.01). Thus, IFN not only inhibited tumor growth through anti-angiogenesis, but also through increased apoptosis in tumor cells. Other studies in tumor cell lines demonstrate the apoptotic effects of IFN alpha and 5-fluorouracil are mediated partly through the Fas/FasL pathway (70).
In summary, animal studies and studies in tumor cell lines demonstrate antineoplastic effects of IFN on HCC through multiple mechanisms. These effects are mediated through inhibiting fibrosis production, hepatic stellate cell activation, inhibition of tumor angiogenesis and promoting tumor apoptosis.
HCC in patients treated with IFN based therapy
The risk of HCC in HCV patients who achieve SVR is markedly reduced, but patients remain at risk for HCC, especially patients who have bridging fibrosis or cirrhosis (71). Although eradication of HCV virus in the serum 12 weeks after therapy is terminated serves as a surrogate to eradicating virus in the liver, studies have shown that HCV RNA persists in the liver and peripheral blood mononuclear cells in some sustained viral responder (72,73). A study in nine sustained viral responders found that peripheral blood mononuclear cells from three of these individuals elicited productive infection in vitro (72). The association of persistent viral RNA in peripheral blood mononuclear cells or in the liver and the risk of HCC is unknown.
Studies demonstrate that the risk of HCC in individuals who achieve virologic cure is reduced compared to non-responders (74-78). In a multicenter retrospective study of 479 HCV patients treated with IFN or PEG-IFN with or without ribavirin, 142 (29.6%) subjects had a sustained response (74). The HR for HCC in sustained responders was 0.46 (95% CI, 0.12–1.70), P=0.25 compared to those who did not have a sustained response. All the patients in the study had bridging fibrosis or cirrhosis and the median follow up was 2.1 years. An analysis of 1,124 HCV patients reported that 3.5% of patients with virologic cure developed HCC after a median follow up of 5.8 years (75). The patients with virologic cure who developed HCC were more likely to be male, older, and have more advanced fibrosis compared to patients with a SVR who did not develop HCC. Three of the 13 patients with virologic cure who developed HCC had mild fibrosis. There was no significant difference in the rate of HCC in the partial response group compared to the non-responders. In an analysis of 1,191 HCV patients treated with IFN and 452 untreated patients estimates of HCC rates after 5 and 10 years of treatment with IFN were 2.1% and 7.6% compared to 4.8% and 12.4% without treatment (76). The risk of HCC was lowest in patients with normal ALT values with or without HCV-RNA clearance, HR =0.32, P=0.012. A meta-analysis of 11 studies involving 2,178 patients found that HCC was 3.7 times more common in non-responders compared to sustained viral responders, Odds ratio =3.7 (95% CI, 1.7–7.8) (71). Even in patients who did not achieve an SVR there seems to be a benefit from IFN because the risk of HCC in untreated patients was 2.7-fold higher. Thus, HCC occurs in HCV infected patients who have achieved virologic cure, but almost all of these patients had bridging fibrosis and cirrhosis. Compared to patients treated with IFN versus those never treated, odds ratio =2.7 (95% CI, 1.9–3.9). Thus, patients with SVR and bridging fibrosis or cirrhosis may warrant ongoing surveillance for HCC, particularly older patients, male patients, and patients with elevated ALT.
Among patients who develop HCC after virologic cure, HCV RNA can be found in hepatic tissue (79). Microscopic pathologic features of HCC are similar between patients who have achieved virologic cure and non-responders. At the molecular level, however, alterations in mitochondrial DNA and methylation status are less frequent in HCC’s from those with virologic cure than HCC’s from patients with chronic HCV (73). The implications of these differences in molecular alterations in HCC’s from those cured and chronic HCV patients are unknown.
HCC and IFN maintenance therapy
Because IFN has anti-fibrotic and anti-carcinogenic properties the use of IFN as maintenance therapy in patients who were non-responders to prior treatment provided the rationale for several clinical trials. In a randomized trial of 53 patients Shiffman et al. found that maintenance IFN therapy with 3 MU three times a week reduced fibrosis stage with a decrease in stage from 2.5 at baseline to 1.7 after 30 months of therapy compared to essentially no change in fibrosis score in the group that stopped IFN (80). The study was not designed to detect significant differences in rates of HCC between the groups. In a clinical trial that included 90 patients randomized to IFN-alpha 6 million units for 12 to 24 weeks or symptomatic treatment (control group), followed for 2 to 7 years, 2 (4%) patients in the IFN group and 17 (38%) patients in the control group developed HCC, P=0.002 (81). Data from these studies provided rationale to consider prescribing IFN maintenance therapy in HCV patients with advanced fibrosis who were non-responders.
The HCV Antiviral Long-Term Treatment against Cirrhosis (HALT-C) trial was designed to determine if long term treatment with PEG-IFN reduces progression of liver disease as indicated by death, HCC, hepatic decompensation or progression to cirrhosis in patients with bridging fibrosis (82). A total of 1,050 patients with bridging fibrosis or cirrhosis who had not had a response to previous therapy with PEG-IFN and ribavirin were randomized to 90 micrograms per week of subcutaneous PEG-IFN alpha-2a or no treatment. More than 90% of patients were genotype 1 and the average age was 50 years old in each group. At 3.5 years after randomization 12 patients in the PEG-IFN group and 15 patients in the control group developed HCC, P=ns. There were no differences in HCC rates when results were stratified by the presence or absence of cirrhosis. A subsequent analysis from HALT-C on the effect of PEG-IFN maintenance therapy on HCC in HCV patients with bridging fibrosis or cirrhosis was conducted in 1,005 patients reported the annual incidence for HCC was 1.1% in the cohort (83). During a median follow up of 4.5 years the cumulative 5-year incidence of HCC for treated patients and controls was 5.4% and 5.0%, respectively, P=0.78. The cumulative 5-year incidence was higher among patients with cirrhosis than with bridging fibrosis, 7.0% and 4.1%, respectively, P=0.08. The rate of HCC in patients without cirrhosis was unexpected. Significant predictors for developing HCC were older age, Black race, esophageal varices, low platelet count, and history of ever smoking.
Smaller studies suggest certain groups of patients may benefit from maintenance therapy. A study of 125 patients 60 years of age and older with chronic HCV treated with IFN alpha 3 million units two to three times a week for a mean of 2.5 years compared rates of HCC to 240 patients treated with herbal medicines (84). The 5-year cumulative rates of HCC in the IFN group and herbal group were 5.9% and 13.7%, respectively. The authors suggest that older patients with advanced fibrosis may benefit from prolonged IFN therapy. It is interesting to note that in individuals with HCV who receive IFN therapy AFP levels decline regardless of virologic response (85). AFP levels may decrease by 57% in patients treated with IFN.
IFN as a chemotherapeutic agent for HCC
IFN-alpha is prescribed as a chemotherapeutic agent for the treatment of malignant melanoma and hematologic malignancies such as hairy cell leukemia. There have been trials of IFN for treating patients with HCC, but many studies have included patients with predominantly HBV (86,87). The largest randomized clinical trial of HCV patients with HCC treated with IFN did not demonstrate a benefit with therapy (88). In this trial 58 patients were randomized to 3 MU of IFN alpha-2b three times a week for one year or symptomatic treatment. Partial tumor response, and tumor progression were not significantly different between the two groups. Overall survival in the IFN group and control group were 58% and 38%, respectively, P=0.19. The study may not have shown significant benefit because the sample size may have been too small as it was powered to detect a 30% improvement in overall survival. Also, patients in this trial had advanced HCC and it may be that IFN may benefit patients with earlier stage disease. IFN therapy was poorly tolerated with 48% of patients discontinuing treatment. Based on these data, IFN cannot be recommended for treatment of HCC outside of a clinical trial.
IFN after liver resection or ablation to prevent or treat recurrent HCC
IFN has been studied as adjuvant therapy after liver resection or ablation of HCC in HCV infected cirrhotics because of its anti-carcinogenic properties (89-95). Among 209 patients with HCV who underwent curative resection for HCC, 70 patients underwent IFN therapy (89). Three-year tumor free survival rates were higher among 40 patients who achieved virologic cure or a biochemical response compared to the untreated group, 71% vs. 46%, P<0.001. Patients with a single tumor derived the most benefit from IFN therapy. In a randomized clinical trial, 150 HCV patients with HCC, of whom 80 were HBV core antibody negative and 70 were core antibody positive, were randomized within 6 weeks after liver resection to IFN administered 3 MU three times a week for 48 weeks or an untreated control group (90). In the overall study group, there were no significant differences in HCC recurrence rates between the treated and control group after liver resection. The subgroup of patients who derived a benefit from post-resection treatment with IFN were those HCV patients who were HBV core antibody negative; the risk of HCC recurrence 2 years or later after resection was reduced by 70%, HR =0.3 (95% CI, 0.09–0.9), P=0.048. Patients with HCV who have had prior HBV infection may be at increased risk for HCC compared to patients with HCV who have not had HBV because HBV may promote carcinogenesis through mechanisms independent of HCV virus. Patients with single HCC’s less than 3 cm without vascular invasion treated with IFN were less likely to develop recurrent HCC compared to the control group, HR =0.4 (95% CI, 0.19–0.89), P=0.02. Investigators tested the efficacy of IFN-alpha in combination with 5-fluouracil in 30 patients with advanced HCC and tumor thrombi in the main portal vein after resection (91). Patients received subcutaneous IFN-alpha 5 MU three times a week postoperatively for a total dose of 60 MU. 5-FU at a dose of 300 mg/m2 was administered through the proper hepatic artery during the first and second postoperative week. The primary outcome was a complete response defined as normalization of tumor marker levels and disappearance of all tumors and portal vein thrombosis on CT or MRI. A partial response was defined as a decrease in tumor marker levels and a decrease in tumor size between 50–99% of the original size. The average tumor size was 16 mm. Six (20%) patients had a complete response, 4 (13%) patients had a partial response and 19 (63%) patients had progressive disease. The median overall survival was 9.5 months and 3-year survival rate was 21%. The median survival in patients with a complete or partial response and patients with disease progression or no changes was 29 and 6 months, respectively. The median overall survival for patients whose tumors stained IFN type 2 receptor (IFNAR2)-positive and IFNAR2-negative were 16 and 5.5 months respectively, P<0.0025. Although this study has several limitations, including lack of a control group and the authors did not provide the underlying etiology of liver disease it provides several ideas for future studies. The identification of IFNAR2 as a potential prognostic indicator of therapeutic efficacy of IFN is an interesting finding that should be explored in future studies. Others have evaluated IFN in combination with traditional chemotherapies after liver resection. Eighty-six patients with HCC and tumor thrombi in the main portal vein or branches were divided into two groups who underwent resection (92). One group received 5-FU, adriamycin, cisplatin, and IFN-alpha after resection and thrombectomy while the second group underwent resection and thrombectomy only. Median tumor free survival and overall survival in the group that received chemotherapy and the group that underwent resection only were 5.1 vs. 2.5 months, respectively, P=0.017 and 11.5 and 6.2 months, respectively, P=0.007. In multivariate analysis chemotherapy along with pathologic grading and tumor size were independent prognostic factors of tumor free survival.
The results of a meta-analysis demonstrated that IFN therapy appears to be effective after curative treatment for HCC in HCV patients because of improved survival and lower recurrence rates (96). However, the authors caution the routine use of IFN cannot be advocated based upon the available evidence because the studies included in the analysis were heterogeneous and in some cases benefits of IFN were only demonstrated in subgroup analyses. Some studies have included patients with early HCC while others have evaluated it in patients with more advanced cancer. Another difference among studies is some studies have included patients with HCV while other studies have included patients with HBV or both HBV and HCV. Patients with HBV and HCC in may not be comparable to patients with HCV and HCC because patients with HBV may develop HCC in the absence of advanced fibrosis and thus more likely to be resection candidates. Studies have compared IFN alone or in combination with other chemotherapeutic agents. A reasonable approach is to consider PEG-IFN with ribavirin after resection or ablation in patients who can tolerate therapy and who do not have decompensated cirrhosis with the goal of achieving virologic cure. The data do not support the routine use of IFN after resection or ablation in HCV patients with HCC.
Direct acting agents (DAA) for HCV and HCC
Use of IFN-free DAA for the treatment of HCV has been quite a revolution for the field of hepatology and virology. Traditional cure rates have risen from ~50% range to well above 90% in most groups of patients. Long term data is not yet available as to the impact of these newer agents and the incidence of HCC. It has been recognized that liver related complications such as hepatic encephalopathy and variceal hemorrhage are reduced and there is an improvement in hepatic function as demonstrated by the reduction in the Model for End-Stage Liver Disease (MELD) score (97). A retrospective study from Japan recently reported that HCV genotype 1b infected patients that were cured by DAA as compared to those cured by IFN had similar rates of HCC development after cure (98). This study compared 77 DAA treated patients with a historical database of 528 patients.
Recent reports have emerged demonstrating increased aggressiveness and rates of HCC recurrence in patients with cured HCV after achieving a complete response to resection or local ablation. Reig et al. reported from a multicenter cohort in Spain that HCC recurrence rates were calculated to be higher as compared to the placebo arm of the international STORM study (99). In this retrospective analysis, 103 subjects were treated with DAA, and 58 met criteria for inclusion. After a median of 5.7 months 16 subjects developed HCC recurrence in the following pattern: intrahepatic growth [3], new intrahepatic lesion (1 nodule in 5 subjects, up to 3 nodules less than or equal to 3 cm in 4 subjects, and 1 with multifocal disease). HCC treatment was with local ablation or resection. In a different study, Italian authors report an unusually high occurrence of HCC in patients with HCV related cirrhosis cured by DAA, again in a retrospective study (100). HCC was detected in 26 patients: 17 patients with previously treated HCC and 9 patients with no history of HCC. HCC recurrence rates were compared to historical data from the same institution.
Microenvironment and viral induced inflammation both play a key role in in chronic liver injury and tumor initiation (101). It has been well recognized that the immune system has an anti-tumor function. There is a complex and delicate equilibrium between a pro-tumor and anti-tumor function of the immune system. It has been proposed that HCV treatment with DAA modifies natural killer function and expression of IFN response (102,103). With the initiation of DAA, there is rapid decline in the burden of HCV RNA, and possibly dysregulation of the anti-tumor response. Additionally, there may be a disturbance of immune surveillance with this rapid viral clearance. Again, these postulations need further validation. Furthermore, many more patients with decompensated liver disease (Childs B and C cirrhosis) who were never previously candidates for HCV treatment are now being treated with DAA; these patients carry an incrementally higher risk of HCC vs. compensated patients. Conversely, a French collaborative group reported no evidence for increased risk of HCC who achieved SVR (104). This included patients that had evidence of hepatic decompensation and some that underwent liver transplantation.
Conclusions
Chronic HBV and HCV are both associated with the development of HCC, although through different mechanisms. Treatment of chronic HBV with oral antiviral therapy results in lower rates of HCC. The risk of HCC is substantially reduced in patients with chronic HCV who achieve virologic cure, but the risk is not completely eliminated and patients with advanced cirrhosis should continue surveillance for HCC. More studies are needed to elucidate the effect that DAA have on HCC. Certainly, patients who are otherwise treatment candidates should be considered for antiviral therapy with the goal of achieving virologic cure.
Acknowledgements
None.
Footnote
Conflicts of Interest: Dr. Russo: speakers bureau for Gilead (HBV and HCV); bureau: (HCV)Gilead, Merck and AbbVie, (HBV) Gilead; Bayer (hepatocellular). Dr. Zamor: speakers bureau for Gilead (HCV); (HCV)Gilead, Merck and AbbVie. Dr. deLemos has no conflicts of interest to declare.
References
- El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 2007;132:2557-76. [Crossref] [PubMed]
- Venook AP, Papandreou C, Furuse J, et al. The incidence and epidemiology of hepatocellular carcinoma: a global and regional perspective. Oncologist 2010;15 Suppl 4:5-13. [Crossref] [PubMed]
- Perz JF, Armstrong GL, Farrington LA, et al. The contributions of hepatitis B virus and hepatitis C virus infections to cirrhosis and primary liver cancer worldwide. J Hepatol 2006;45:529-38. [Crossref] [PubMed]
- Di Bisceglie AM. Hepatitis B and hepatocellular carcinoma. Hepatology 2009;49:S56-60. [Crossref] [PubMed]
- Yuen MF, Wong DK, Sablon E, et al. HBsAg seroclearance in chronic hepatitis B in the Chinese: virological, histological, and clinical aspects. Hepatology 2004;39:1694-701. [Crossref] [PubMed]
- Yuen MF, Wong DK, Fung J, et al. HBsAg Seroclearance in chronic hepatitis B in Asian patients: replicative level and risk of hepatocellular carcinoma. Gastroenterology 2008;135:1192-9. [Crossref] [PubMed]
- Zhou M, Wang H, Zhu J, et al. Cause-specific mortality for 240 causes in China during 1990-2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016;387:251-72. [Crossref] [PubMed]
- Zhu RX, Seto WK, Lai CL, et al. Epidemiology of Hepatocellular Carcinoma in the Asia-Pacific Region. Gut Liver 2016;10:332-9. [Crossref] [PubMed]
- Komatsu H. Hepatitis B virus: where do we stand and what is the next step for eradication? World J Gastroenterol 2014;20:8998-9016. [PubMed]
- Chang MH, Chen CJ, Lai MS, et al. Universal hepatitis B vaccination in Taiwan and the incidence of hepatocellular carcinoma in children. Taiwan Childhood Hepatoma Study Group. N Engl J Med 1997;336:1855-9. [Crossref] [PubMed]
- Sherman M. Risk of hepatocellular carcinoma in hepatitis B and prevention through treatment. Cleve Clin J Med 2009;76 Suppl 3:S6-9. [Crossref] [PubMed]
- Fattovich G, Stroffolini T, Zagni I, et al. Hepatocellular carcinoma in cirrhosis: incidence and risk factors. Gastroenterology 2004;127:S35-50. [Crossref] [PubMed]
- Wang SH, Yeh SH, Lin WH, et al. Estrogen receptor alpha represses transcription of HBV genes via interaction with hepatocyte nuclear factor 4alpha. Gastroenterology 2012;142:989-98 e4.
- Fattovich G, Giustina G, Christensen E, et al. Influence of hepatitis delta virus infection on morbidity and mortality in compensated cirrhosis type B. The European Concerted Action on Viral Hepatitis (Eurohep). Gut 2000;46:420-6. [Crossref] [PubMed]
- Kushner T, Serper M, Kaplan DE. Delta hepatitis within the Veterans Affairs medical system in the United States: Prevalence, risk factors, and outcomes. J Hepatol 2015;63:586-92. [Crossref] [PubMed]
- Sureau C, Negro F. The hepatitis delta virus: Replication and pathogenesis. J Hepatol 2016;64:S102-16. [Crossref] [PubMed]
- Donato F, Tagger A, Gelatti U, et al. Alcohol and hepatocellular carcinoma: the effect of lifetime intake and hepatitis virus infections in men and women. Am J Epidemiol 2002;155:323-31. [Crossref] [PubMed]
- Ming L, Thorgeirsson SS, Gail MH, et al. Dominant role of hepatitis B virus and cofactor role of aflatoxin in hepatocarcinogenesis in Qidong, China. Hepatology 2002;36:1214-20. [Crossref] [PubMed]
- Jiang DK, Sun J, Cao G, et al. Genetic variants in STAT4 and HLA-DQ genes confer risk of hepatitis B virus-related hepatocellular carcinoma. Nat Genet 2013;45:72-5. [Crossref] [PubMed]
- Clifford RJ, Zhang J, Meerzaman DM, et al. Genetic variations at loci involved in the immune response are risk factors for hepatocellular carcinoma. Hepatology 2010;52:2034-43. [Crossref] [PubMed]
- Gu X, Qi P, Zhou F, et al. +49G > A polymorphism in the cytotoxic T-lymphocyte antigen-4 gene increases susceptibility to hepatitis B-related hepatocellular carcinoma in a male Chinese population. Hum Immunol 2010;71:83-7. [Crossref] [PubMed]
- Chan KY, Wong CM, Kwan JS, et al. Genome-wide association study of hepatocellular carcinoma in Southern Chinese patients with chronic hepatitis B virus infection. PLoS One 2011;6:e28798. [Crossref] [PubMed]
- Zhang H, Zhai Y, Hu Z, et al. Genome-wide association study identifies 1p36.22 as a new susceptibility locus for hepatocellular carcinoma in chronic hepatitis B virus carriers. Nat Genet 2010;42:755-8. [Crossref] [PubMed]
- Iavarone M, Colombo M. HBV infection and hepatocellular carcinoma. Clin Liver Dis 2013;17:375-97. [Crossref] [PubMed]
- Chen CJ, Yang HI, Su J, et al. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA 2006;295:65-73. [Crossref] [PubMed]
- Guerrieri F, Belloni L, Pediconi N, et al. Molecular mechanisms of HBV-associated hepatocarcinogenesis. Semin Liver Dis 2013;33:147-56. [Crossref] [PubMed]
- Tseng TC, Liu CJ, Yang HC, et al. High levels of hepatitis B surface antigen increase risk of hepatocellular carcinoma in patients with low HBV load. Gastroenterology 2012;142:1140-1149.e3; quiz e13-4.
- Chan HL, Hui AY, Wong ML, et al. Genotype C hepatitis B virus infection is associated with an increased risk of hepatocellular carcinoma. Gut 2004;53:1494-8. [Crossref] [PubMed]
- Ni YH, Chang MH, Wang KJ, et al. Clinical relevance of hepatitis B virus genotype in children with chronic infection and hepatocellular carcinoma. Gastroenterology 2004;127:1733-8. [Crossref] [PubMed]
- Kao JH, Chen PJ, Lai MY, et al. Basal core promoter mutations of hepatitis B virus increase the risk of hepatocellular carcinoma in hepatitis B carriers. Gastroenterology 2003;124:327-34. [Crossref] [PubMed]
- Yang HI, Lu SN, Liaw YF, et al. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med 2002;347:168-74. [Crossref] [PubMed]
- Chen CJ, Yang HI, Iloeje UH, et al. Hepatitis B virus DNA levels and outcomes in chronic hepatitis B. Hepatology 2009;49:S72-84. [Crossref] [PubMed]
- Zoulim F, Locarnini S. Hepatitis B virus resistance to nucleos(t)ide analogues. Gastroenterology 2009;137:1593-608.e1-2.
- Kuang SY, Jackson PE, Wang JB, et al. Specific mutations of hepatitis B virus in plasma predict liver cancer development. Proc Natl Acad Sci U S A 2004;101:3575-80. [Crossref] [PubMed]
- Friedman SL. Mechanisms of hepatic fibrogenesis. Gastroenterology 2008;134:1655-69. [Crossref] [PubMed]
- Lee JM, Wong CM, Ng IO. Hepatitis B virus-associated multistep hepatocarcinogenesis: a stepwise increase in allelic alterations. Cancer Res 2008;68:5988-96. [Crossref] [PubMed]
- Kanai Y. Genome-wide DNA methylation profiles in precancerous conditions and cancers. Cancer Sci 2010;101:36-45. [Crossref] [PubMed]
- Um TH, Kim H, Oh BK, et al. Aberrant CpG island hypermethylation in dysplastic nodules and early HCC of hepatitis B virus-related human multistep hepatocarcinogenesis. J Hepatol 2011;54:939-47. [Crossref] [PubMed]
- Benhenda S, Cougot D, Buendia MA, et al. Hepatitis B virus X protein molecular functions and its role in virus life cycle and pathogenesis. Adv Cancer Res 2009;103:75-109. [Crossref] [PubMed]
- Levrero M, Zucman-Rossi J. Mechanisms of HBV-induced hepatocellular carcinoma. J Hepatol 2016;64:S84-S101. [Crossref] [PubMed]
- Beasley RP. Hepatitis B virus. The major etiology of hepatocellular carcinoma. Cancer 1988;61:1942-56. [Crossref] [PubMed]
- Beasley RP, Hwang LY, Lin CC, et al. Hepatocellular carcinoma and hepatitis B virus. A prospective study of 22 707 men in Taiwan. Lancet 1981;2:1129-33. [Crossref] [PubMed]
- Zhang BH, Yang BH, Tang ZY. Randomized controlled trial of screening for hepatocellular carcinoma. J Cancer Res Clin Oncol 2004;130:417-22. [Crossref] [PubMed]
- Terrault NA, Bzowej NH, Chang KM, et al. AASLD guidelines for treatment of chronic hepatitis B. Hepatology 2016;63:261-83. [Crossref] [PubMed]
- European Association For The Study Of The Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol 2012;57:167-85. [Crossref] [PubMed]
- NCCN Guidelines Version 2.2016 Updates Hepatobiliary Cancers. National Comprehensive Cancer Network, 2016.
- Chang TS, Wu YC, Tung SY, et al. Alpha-Fetoprotein Measurement Benefits Hepatocellular Carcinoma Surveillance in Patients with Cirrhosis. Am J Gastroenterol 2015;110:836-44. [Crossref] [PubMed]
- Gopal P, Singal AG. Reply: To PMID 24095974. Clin Gastroenterol Hepatol 2014;12:2139-40.
- Chen JG, Parkin DM, Chen QG, et al. Screening for liver cancer: results of a randomised controlled trial in Qidong, China. J Med Screen 2003;10:204-9. [Crossref] [PubMed]
- Hino O, Kajino K, Umeda T, et al. Understanding the hypercarcinogenic state in chronic hepatitis: a clue to the prevention of human hepatocellular carcinoma. J Gastroenterol 2002;37:883-7. [Crossref] [PubMed]
- Matsuzaki K, Murata M, Yoshida K, et al. Chronic inflammation associated with hepatitis C virus infection perturbs hepatic transforming growth factor beta signaling, promoting cirrhosis and hepatocellular carcinoma. Hepatology 2007;46:48-57. [Crossref] [PubMed]
- Schulze-Krebs A, Preimel D, Popov Y, et al. Hepatitis C virus-replicating hepatocytes induce fibrogenic activation of hepatic stellate cells. Gastroenterology 2005;129:246-58. [Crossref] [PubMed]
- Moriya K, Fujie H, Shintani Y, et al. The core protein of hepatitis C virus induces hepatocellular carcinoma in transgenic mice. Nat Med 1998;4:1065-7. [Crossref] [PubMed]
- Nkontchou G, Ziol M, Aout M, et al. HCV genotype 3 is associated with a higher hepatocellular carcinoma incidence in patients with ongoing viral C cirrhosis. J Viral Hepat 2011;18:e516-22. [Crossref] [PubMed]
- Castera L, Hezode C, Roudot-Thoraval F, et al. Effect of antiviral treatment on evolution of liver steatosis in patients with chronic hepatitis C: indirect evidence of a role of hepatitis C virus genotype 3 in steatosis. Gut 2004;53:420-4. [Crossref] [PubMed]
- Piodi A, Chouteau P, Lerat H, et al. Pawlotsky JM. Morphological changes in intracellular lipid droplets induced by different hepatitis C virus genotype core sequences and relationship with steatosis. Hepatology 2008;48:16-27. [Crossref] [PubMed]
- Kim JH, Park JW, Koh DW, et al. Efficacy of lamivudine on hepatitis B viral status and liver function in patients with hepatitis B virus-related hepatocellular carcinoma. Liver Int 2009;29:203-7. [Crossref] [PubMed]
- Liaw YF, Sung JJ, Chow WC, et al. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med 2004;351:1521-31. [Crossref] [PubMed]
- Yeo W, Mo FK, Chan SL, et al. Hepatitis B viral load predicts survival of HCC patients undergoing systemic chemotherapy. Hepatology 2007;45:1382-9. [Crossref] [PubMed]
- Yang T, Lu JH, Zhai J, et al. High viral load is associated with poor overall and recurrence-free survival of hepatitis B virus-related hepatocellular carcinoma after curative resection: a prospective cohort study. Eur J Surg Oncol 2012;38:683-91. [Crossref] [PubMed]
- Toyoda H, Kumada T, Tada T, et al. Transarterial chemoembolization for hepatitis B virus-associated hepatocellular carcinoma: improved survival after concomitant treatment with nucleoside analogues. J Vasc Interv Radiol 2012;23:317-22.e1. [Crossref] [PubMed]
- Hosaka T, Suzuki F, Kobayashi M, et al. Long-term entecavir treatment reduces hepatocellular carcinoma incidence in patients with hepatitis B virus infection. Hepatology 2013;58:98-107. [Crossref] [PubMed]
- Wang CC, Kao JH. How have the recent advances in antiviral therapy impacted the management of virus-related hepatocellular carcinoma? Expert Opin Pharmacother 2016;17:911-9. [Crossref] [PubMed]
- Kunimoto H, Ikeda K, Sorin Y, et al. Long-Term Outcomes of Hepatitis-C-Infected Patients Achieving a Sustained Virological Response and Undergoing Radical Treatment for Hepatocellular Carcinoma. Oncology 2016;90:167-75. [Crossref] [PubMed]
- Hiramatsu N, Oze T, Takehara T. Suppression of hepatocellular carcinoma development in hepatitis C patients given interferon-based antiviral therapy. Hepatol Res 2015;45:152-61. [Crossref] [PubMed]
- Khan F, Peltekian KM, Peterson TC. Effect of interferon-alpha, ribavirin, pentoxifylline, and interleukin-18 antibody on hepatitis C sera-stimulated hepatic stellate cell proliferation. J Interferon Cytokine Res 2008;28:643-51. [Crossref] [PubMed]
- Tasci I, Mas MR, Vural SA, et al. Rat liver fibrosis regresses better with pegylated interferon alpha2b and ursodeoxycholic acid treatments than spontaneous recovery. Liver Int 2006;26:261-8. [Crossref] [PubMed]
- Wang L, Wu WZ, Sun HC, et al. Mechanism of interferon alpha on inhibition of metastasis and angiogenesis of hepatocellular carcinoma after curative resection in nude mice. J Gastrointest Surg 2003;7:587-94. [Crossref] [PubMed]
- Cao B, Chen XP, Zhu P, et al. Inhibitory effect of interferon-alpha-2b on expression of cyclooxygenase-2 and vascular endothelial growth factor in human hepatocellular carcinoma inoculated in nude mice. World J Gastroenterol 2008;14:6802-7. [Crossref] [PubMed]
- Nakamura M, Nagano H, Sakon M, et al. Role of the Fas/FasL pathway in combination therapy with interferon-alpha and fluorouracil against hepatocellular carcinoma in vitro. J Hepatol 2007;46:77-88. [Crossref] [PubMed]
- Papatheodoridis GV, Papadimitropoulos VC, Hadziyannis SJ. Effect of interferon therapy on the development of hepatocellular carcinoma in patients with hepatitis C virus-related cirrhosis: a meta-analysis. Aliment Pharmacol Ther 2001;15:689-98. [Crossref] [PubMed]
- MacParland SA, Pham TN, Guy CS, et al. Hepatitis C virus persisting after clinically apparent sustained virological response to antiviral therapy retains infectivity in vitro. Hepatology 2009;49:1431-41. [Crossref] [PubMed]
- Hayashi T, Tamori A, Nishikawa M, et al. Differences in molecular alterations of hepatocellular carcinoma between patients with a sustained virological response and those with hepatitis C virus infection. Liver Int 2009;29:126-32. [Crossref] [PubMed]
- Veldt BJ, Heathcote EJ, Wedemeyer H, et al. Sustained virologic response and clinical outcomes in patients with chronic hepatitis C and advanced fibrosis. Ann Intern Med 2007;147:677-84. [Crossref] [PubMed]
- Kobayashi S, Takeda T, Enomoto M, et al. Development of hepatocellular carcinoma in patients with chronic hepatitis C who had a sustained virological response to interferon therapy: a multicenter, retrospective cohort study of 1124 patients. Liver Int 2007;27:186-91. [Crossref] [PubMed]
- Ikeda K, Saitoh S, Arase Y, et al. Effect of interferon therapy on hepatocellular carcinogenesis in patients with chronic hepatitis type C: A long-term observation study of 1,643 patients using statistical bias correction with proportional hazard analysis. Hepatology 1999;29:1124-30. [Crossref] [PubMed]
- Yoshida H, Shiratori Y, Moriyama M, et al. Interferon therapy reduces the risk for hepatocellular carcinoma: national surveillance program of cirrhotic and noncirrhotic patients with chronic hepatitis C in Japan. IHIT Study Group. Inhibition of Hepatocarcinogenesis by Interferon Therapy. Ann Intern Med 1999;131:174-81. [Crossref] [PubMed]
- Imai Y, Kawata S, Tamura S, et al. Relation of interferon therapy and hepatocellular carcinoma in patients with chronic hepatitis C. Osaka Hepatocellular Carcinoma Prevention Study Group. Ann Intern Med 1998;129:94-9. [Crossref] [PubMed]
- Sanefuji K, Kayashima H, Iguchi T, et al. Characterization of hepatocellular carcinoma developed after achieving sustained virological response to interferon therapy for hepatitis C. J Surg Oncol 2009;99:32-7. [Crossref] [PubMed]
- Shiffman ML, Hofmann CM, Contos MJ, et al. A randomized, controlled trial of maintenance interferon therapy for patients with chronic hepatitis C virus and persistent viremia. Gastroenterology 1999;117:1164-72. [Crossref] [PubMed]
- Nishiguchi S, Kuroki T, Nakatani S, et al. Randomised trial of effects of interferon-alpha on incidence of hepatocellular carcinoma in chronic active hepatitis C with cirrhosis. Lancet 1995;346:1051-5. [Crossref] [PubMed]
- Di Bisceglie AM, Shiffman ML, Everson GT, et al. Prolonged therapy of advanced chronic hepatitis C with low-dose peginterferon. N Engl J Med 2008;359:2429-41. [Crossref] [PubMed]
- Lok AS, Seeff LB, Morgan TR, et al. Incidence of hepatocellular carcinoma and associated risk factors in hepatitis C-related advanced liver disease. Gastroenterology 2009;136:138-48. [Crossref] [PubMed]
- Arase Y, Ikeda K, Suzuki F, et al. Prolonged-interferon therapy reduces hepatocarcinogenesis in aged-patients with chronic hepatitis C. J Med Virol 2007;79:1095-102. [Crossref] [PubMed]
- Tamura Y, Yamagiwa S, Aoki Y, et al. Serum alpha-fetoprotein levels during and after interferon therapy and the development of hepatocellular carcinoma in patients with chronic hepatitis C. Dig Dis Sci 2009;54:2530-7. [Crossref] [PubMed]
- Patt YZ, Yoffe B, Charnsangavej C, et al. Low serum alpha-fetoprotein level in patients with hepatocellular carcinoma as a predictor of response to 5-FU and interferon-alpha-2b. Cancer 1993;72:2574-82. [Crossref] [PubMed]
- Lai CL, Lau JY, Wu PC, et al. Recombinant interferon-alpha in inoperable hepatocellular carcinoma: a randomized controlled trial. Hepatology 1993;17:389-94. [Crossref] [PubMed]
- Llovet JM, Sala M, Castells L, et al. Randomized controlled trial of interferon treatment for advanced hepatocellular carcinoma. Hepatology 2000;31:54-8. [Crossref] [PubMed]
- Uenishi T, Nishiguchi S, Tanaka S, et al. Response to interferon therapy affects risk factors for postoperative recurrence of hepatitis C virus-related hepatocellular carcinoma. J Surg Oncol 2008;98:358-62. [Crossref] [PubMed]
- Mazzaferro V, Romito R, Schiavo M, et al. Prevention of hepatocellular carcinoma recurrence with alpha-interferon after liver resection in HCV cirrhosis. Hepatology 2006;44:1543-54. [Crossref] [PubMed]
- Nagano H, Miyamoto A, Wada H, et al. Interferon-alpha and 5-fluorouracil combination therapy after palliative hepatic resection in patients with advanced hepatocellular carcinoma, portal venous tumor thrombus in the major trunk, and multiple nodules. Cancer 2007;110:2493-501. [Crossref] [PubMed]
- Liang LJ, Hu WJ, Yin XY, et al. Adjuvant intraportal venous chemotherapy for patients with hepatocellular carcinoma and portal vein tumor thrombi following hepatectomy plus portal thrombectomy. World J Surg 2008;32:627-31. [Crossref] [PubMed]
- Ikeda K, Arase Y, Saitoh S, et al. Interferon beta prevents recurrence of hepatocellular carcinoma after complete resection or ablation of the primary tumor-A prospective randomized study of hepatitis C virus-related liver cancer. Hepatology 2000;32:228-32. [Crossref] [PubMed]
- Shiratori Y, Shiina S, Teratani T, et al. Interferon therapy after tumor ablation improves prognosis in patients with hepatocellular carcinoma associated with hepatitis C virus. Ann Intern Med 2003;138:299-306. [Crossref] [PubMed]
- Jeong S, Aikata H, Katamura Y, et al. Low-dose intermittent interferon-alpha therapy for HCV-related liver cirrhosis after curative treatment of hepatocellular carcinoma. World J Gastroenterol 2007;13:5188-95. [Crossref] [PubMed]
- Kudo M. Impact of interferon therapy after curative treatment of hepatocellular carcinoma. Oncology 2008;75 Suppl 1:30-41. [Crossref] [PubMed]
- Manns M, Samuel D, Gane EJ, et al. Ledipasvir and sofosbuvir plus ribavirin in patients with genotype 1 or 4 hepatitis C virus infection and advanced liver disease: a multicentre, open-label, randomised, phase 2 trial. Lancet Infect Dis 2016;16:685-97. [Crossref] [PubMed]
- Kobayashi M, Suzuki F, Fujiyama S, et al. Sustained virologic response by direct antiviral agents reduces the incidence of hepatocellular carcinoma in patients with HCV infection. J Med Virol 2017;89:476-83. [Crossref] [PubMed]
- Reig M, Marino Z, Perello C, et al. Unexpected high rate of early tumor recurrence in patients with HCV-related HCC undergoing interferon-free therapy. J Hepatol 2016;65:719-26. [Crossref] [PubMed]
- Conti F, Buonfiglioli F, Scuteri A, et al. Early occurrence and recurrence of hepatocellular carcinoma in HCV-related cirrhosis treated with direct-acting antivirals. J Hepatol 2016;65:727-33. [Crossref] [PubMed]
- Makarova-Rusher OV, Medina-Echeverz J, Duffy AG, et al. The yin and yang of evasion and immune activation in HCC. J Hepatol 2015;62:1420-9. [Crossref] [PubMed]
- Meissner EG, Kohli A, Virtaneva K, et al. Achieving sustained virologic response after interferon-free hepatitis C virus treatment correlates with hepatic interferon gene expression changes independent of cirrhosis. J Viral Hepat 2016;23:496-505. [Crossref] [PubMed]
- Serti E, Park H, Keane M, et al. Rapid decrease in hepatitis C viremia by direct acting antivirals improves the natural killer cell response to IFNα. Gut 2017;66:724-35. [Crossref] [PubMed]
- ANRS collaborative study group on hepatocellular carcinoma (ANRS CO22 HEPATHER, CO12 CirVir and CO23 CUPILT cohorts). Lack of evidence of an effect of direct-acting antivirals on the recurrence of hepatocellular carcinoma: Data from three ANRS cohorts. J Hepatol 2016;65:734-40. [Crossref] [PubMed]


