Depression, anxiety, and health related quality of life among colorectal cancer survivors
Introduction
Anxiety and/or depression are the most frequent mental disorders among patients with malignant cancer (1-3). The prevalence of clinical depression in cancer patients has been reported to be 13% to 40% (4). Depression and higher levels of depressive symptoms is linked to an increased mortality (5). Moreover, depression is a significant symptom for approximately 25% of palliative care patients (6). Routine screening for depression in the cancer clinical setting and referrals to mental health specialists should be taken into consideration (7,8). There is some evidence that anxiety and depression are strongly associated with poor quality of life (QOL) in colorectal cancer (CRC) patients (9). Further research is in place to examine whether the treatment of depression can increase the survival of depressed cancer patients beyond the QOL improvement (5). On the other hand, anxiety is even more frequent in cancer patients than depression (10).
Health related quality of life (HRQOL) is a multidimensional construct and is an important concept that, only in recent decades, there has been a considerable increase in studies reporting on HRQOL. It covers a range of the subjective perceptions from physical, emotional, social, and cognitive functions to disease symptoms and treatment side effects among cancer patients (11). HRQOL has been considered as a critical aspect of cancer patients’ care in clinical setting by many clinicians (12). Assessment of the psychological distress in people with cancer is very important as psychological wellbeing is one of the key dimensions of the HRQOL (13).
Few studies have examined psychological distress or the association between the Hospital Anxiety and Depression Scale (HADS) and the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C30 version 3.0 (EORTC QLQ-C30 v.3) in patients with various cancers (14,15). In fact, only one study was found which has addressed such a relationship in a relatively large series of CRC survivors (16).
The present study aims at examining the relationship between psychological morbidity (as measured by the HADS) and quality of life (as measured by EORTC QLQ-C30 v.3) in colorectal survivors in the north of Iran. We have already reported that the prevalence of psychological distress among CRC survivor in this area is considerable and they have relatively poor QOL (17,18).
Methods
Participants of the study
This cross-sectional study was conducted in the city of Babol which is located to the north of Iran. The Babol cancer registry, established in 1960s (19), is the first population-based cancer registry in Iran. For the purpose of the present study, the CRC survivors were selected from the registry database. Subjects with C18 (colon), C19 (recto-sigmoid junction), C20 (rectum), and C21 (anus and anal canal) codes who had been recorded between 2007 and 2013 were included in this study (n=332). The inclusion criteria were as follows: (I) having, at least, one of the listed codes; (II) being alive; (III) currently residing in Babol; and (IV) being diagnosed during the specified periods. Lack of cooperation and incorrect address or phone number were the exclusion criteria. After exclusion of people who did not resided in Babol any more (37 cases), died (112 cases), migrated (six cases), were non-cooperative (four cases) or had incorrect phone and home addresses at the registry (16 cases), the questionnaires were completed for all the remaining 157 patients.
Measures
Demographic information including age, level of education, employment status and place of residency was collected via self-report. Age was categorized into two categories; <50 and ≥50 years, level of education was classified as illiterate, literate, occupation classed into (paid work or out of work) and finally place of residency specified as either urban or rural. Patients were also asked whether they experienced various comorbid conditions (including heart disease, hypertension, chronic back pain, arthritis, stroke, osteoporosis, asthma, chronic obstructive pulmonary disease, stomach and/or intestinal.
Participants were interviewed by two trained interviewers and the EORTC QLQ C-30 (version 3.0) and the HADS scales were completed. A Persian version of the two questionnaires which had already been validated prior to the study were also used in this survey (20,21). Each of the subscales, namely HADS-A (anxiety) and HADS-D (depression), consist of seven items, and both of them had scores ranging from 0 (no problems) to 3 (maximum distress) resulting in a sum score ranging from 0 to 21 for both anxiety and depression. “Cases” were defined based on score of 11 and more in HADS-A, HADS-D and HADS-T,
Statistical analysis
All relationships between the HADS and QLQ-C30 scales were assessed by linear regression, using the original scores of HADS and transformed scores of QLQ-C30. In the present study, HADS-A, HADS-D, and HADS-T were used as continuous variables. In the regression analyses, HADS was the independent variable and EF the dependent variable. Age, sex, location of the tumor, and the extent of disease were analyzed as additional covariates. In a further step, HADS-A and HADS-D were fed into a multiple linear regression analysis, with different QOL dimensions being the dependent variables. Agreement between HADS-A, HADS-D, and HADS-T and the EF dimension was evaluated for all the patients. Subsequently, the influence of sex, age, location of the tumor (colon vs. rectum) and the extent of disease on the HADS and EF scale was studied. Then, the associations between HADS-A and HADS-D and every dimensions of the QLQ-C30 were investigated. P value of less than 0.01 was predetermined to be mean statistical significance and SPSS version 21 was used for all data analyses.
This study received Ethics approval from the ethics committee of Tabriz University of Medical Sciences (TBZMED.1392.220). All patients completed an informed consent form prior to the interview session.
Results
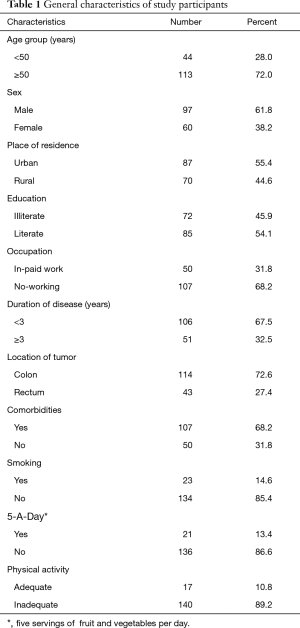
A total of 157 CRC survivors were included in this study with a mean age of 56.71 (SD 13.78). The majority of them were male (61.8%), over 50 years of age (72%), and more than half resided in urban areas. About 46% of them had no education, and about two-third were then out of work. The majority of them (68%) were diagnosed less than 3 years ago and 67% of survivors had at least one comorbid condition (Table 1).
Full table
Prevalence of psychological distress
In the present study, based on HADS-D, the frequency of depression was 20.4% and 17.2% of the participants were designated as borderline after scoring process. Similarly, according to HADS-A, the frequency of anxiety was 31.8% and only 14% of the patients were scored as borderline. However, 16.6% of the patients scored equal to or less than 11 on both HADS-A and HADS-D.
Table 2 shows the mean (SD) score for different dimensions of QOL and HADS-A, HADS-D, and HADS-T. As it can be seen, older patients, female, illiterate patients, those out of work, and those with inadequate physical activity had significantly higher levels of symptoms of distress (fatigue, pain) and lower scores for total QOL, and EF, PF, SF dimensions. The same results hold for those diagnosed with comorbid condition. Likewise, females, those suffering from comorbidity as well as those who had inadequate physical activity got significantly lower scores in CF dimension. Finally, illiterate patients and those who were not working and patients with comorbid conditions had significantly lower scores for RF dimension.

Full table
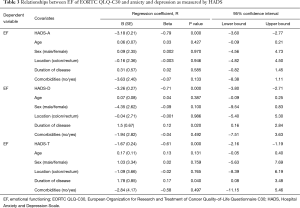
There were statistically a significant association between the EF dimension and each of the three HADS scores (P<0.001). Duration of disease was a significant independent covariate for the relationships between the EF dimension, HADS-T and HADS-D. However, this was not the case with HADS-A (Table 3). In case of equal scores obtained for both HADS-T and HADS-D, patients having lower duration of disease reported better EF than long-term survivors.
Full table
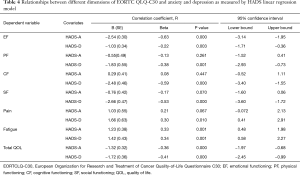
Table 4 shows the association between different dimensions of QLQ-C30 and three measures of HADS (HADS-A, HADS-D, HADS-T). There were significant relationships between all dimensions of QLQ-C30 and HADS-D score. By the same token, the same was true with HADS-A, except for PF and CF dimensions. The relationships between SF and pain dimensions and HADS-A were not found to be statistically significant (P=0.07). Overall, depression not only was a strong predictor of reduced QOL in all its dimensions, it but also seemed to be a stronger predictor of reduced QOL dimensions than anxiety.
Full table
Discussion
HRQOL has become an important outcome measure for cancer patients (12). The EF dimension of the QLQ-C30, as one of the key dimensions of HRQOL, is expected to detect psychological distress among cancer patients. We examined the relationship between psychological morbidity and QOL in CRC survivors in the north of Iran.
To our knowledge, hitherto only one study has examined the association between the EF dimension of the QLQ-C30 and the HADS among CRC survivors (16), and studies which have assessed such a relationship in patients with various cancer sites are far and few between (14,15).
In the current study, the frequency of depression, as obtained by HADS-D, was 20.4% and 17.2% of the participants were specified as borderline. Based on HADS-A, the frequency of anxiety was 31.8% and 14% of the patients fall into borderline.
Our patients’ reports showed high prevalence of psychological distress compared with study done by Skarstein et al. (22). The prevalence of “cases” with anxiety and depression was13% and 9% respectively. It was lower compared to study undertaken by Mystakidou et al. (14) which reported that the prevalence of “cases” with depression was 25.8%, and with anxiety was 24.2%. Our result was also different from the findings reported by Tsunoda et al. (16) which reported the prevalence of anxiety to be 7.8% (10/128) and depression to be 36.7% (47/128). The reason for this difference might be explained by the type of cancer which was a selection of various cancers in a study conducted by Skarstein et al. (22) or the stage of disease which was advanced cancer cases in the study conducted by Mystakidou et al. (14). Alternatively, it might be triggered as a result of different cut-off points which can be seen in the study conducted by Tsunoda et al. (16).
In our study, we found a strong significant association between the EF dimension and each of the three HADS scores. A similar result has been reported in a study conducted by Mystakidou et al. (14) with patients suffering from advanced cancer (n=120). Moreover, Tsunoda et al. (16) and Skarstein et al. (22) found a significant association between HADS-A, HADS-D and EF. The association between EF and HADS-D was, even, weaker than that of reached between EF and HADS-A. In our study, the coefficient of correlation for HADS-A was close to the coefficient calculated for HADS-D. To be more specific, the respective values for HADS-A and HADS-D read −0.79 and −0.71, respectively.
It was found that in case of equal scores for HADS-T and HADS-D, patients with lower duration of disease reported better EF than long-term survivors. In addition, age, sex, location of disease and comorbid conditions were not influential factors. This finding agrees with both a study conducted by Tsunoda et al. study (16) and another study carried out by Grassi et al. (15) which reported that none of the factors as such age, sex, location of the tumor, or extent of disease had an effect on the association between HADS-D and EF. In contrast, Skarstein et al. (22) found that in the event of having equal scores for HADS-T and HADS-D, male patients reported better EF than females. Similarly, older patients reported to enjoy a better EF than younger ones. These might be introduced by the impact of the cancer site.
There was strong association between both HADS-A and HADS-D and global QOL. In the present study, significant relationships between all dimensions of QLQ-C30 and HAD-D score, were seen, which are similar to the results of some other studies (15,16,22). HADS-A was, solely, related to EF and fatigue dimensions. Although, the relationships between SF, Pain dimensions and HADS-A were not statistically significant, they might be clinically important (P=0.07).
Few studies, also, have examined the agreement between EORTC QLQ-C30 scale and other questionnaires assessing anxiety and depression which yielded different results. For example, Fayers et al. (23) found a relatively poor correlation between the EF dimension of the EORTC QLQ-C30 and the Medical Outcomes Study 36-Item Short Form Health Survey (SF36). Psychological distress was not significantly different when HADS was used as compared to applying the Rotterdam Symptom Checklist in the same group of patients with advanced breast cancer (21).
Our study has both strengths and limitations. The main strengths were the high participation rate and the use of a group of CRC survivors as the study population selected through a population-based cancer registry. However, as to the limitation of the study it should be noted that people with advanced disease might have not been included in this study. In addition, unfortunately the researchers did not find any similar studies in Iran for comparison purposes therefore it is advisable to replicate the present study in other parts of Iran due to the point that different lifestyle and support may affect both psychological distress and the QOL of patients.
Conclusions
The current study found that EF dimension of the QLQ-C30 questionnaire covered anxiety and depression in CRC survivors in the north of Iran. Moreover, there found to be a strong association between both HADS-A and HADS-D and global QOL. In addition to that, compared with HADS-A, significant relationships between all dimensions of QLQ-C30 and HAD-D scores were seen (HADS-A was related to only EF and fatigue dimensions). Beyond QLQ-C30, HADS could be a suitable instrument for screening psychological distress among patients with CRC. On top of that, the relationship between HADS and QLQ-C30, as achieved in the present study, was similar to that of reported in other investigations done in western and Asian countries albeit in two different cultural settings.
In sum, there found a relatively high frequency of anxiety and depression cases which can indicate lack of routine screening and mismanagement of psychological distress in cancer clinics.
Acknowledgements
A substantial part of this study was funded by the research council, Tabriz University of Medical Sciences for which we are thankful. We extend our gratitude to staff working at the Babol cancer registry. We would also like to sincerely thank Mr. Habib Zadeh, Mr. Mirzad, Mrs. Mousavi, the staff at the Screening and Counselling Centre of Babol as well as all patients and their respective families who participated in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical statement: This study received Ethics approval from the ethics committee of Tabriz University of Medical Sciences (TBZMED.1392.220). All patients completed an informed consent form prior to the interview session.
References
- Pasquini M, Biondi M. Depression in cancer patients: a critical review. Clin Pract Epidemiol Ment Health 2007;3:2. [Crossref] [PubMed]
- Sivesind D, Baile WF. The psychologic distress in patients with cancer. Nurs Clin North Am 2001;36:809-25. viii. [PubMed]
- Stiefel F, Razavi D. Common psychiatric disorders in cancer patients. II. Anxiety and acute confusional states. Support Care Cancer 1994;2:233-7. [Crossref] [PubMed]
- Sellick SM, Crooks DL. Depression and cancer: an appraisal of the literature for prevalence, detection, and practice guideline development for psychological interventions. Psychooncology 1999;8:315-33. [Crossref] [PubMed]
- Pinquart M, Duberstein PR. Depression and cancer mortality: a meta-analysis. Psychol Med 2010;40:1797-810. [Crossref] [PubMed]
- Lawrie I, Lloyd-Williams M, Taylor F. How do palliative medicine physicians assess and manage depression. Palliat Med 2004;18:234-8. [Crossref] [PubMed]
- Prasad SM, Eggener SE, Lipsitz SR, et al. Effect of depression on diagnosis, treatment, and mortality of men with clinically localized prostate cancer. J Clin Oncol 2014;32:2471-8. [Crossref] [PubMed]
- Die Trill M. Psychological aspects of depression in cancer patients: an update. Ann Oncol 2012;23 Suppl 10:x302-5. [Crossref] [PubMed]
- Alacacioglu A, Binicier O, Gungor O, et al. Quality of life, anxiety, and depression in Turkish colorectal cancer patients. Support Care Cancer 2010;18:417-21. [Crossref] [PubMed]
- Lloyd-Williams M, Reeve J, Kissane D. Distress in palliative care patients: developing patient-centred approaches to clinical management. Eur J Cancer 2008;44:1133-8. [Crossref] [PubMed]
- Leplège A, Hunt S. The problem of quality of life in medicine. JAMA 1997;278:47-50. [Crossref] [PubMed]
- Osoba D. Lessons learned from measuring health-related quality of life in oncology. J Clin Oncol 1994;12:608-16. [PubMed]
- Velikova G, Stark D, Selby P. Quality of life instruments in oncology. Eur J Cancer 1999;35:1571-80. [Crossref] [PubMed]
- Mystakidou K, Tsilika E, Parpa E, et al. Assessment of anxiety and depression in advanced cancer patients and their relationship with quality of life. Qual Life Res 2005;14:1825-33. [Crossref] [PubMed]
- Grassi L, Indelli M, Marzola M, et al. Depressive symptoms and quality of life in home-care-assisted cancer patients. J Pain Symptom Manage 1996;12:300-7. [Crossref] [PubMed]
- Tsunoda A, Nakao K, Hiratsuka K, et al. Anxiety, depression and quality of life in colorectal cancer patients. Int J Clin Oncol 2005;10:411-7. [Crossref] [PubMed]
- Nikbakht HA, Aminisani N, Hosseini SR, et al. Prevalence of anxiety and depression in patients with colorectal cancer in Babol - north of Iran (2008-12). J Gorgan Uni Med Sci 2016;18:101-7.
- Nikbakht HA, Sani AN, Asghari Jafarabadi M, et al. Quality of life and its determinants among colorectal cancer survivors. J Kermanshah Uni Med Sci 2015;19:84-92.
- Etemadi A, Sadjadi A, Semnani S, et al. Cancer registry in Iran: a brief overview. Arch Iran Med 2008;11:577-80. [PubMed]
- Montazeri A, Harirchi I, Vahdani M, et al. The European Organization for Research and Treatment of Cancer Quality of Life Questionnaire (EORTC QLQ-C30): translation and validation study of the Iranian version. Support Care Cancer 1999;7:400-6. [Crossref] [PubMed]
- Montazeri A, Vahdaninia M, Ebrahimi M, et al. The Hospital Anxiety and Depression Scale (HADS): translation and validation study of the Iranian version. Health Qual Life Outcomes 2003;1:14. [Crossref] [PubMed]
- Skarstein J, Aass N, Fosså SD, et al. Anxiety and depression in cancer patients: relation between the Hospital Anxiety and Depression Scale and the European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire. J Psychosom Res 2000;49:27-34. [Crossref] [PubMed]
- Fayers PM, Hand DJ, Bjordal K, et al. Causal indicators in quality of life research. Qual Life Res 1997;6:393-406. [Crossref] [PubMed]


