Effect of gender on psychosocial adjustment of colorectal cancer survivors with ostomy
Introduction
The incidence of colorectal cancer is in increasing trend and considering the advancement in detection, treatment and surgical techniques it is likely that number of colorectal cancer survivors is going to increase in near future (1,2). In addition to the detrimental effect of cancer itself, most of the colorectal survivors have to deal with ostomy as a part of their treatment (3). Ostomy refers to a surgical procedure that results in an artificial opening in the abdominal wall (stoma) through which bodily waste are excreted (4). To the ostomate, however, it means substantive changes not only in bodily appearance and functional ability but also in overall personal hygiene (5).
Although ostomy is regarded as a life saving surgery, studies have consistently reported low quality of life (QoL) scores in patients with ostomy (6,7). Furthermore, qualitative analysis has explored that low score in QoL is mainly attributable to the psychosocial issues (8-11). Yet, clinical outcome measures are mostly confined to laboratory results, complication rates and death, which often overlook those aspects of functioning and fall short to provide complete picture of how patient’s life has been affected by the disease and its sequelae. Hence, detail analysis of psychosocial adjustment to measure actual outcome in these population is very essential, where psychosocial adjustment is the integration of illness or disability into the individual’s life, identity, self concept, and body image (12).
Deep rooted differences in men and women in societies can shape people’s lives and their adjustment. It is essential to recognize and reflect upon gender roles given the need to provide therapeutic guidance and develop programs and public policies for each health specialty (13). Gender norms, roles and relations can influence health outcomes and affect the attainment of mental, physical and social health and well-being (14). Gender here, simply means social differences whereas sex is the biological difference between men and women.
It is imperative to note that differences in relation to access to health services, uptake of health services, family support, experiences in health-care settings can influence adjustment of men and women respectively (15). Considering the multiple roles of a women in developing countries such as preparing food for the family, cleaning, taking care of husband, children, older adults, and managing home and work, it is expected that illness is likely to affect women in greater extent than in men.
Although, much research has been done in relation to gender differences in adjustment to illness, results are inconclusive. A study have shown that women report more psychological distress due to illness than men, yet, general satisfaction with life were almost comparable (16). Another study, however, has reported favorable outcome in women’s adjustment in case of cancer as compared to men (17). In contrast to this, another study has shown that women report more adjustment problems as compared to men (18).
The variation in adjustment between men and women may be attributable to the differences in coping style between them. Precisely, women are more likely than men to internalize the stress and use emotion focused ways of coping whereas, men prefer problem solving positive behavior. Moreover, societies seem to be more supportive to men than women when it comes to accepting their illness and its sequelae (15).
Thus, considering the differences in various attribute between men and women, it is likely that adjustment to chronic illness will significantly vary by gender. Little is known, however, about the effect of gender on the psychosocial adjustment of colorectal cancer survivors with ostomy. Therefore, this study was carried out with an aim to address these concerns among them.
Methods
Design
A descriptive cross-sectional study was carried out.
Settings and subjects
The study comprised purposively selected 122 colorectal cancer survivors with ostomy (62 men, 60 women) aged 24–76 years visiting the stoma clinic of B.P. Koirala Memorial Cancer Hospital, Bharatpur.
Inclusion criteria
Colorectal cancer survivors with ostomy for at least 6 months before data collection were included in the study.
Ethical considerations
Ethical clearance was obtained from Institutional Review Board of Tribhuvan University, Institute of Medicine. Administrative approval was obtained from authorities of selected hospital. Informed consent was obtained from every patient before collecting data. Researchers (nurses) collected data through face to face interview technique in separate place allocated by the staffs of ostomy clinics. Around 30 minutes was taken to collect data from each respondent.
Tools for data collection
Data were collected using three questionnaires.
- Socio-demographic characteristics: age, sex, employment status and perceived family support;
- Clinical characteristics: time since surgery, treatment, complications, comorbidities, and self care efficacy;
- Psychosocial adjustment: Ostomy Adjustment Inventory-23 (OAI-23) developed by Simmons, Smith and Maekawa (19) was used to assess psychosocial adjustment which is a Likert scale containing 20 items with four subscales: acceptance, anxious preoccupation, social engagement and anger. Scoring: each item could be answered on a 5 point scale where 0 indicates strongly disagree and four indicates strongly agree. The total score was obtained from the sum scores of the items. The highest score possible was thus 80 and lowest 0. Ten items had reverse scoring as they are negatively phrased. Higher scores indicated better adjustment. The decision to use this tool was based on its focus on long term psychosocial adjustment and established psychometric properties. Cronbach’s α=0.93 for overall scale, r=0.83 and α 0.87, 0.74, 0.80, 0.64 for each subscale (19). Permission to use this tool was obtained from Kingsley Simmons, University of Hertfordshire. The tool was translated into Nepali language and then back translated into English language by two independent bilingual translators. The back translated tool was sent to the original author of the tool for verification (retention of same meaning). Before conducting the study, the tool was pre-tested. The Cronbach’s alpha was 0.874 for overall scale; indicating the translated Nepali Likert scale is highly reliable.
Statistical analysis
Statistical Package for Social Sciences (SPSS version 20) was used for data analysis. Continuous variables were expressed using mean and standard deviation. Qualitative variables were described using frequency and percentage. Some of the quantitative data were converted into categorical data to facilitate analysis. Normality of the quantitative variable was verified using Shapiro Wilk test and the data were found to be normally distributed (P>0.05). Pearson chi-square was used to determine difference in socio-demographic, clinical characteristics by gender. Independent t-test was used to compare mean score of overall psychosocial adjustment and its subscales in men and women.
To determine the predictability of gender on the subscales of psychosocial adjustment, hierarchical regression analysis was conducted, where confounders (age, perceived family support and employment status) were entered in step 1 and gender was added next in step 2.
Separate multiple regression analysis was conducted to determine the predictors of psychosocial adjustment in men and women. First of all, univariate analysis with the outcome measure (psychosocial adjustment) was done to determine the potential predictors in men and women separately. Variables significant in univariate analysis with an association of P≤0.05 were entered in the multivariate model. Finally, the best predictive model was constructed for men and women separately, using a enter method, deleting those variables that had the weakest association with the psychosocial adjustment score. Autocollinearity was tested by using Durbin Watson test. The significance level (P) was set at ≤0.05 for inferential statistics.
Results
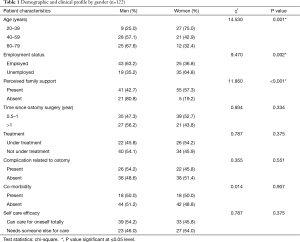
A total of 122 patients (62 men, 60 women) were included in the study. The mean age of the patients was 49.96 years, ranging from 24 to 76 years. The mean ages of 62 men and 60 women were 55.69 and 44.03 years, respectively. In order to avoid possible confounding effects, comparability between genders was examined with regard to socio-demographic and clinical variables. Age (P<0.001), employment status (P=0.002) and perceived family support (P<0.001) differed significantly between men and women. Majority of the women were in the age group of ≤40 years, unemployed and had perceived family support as compared to their male counterparts. However, there was no significant difference in time since surgery, treatment, complication, comorbidity and self care efficacy between men and women (Table 1).
Full table
Psychosocial adjustment by gender
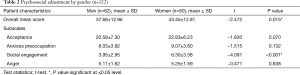
The overall mean score in psychosocial adjustment scale was 40.52±13.16 showing moderate impairment in the psychosocial adjustment and the mean score of acceptance, anxious preoccupation, social engagement and anger was 21.69±6.86, 8.54±3.79, 5.11±3.36, 5.18±1.60 respectively.
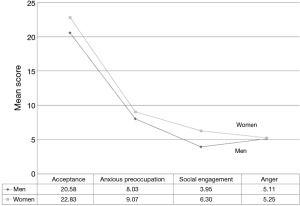
The difference between men and women in psychosocial adjustment and its various domains is presented in Figure 1. Both men and women had significant impairment in the psychosocial adjustment, however, men had significantly lower psychosocial adjustment score (37.68±12.96 vs. 43.45±12.81, t=−2.47, P=0.015) at 95% CI as compared to women. Although men reported lower score in all the domains of psychosocial adjustment than women, difference in the social engagement domain was only one statistically significant, where men reported significantly lower social engagement score than women (3.95±2.95 vs. 6.30±3.38, t=−4.091, P≤0.001) (Table 2).
Full table
Furthermore, analysis of subscales showed significant difference between men and women. Women as compared to men strongly agreed that life is meaningful even with stoma (76.5% vs. 23.5%), had accepted changes brought by stoma (73.3% vs. 26.7%) and felt life as worthwhile (60% vs. 40%). Majority of men however, felt that they had lost control over life (80% vs. 20%) and it’s uneasy to mix up with society (55.9% vs. 44.1%) and they were always conscious about stoma leakage, noise and smell (54.7% vs. 45.3%). However, less sexual attraction due to stoma was major concern of women than men (58.8% vs. 41.2%).
Additionally, the hierarchical regression analysis was done with subscales of psychosocial adjustment as dependent variable controlling for the effect of age, employment status and perceived family support. The analysis revealed that men significantly predicted low acceptance {β=−3.078, P=0.023, ΔR2=0.036, F [4,117] =7.90, P<0.001} and low social engagement score {β=−2.501, P<0.001, ΔR2=0.098, F [4,117] =6.03, P<0.001} as compared to women.
Predictors of psychosocial adjustment by gender
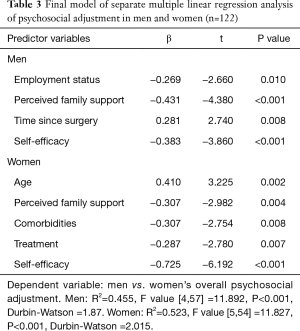
Subsequently, it was investigated whether men’s and women’s psychological adjustment respectively was determined differently by gender. To explore this, separate multiple regression analysis was carried out for men and women (Table 3).
Full table
Men’s lower psychosocial adjustment was predominantly explained by perceived lack of family support, total dependence on other for care of ostomy and to lesser extent by employment status. However, as time since ostomy surgery increased, men’s adjustment to ostomy also increased.
Similarly, women’s lower psychosocial adjustment was predominantly explained by total dependence on other for care of ostomy and to lesser extent by presence of comorbidity, treatment and perceived lack of family support. However, as women’s age increased, their psychosocial adjustment also increased. The employment status however showed no significant role in women compared with that of men.
Discussion
The present study highlights the psychosocial adjustment difference in men and women colorectal cancer survivors with ostomy. While men and women in this study were similar in various demographic and clinical aspects, there were some significant differences in the age, employment status and perceived family support.
Regarding the psychosocial adjustment, the result showed that both men and women had significant impairment in the psychosocial adjustment as reported in previous study (20). However, men had significantly lower psychosocial adjustment score than women, which is contrast to the findings reported by other studies (21,22).
More precisely, the analysis of subscales showed that men reported more negative emotions (loss of control over body, uneasy to mix up with society and consciousness of stoma leakage, noise and smell) than women. This should be interpreted considering the difference in the employment status between men and women in this study. Most of the men with ostomy were employed (69.4%) as compared to women. In addition to the reaction of family members and neighborhood, employed men expressed fear of social embarrassment and activity restriction as well. They expressed that they were more conscious about stoma leakage, smell or noise in the work than in home. Loss of control over body in the form of noise, smell and leakage could increase negative emotions and affect one’s self-identity and social role (2), especially when power and control are considered synonymous to male body. This is especially true in our cultural context, which in turn can lead to social isolation and adjustment problems. Furthermore, activities restriction and uneasiness to mix up with others may be defense in response to fear of other’s reaction to ostomy as suggested by Druss et al. (23).
Besides that, among the currently employed men with ostomy, 43.5% had changed occupation after formation of stoma. They expressed that ostomy interfered with the nature of their work, thus, they had to change their occupation. This might explain why men reported lower psychosocial adjustment as compared to women, where majority of women were unemployed and were living with family most of the time as compared to men.
Another possible explanation for lower adjustment in men may be the fact that men in this study perceived lower family support (80.8%) than women. Presence of family support can boost one’s acceptance, psychological wellbeing, confidence and adjustment as a whole. This is also supported by multiple studies conducted worldwide; where family support is associated with higher psychosocial adjustment in patients with ostomy (24-27). Accordingly, regression analysis also showed that lack of perceived family support as a significant predictor of lower psychosocial adjustment in both men and women respectively.
Moreover, most of the men were in the age group of ≥40 as compared to women. Hence, lower social engagement in men might be due to restriction in activities and increasing dependency related to age. A study conducted in Iran (28) also found that as compared to younger ostomy patients, persons older than 40 years of age had more psychological problems (OR =2.77). In line with this is the result of regression analysis which showed that low self-efficacy predicted lower psychosocial adjustment in both men and women.
Notably, even after controlling for effect of the possible confounders (age, employment status and perceived family support), the result of hierarchical regression analysis showed that men uniquely and significantly predicted lower acceptance and social engagement score.
Considering the multiple roles women have to play in our cultural context, we expected women to report more adjustment problems because of ostomy than men. In contrast to our expectation, women reported more positive emotions where, majority of the women had accepted stoma as their body part including the changes associated with it and had felt that it has given them new life. This is in line with the suggestion of Vlassoff, who argues that women accept their condition more than to see it as a challenge like their men counterparts do (15). Remarkably, acceptance is associated with better adjustment since those who fail to accept, experience poor interpersonal relationships and are less likely to report improvements in adjustment to stoma surgery (27). Thus, this may also explain why women had high psychosocial adjustment than men.
Still, less sexual attraction were major concerns for women than men in this study. Several factors likely account for this difference. Researchers collecting data were female nurses, and culturally, Nepalese men are less likely to discuss this topic with women. Thus this may have been a barrier for men to initiate conversation about sexual functioning. Nevertheless, threat to self-image and physical appearance brought by ostomy is mainly reported by women than men which could lead to the feeling of less sexual attraction (21).
Regarding the predictors of psychosocial adjustment in men and women, major predictors were almost similar between them. This signifies the importance of family support and self care efficacy to improve adjustment in both. This can have significant implications for health care providers.
Conclusions
Men and women colorectal cancer survivors with ostomy have remarkable psychosocial adjustment problems, however, they significantly vary in relation to acceptance, social engagement, emotions and sexuality. Notably, clinicians, nurses and enterostomal therapist should recognize the role of gender and should design and implement programs to aid adjustment taking gender differences into account.
Men should receive special attention in counseling to improve their acceptance and social engagement. Interaction programs with women ostomates could help to improve their view towards ostomy and to accept it as their body part. Sexuality and intimacy concerns should also be assessed regularly in ostomates, however, women needs special attention on this aspect during survivorship care.
Limitations
The main limitation of the study is its sample size, which has implication on generalization of the findings. Larger sample in further studies can validate our result. Due to the design of this study, causality cannot be determined. The study may not reflect overall picture of many colorectal cancer survivors with ostomy who have no access to stoma clinics.
Acknowledgements
We would like to thank Institutional Review Board of Tribhuvan University, Institute of Medicine, B.P. Koirala Memorial Cancer Hospital for providing an opportunity to conduct this study. Similarly, our sincere gratitude goes to Ms Kingsley L. Simmons for granting the permission to use Ostomy Adjustment Inventory. We owe our vote of thanks to all survivors with ostomy who participated in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by institutional ethics board of Tribhuvan University [No. 187(6-11-E)2/070/71] and written informed consent was obtained from all patients.
References
- American Cancer Society. Colorectal Cancer Facts & Figures 2014-2016. Available online: http://www.cancer.org/acs/groups/content/documents/document/acspc-042280.pdf
- Liao C, Qin Y. Factors associated with stoma quality of life among stoma patients. International Journal of Nursing Sciences 2014;1:196-201. [Crossref]
- Turns D. Psychosocial issues: pelvic exenterative surgery. J Surg Oncol 2001;76:224-36. [Crossref] [PubMed]
- Follick MJ, Smith TW, Turk DC. Psychosocial adjustment following ostomy. Health Psychol 1984;3:505-17. [Crossref] [PubMed]
- Zakri RH, Shah SA, Khaliq T, et al. Impact of ostomy surgery on hospitalized patients at a tertiary care hospital in Pakistan. Ann Pak Inst Med Sci 2010;6:36-9.
- Vonk-Klaassen SM, de Vocht HM, den Ouden ME, et al. Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res 2016;25:125-33. [Crossref] [PubMed]
- Salomé GM, de Almeida SA, Silveira MM. Quality of life and self-esteem of patients with intestinal stoma. Journal of Coloproctology 2014;34:231-9. [Crossref]
- Dabirian A, Yaghmaei F, Rassouli M, et al. Quality of life in ostomy patients: a qualitative study. Patient Prefer Adherence 2010;5:1-5. [PubMed]
- Ito N, Tanaka M, Kazuma K. Health-related quality of life among persons living in Japan with a permanent colostomy. J Wound Ostomy Continence Nurs 2005;32:178-83. [Crossref] [PubMed]
- Krouse R, Grant M, Ferrell B, et al. Quality of life outcomes in 599 cancer and non-cancer patients with colostomies. J Surg Res 2007;138:79-87. [Crossref] [PubMed]
- Popek S, Grant M, Gemmill R, et al. Overcoming challenges: life with an ostomy. Am J Surg 2010;200:640-5. [Crossref] [PubMed]
- Chan F, Cardoso ED, Chronister JA. editors. Understanding psychosocial adjustment to chronic illness and disability. New York: Springer publishing company, 2009.
- Bergerot CD, de Araujo TC, Troccoli BT. Assessment of Distress Among Chemotherapy Patients: A Comparative Study of Gender. Paidéia 2014;24:56-65.
- World Health Organization. Gender, 2016. Available online: http://www.who.int/gender-equity-rights/understanding/gender-definition/en/
- Vlassoff C. Gender differences in determinants and consequences of health and illness. J Health Popul Nutr 2007;25:47-61. [PubMed]
- Keller M, Henrich G. Illness-related distress: does it mean the same for men and women? Gender aspects in cancer patients’ distress and adjustment. Acta Oncol 1999;38:747-55. [Crossref] [PubMed]
- Fife BL, Kennedy VN, Robinson L. Gender and adjustment to cancer: clinical implications. J Psychosoc Oncol 1994;12:1-2. [Crossref]
- Baider L, Perez T, De-Nour AK. Gender and adjustment to chronic disease. A study of couples with colon cancer. Gen Hosp Psychiatry 1989;11:1-8. [Crossref] [PubMed]
- Simmons KL, Smith JA, Maekawa A. Development and psychometric evaluation of the Ostomy Adjustment Inventory-23. J Wound Ostomy Continence Nurs 2009;36:69-76. [Crossref] [PubMed]
- Cheng F, Meng AF, Yang LF, et al. The correlation between ostomy knowledge and self-care ability with psychosocial adjustment in Chinese patients with a permanent colostomy: a descriptive study. Ostomy Wound Manage 2013;59:35-8. [PubMed]
- Grant M, McMullen CK, Altschuler A, et al. Gender differences in quality of life among long-term colorectal cancer survivors with ostomies. Oncol Nurs Forum 2011;38:587-96. [Crossref] [PubMed]
- Krouse RS, Herrinton LJ, Grant M, et al. Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol 2009;27:4664-70. [Crossref] [PubMed]
- Druss RG, O’Connor JF, Stern LO. Psychologic response to colectomy. II. Adjustment to a permanent colostomy. Arch Gen Psychiatry 1969;20:419-27. [Crossref] [PubMed]
- Altschuler A, Ramirez M, Grant M, et al. The influence of husbands’ or male partners’ support on women’s psychosocial adjustment to having an ostomy resulting from colorectal cancer. J Wound Ostomy Continence Nurs 2009;36:299-305. [Crossref] [PubMed]
- Nichols TR. Social connectivity in those 24 months or less postsurgery. J Wound Ostomy Continence Nurs 2011;38:63-8. [Crossref] [PubMed]
- Piwonka MA, Merino JM. A multidimensional modeling of predictors influencing the adjustment to a colostomy. J Wound Ostomy Continence Nurs 1999;26:298-305. [PubMed]
- Simmons KL, Smith JA, Bobb KA, et al. Adjustment to colostomy: stoma acceptance, stoma care self-efficacy and interpersonal relationships. J Adv Nurs 2007;60:627-35. [Crossref] [PubMed]
- Mahjoubi B, Moghimi A, Mirzaei R, et al. Evaluation of the end colostomy complications and the risk factors influencing them in Iranian patients. Colorectal Dis 2005;7:582-7. [Crossref] [PubMed]