Radiographic and endoscopic regression of metastatic gastric cancer to the colon in the setting of 5-aminosalicylic acid use
Introduction
Gastric cancer is the third leading cause of cancer-related death worldwide and presents a major public health issue (1). Signet ring cell gastric cancer comprises around 35−45% of all gastric cancer, and is increasing in incidence (2,3). Advanced stages of this disease may result in multiple organ involvement, though metastasis to the colon is very rare and sparsely reported. We present a case report of metastatic signet ring cell gastric adenocarcinoma to the colon diagnosed by serial colonoscopic biopsies with regressing computer tomography (CT) imaging and endoscopic findings in the setting of 5-aminosalicylic acid (5-ASA) use.
Case presentation
A 59-year-old Caucasian female presented to the outpatient GI clinic for consultation given recurrent complaints of nausea, vomiting, vague abdominal cramping, loose stools, and subjective fevers lasting up to 5 days at a time over the past 3−4 months. She provided a report from a recent CT abdomen/pelvis with IV/PO contrast suggestive of an apple-core lesion of the ascending colon, with a second area of focal wall thickening involving the hepatic flexure. She had a past medical history of cholecystectomy, cesarean section, and a previous 7-pack year smoking history. She denied any family history of GI-related cancer or disease. Medications included calcium/vitamin D and multivitamin, and recent additions of omeprazole and ondansetron by her primary care provider. Review of systems were negative for GI bleeding though notable for a 15−20 lbs unintentional weight loss over the past few years. She had never undergone an upper endoscopy and reported a normal colonoscopy 3 years prior.
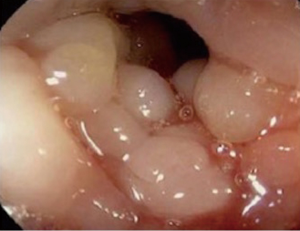
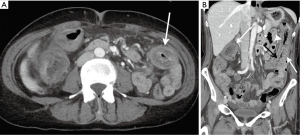
Colonoscopy was performed and was notable for sigmoid diverticulosis and a severe stenosis 40 cm proximal to the anus that was unable to be traversed with an adult gastroscope or pediatric colonoscope (Figure 1). Mucosa at the site appeared thickened and nodular; no ulcerated tissue was seen and mucosal integrity appeared preserved. The area was tattooed and biopsies were taken which revealed mild acute and chronic inflammation without evidence of dysplasia or carcinoma. CT abdomen/pelvis with IV contrast was subsequently performed within the next month and showed diffuse wall thickening and mucosal hyperenhancement involving the ascending, transverse, and descending colon with minimal mesenteric or retroperitoneal lymphadenopathy and patent mesenteric vasculature consistent with colitis, though no apple-core lesion (Figure 2). Stool cultures, examination for ova & parasites, clostridium difficile toxin assay, and fecal leukocyte assay were ordered and resulted negative. The clinical decision was made to start her on mesalamine, which she tolerated with mild improvement of symptoms and stabilization of her weight after 2 months. Repeat CT abdomen/pelvis with IV contrast was performed and re-demonstrated mucosal thickening involving the ascending colon and transverse colon, though substantially less marked.
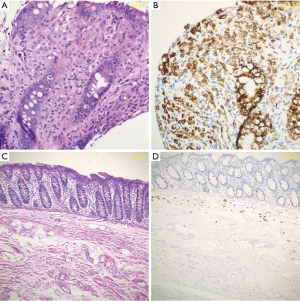
Because of continued clinical concern, ambiguity in diagnosis, and persistent dyspepsia, repeat colonoscopy and upper endoscopy was performed which showed benign-appearing intrinsic mild stenoses in the sigmoid, transverse, and ascending colon with normal appearing mucosa (Figure 3). Colonoscopy was completed to the terminal ileum. Endoscopic examination of the upper GI tract showed erythematous and cobblestoned appearance in the gastric fundus and body, and normal appearing duodenum and esophagus. Biopsies revealed primary signet ring cell adenocarcinoma of the stomach and metastatic signet ring cell adenocarcinoma of the ascending colon (Figure 4A,B). She was seen by Oncology and Surgery and underwent a PET-CT that showed no further metastases. A diagnostic abdominal laparoscopy with peritoneal washings was negative. She was initiated on FOLFOX chemotherapy followed by successful total gastrectomy and right hemicolectomy. The stomach contained signet ring cell carcinoma with full-thickness gastric wall involvement (from mucosa to serosa) and metastatic carcinoma in one gastric lymph node. The colectomy specimen revealed metastatic signet ring cell carcinoma involving the colon (Figure 4C,D), mesentery and mesoappendix. The metastatic carcinoma also involved the full-thickness of colonic wall, and presented in six colonic lymph nodes. She is continuing FOLFOX chemotherapy at the time of this report with most recent CT scan 1 month after surgery showing no evidence of recurrent or metastatic disease.
Discussion
Colonic metastases are generally a rare occurrence, though post-mortem studies suggest a higher incidence than expected (4). The most common route of metastatic occurrence to the bowel is from peritoneal seeding typical of ovarian carcinoma, though hematogenous dissemination to the colon has also been described in breast carcinoma, lung carcinoma, and melanoma (5-8). Colonic metastases from gastric cancer have been rarely reported (4,9-11). This unusual phenomenon has typically been associated with Lauren’s diffuse type histology and linitis plastica with a hematogenous dissemination route of metastasis, though a peritoneal route has also been described (4,11). A retrospective study of intestinal metastasis from gastric adenocarcinoma noted 21 patients with metastasis to the colon, rectum, or appendix. Of these, six cases (29%) showed poorly differentiated adenocarcinoma with signet ring cell features and five (24%) showed signet ring cell gastric adenocarcinoma (4). The majority of these patients (82%) had linitis plastica, which was also found in our case upon surgical removal. Linitis plastica of the stomach can be identified on CT scan by diffuse thickening and a narrowed lumen, though these features were interestingly not observed on serial CT scans in our patient. The majority of the rare cases of colonic metastases from gastric cancer show long circumferential involvement, multiplicity, and an inner layer with distinct enhancement and thickening reminiscent of a “target” pattern (4). Though bowel wall thickening itself is nonspecific and may represent an inflammatory, infectious, or ischemic process, the distinct pattern of inner layer enhancement is peculiar and may represent a hallmark of metastatic signet ring cell adenocarcinoma (4). Interestingly, in our patient CT findings of the colon appeared regressive, with initial findings of an apple-core lesion to later scans demonstrating diminishing degrees of pancolonic wall thickening with mucosal hyperenhancement. This correlated with experience on serial colonoscopy, with the first colonoscopy attempt noting a tight nodular non-traversable stricture and the second noting mild benign-appearing stenoses throughout the colon that were easily traversable. This is unusual, as sparse evidence regarding the radiological evolution of colon metastases show progression as would be expected clinically with the evolution of this cancer over time. We hypothesize that this pattern of regression may be due in some degree to waxing and waning edema in the setting of lymphatic involvement, and perhaps also because of mesalamine use, a 5-ASA compound. 5-ASA medications are a common drug class used for maintenance of remission in inflammatory bowel disease (IBD), mainly ulcerative colitis, and epidemiological studies suggest that long-term consumption decreases the colon cancer risk for these patients (12,13). Furthermore, 5-ASA compounds have been demonstrated to have pro-apopotic and anti-proliferative effects on several cancer-derived cell lines through a multitude of mechanisms including EGFR activation, COX-2 expression, and inhibition of Wnt/β-catenin pathway (14-18). Though no studies in the literature exist on the impact of 5-ASA compounds on gastric adenocarcinoma cell lines, it may be possible that similar anti-tumor and anti-inflammatory effects played a role in the evolution of findings in our patient.
Our case also illustrates the difficulty in colonoscopic mucosal biopsies in relaying a positive result as metastatic carcinoma is often deep in the wall, leading to a false negative result in up to 54% of cases (4). Even with a deeper tunneled biopsy specimen, the scarcity and deceivingly bland morphology of tumor cells may hinder detection (4). The colectomy specimen in our case revealed very limited mucosal involvement, with carcinoma cells predominantly present in submucosa and deeper portion of the colonic wall, consistent with the metastatic/implantation nature of the disease (Figure 4C,D). As our case demonstrated, the clinician should be hyper-vigilant in pursuing a diagnosis and consider repeat endoscopic evaluation as a case evolves.
Acknowledgements
Funding: This work was supported by the National institutes of Health (5T32DK007568-25 to Yuval A. Patel).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359-86. [Crossref] [PubMed]
- Bamboat ZM, Tang LH, Vinuela E, et al. Stage-stratified prognosis of signet ring cell histology in patients undergoing curative resection for gastric adenocarcinoma. Ann Surg Oncol 2014;21:1678-85. [Crossref] [PubMed]
- Taghavi S, Jayarajan SN, Davey A, et al. Prognostic significance of signet ring gastric cancer. J Clin Oncol 2012;30:3493-8. [Crossref] [PubMed]
- Jang HJ, Lim HK, Kim HS, et al. Intestinal metastases from gastric adenocarcinoma: helical CT findings. J Comput Assist Tomogr 2001;25:61-7. [Crossref] [PubMed]
- Feczko PJ, Collins DD, Mezwa DG. Metastatic disease involving the gastrointestinal tract. Radiol Clin North Am 1993;31:1359-73. [PubMed]
- Taal BG, den Hartog Jager FC, Steinmetz R, et al. The spectrum of gastrointestinal metastases of breast carcinoma: II. The colon and rectum. Gastrointest Endosc 1992;38:136-41. [Crossref] [PubMed]
- Eyres KS, Sainsbury JR. Large bowel obstruction due to metastatic breast cancer: an unusual presentation of recurrent disease. Br J Clin Pract 1990;44:333-4. [PubMed]
- Reintgen DS, Thompson W, Garbutt J, et al. Radiologic, endoscopic, and surgical considerations of melanoma metastatic to the gastrointestinal tract. Surgery 1984;95:635-9. [PubMed]
- Pace U, Contino G, Chiappa A, et al. Metachronous Colon Metastases from Gastric Adenocarcinoma: A Case Report. Case Rep Oncol 2009;2:92-6. [Crossref] [PubMed]
- Lee HC, Yang MT, Lin KY, et al. Metastases from gastric carcinoma to colon in the form of multiple flat elevated lesions: a case report. Kaohsiung J Med Sci 2004;20:552-7. [Crossref] [PubMed]
- Fisher ER, Brown CH. Linitis plastica carcinoma of the stomach with extensive metastases simulating a colonic lesion. Gastroenterology 1952;20:503-8. [PubMed]
- Rubin DT, LoSavio A, Yadron N, et al. Aminosalicylate therapy in the prevention of dysplasia and colorectal cancer in ulcerative colitis. Clin Gastroenterol Hepatol 2006;4:1346-50. [Crossref] [PubMed]
- Eaden J. Review article: the data supporting a role for aminosalicylates in the chemoprevention of colorectal cancer in patients with inflammatory bowel disease. Aliment Pharmacol Ther 2003;18 Suppl 2:15-21. [Crossref] [PubMed]
- Bos CL, Diks SH, Hardwick JC, et al. Protein phosphatase 2A is required for mesalazine-dependent inhibition of Wnt/beta-catenin pathway activity. Carcinogenesis 2006;27:2371-82. [Crossref] [PubMed]
- Svrcek M, Cosnes J, Tiret E, et al. Expression of epidermal growth factor receptor (EGFR) is frequent in inflammatory bowel disease (IBD)-associated intestinal cancer. Virchows Arch 2007;450:243-4. [Crossref] [PubMed]
- Spano JP, Lagorce C, Atlan D, et al. Impact of EGFR expression on colorectal cancer patient prognosis and survival. Ann Oncol 2005;16:102-8. [Crossref] [PubMed]
- Monteleone G, Franchi L, Fina D, et al. Silencing of SH-PTP2 defines a crucial role in the inactivation of epidermal growth factor receptor by 5-aminosalicylic acid in colon cancer cells. Cell Death Differ 2006;13:202-11. [Crossref] [PubMed]
- Stolfi C, Fina D, Caruso R, et al. Cyclooxygenase-2-dependent and -independent inhibition of proliferation of colon cancer cells by 5-aminosalicylic acid. Biochem Pharmacol 2008;75:668-76. [Crossref] [PubMed]