Selective extra levator versus conventional abdomino perineal resection: experience from a tertiary-care center
Introduction
With a growing economy, the incidence of rectal cancer in India is on the rise, with an estimated age standardized rate of 4.3 and 3.5 per 100,000 in male and female subjects, respectively (1). Currently, the standard curative treatment for rectal cancer consists of radical surgery with total or partial tumor-specific mesorectal excision depending on the tumor location. Locally advanced tumors have better loco regional control with the use of neoadjuvant chemo radiotherapy, followed by surgery (2). Despite an increasing trend towards sphincter-saving surgery for low rectal cancer, abdominoperineal resection (APER) is still the commonly performed with reported rates of end stoma of upto 12–30% (3).
Studies have shown that local recurrence rates are higher and overall prognosis is worse for patients with rectal cancer who require APER as compared to those who require anterior resection (4-6). Studies further suggest the possibility of tumor-specific factors being responsible for these adverse outcomes rather than the procedure itself (7). Circumferential resection margin (CRM) positivity is the single most important factor predicting local recurrence and overall prognosis after rectal cancer surgery (8). With conventional APER, CRM positivity rate has ranged between 12% and 15.7% (9,10). One possible explanation for this high rate of CRM positivity is the thinning of the mesorectum distally where the tumor tends to abut the levator complex. This is still more significant for anteriorly located tumors where the mesorectum is virtually nonexistent. This has encouraged the surgeons to reevaluate the current technique and further modify the surgical approach so as to achieve a wider CRM.
Holm et al. (11) first described the extralevator APER (ELAPER), which closely resembles the original procedure of APER described by Miles (11). It involves an en bloc resection of the rectum and anal canal along with the entire levator muscle without dissecting the mesorectum from the levator muscles so as to resect the levator muscle at its origin from the arcuate line on the obturator internus muscle. This procedure aims to create a cylindrical specimen without a “waist” so as to reduce the rate of intra operative tumor perforation and CRM positivity. Studies comparing APER with ELAPER have yielded conflicting results (12-15). There is only one randomized control trial that found a lower rate of local recurrence without an increase in complications with ELAPER (16). Two systematic reviews on the issue have shown differing results (14,17). With the inception of a dedicated colorectal unit at our institute, ELAPER has been offered to the patients although with less-stringent selection criteria.
Aims and objectives
To compare ELAPER with conventional APER in terms of short-term oncological and clinical outcomes.
Methods
This is a retrospective review of a prospectively maintained database in the Division of Colorectal Surgery at the Tata Memorial Center, Mumbai, India. All patients undergoing an APER between July 1, 2013, and January 31, 2015, were included in the study. A comparative analysis was performed between those who underwent conventional APER and ELAPER.
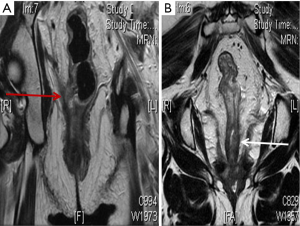
Following a detailed history and physical examination, all patients underwent a complete colonoscopy with biopsy and determination of serum carcinoembryonic antigen (CEA) levels. Loco regional staging was achieved with a baseline magnetic resonance imaging (MRI) of the pelvis (MRI 1). Contrast-enhanced computed tomography (CECT) of the thorax and abdomen were performed to rule out metastatic disease. Neoadjuvant chemo radiotherapy (NACTRT) was administered to all patients with a threatened CRM and/or enlarged mesorectal nodes on preoperative MRI. All treatment decisions were taken by a multidisciplinary team (MDT), comprising a colorectal surgeon, a radiation oncologist, a gastroenterologist, and a radiologist. NACTRT consisted of 50 Gy in 25 fractions for 5 weeks along with concurrent oral capecitabine (850 mg/m2 twice a day from days 1 to 14 and 22 to 35). Patients receiving NACTRT were evaluated for response with a second MRI of the pelvis (MRI 2) after 6-10 weeks of completion of neoadjuvant therapy, just before definitive surgery. The decision to perform ELAPER was individualized and was based mainly on the extent of levator muscle involvement, bulk of the tumor, the closeness of the tumor to CRM on MRI, and on the subjective judgment of the MDT (Figure 1A,B). Young male subjects with the involvement of prostate on MRI underwent either pelvic exenteration or ELAPER with shaving off the tumor from prostate depending on the extent of prostatic involvement and after discussion with the patient.
Technique of ELAPER
After an initial exploration of abdomen and pelvis to ensure the absence of liver and peritoneal metastasis, the mesorectum is mobilized till the origin of levator muscle circumferentially. This roughly corresponds to the sacrococcygeal joint posteriorly, the ischial spines laterally, and the seminal vesicles anteriorly. The inferior mesenteric pedicle is divided, the end sigmoid stoma created, and the abdomen closed. The patient is then placed in prone position and an extended perineal dissection performed, which encompasses an en bloc resection of the sphincter complex and the levator muscles from their origin on the pelvic sidewall. The coccyx is removed in continuity with the main specimen to facilitate access and ensure a negative CRM for posteriorly based tumors. Anteriorly, if the CRM is found to be threatened, a portion of prostate or vaginal wall is also removed. The resultant perineal defect is closed primarily in layers only if a tension-free closure is possible. Otherwise, some form of plastic reconstruction is adopted in the form of a V-Y advancement flap or gracilis flap with or without biological mesh placement.
Short-term oncological parameters evaluated included CRM positivity, tumor site perforation, and number of nodes harvested. Peri operative outcomes included blood loss, length of hospital stay, postoperative perineal wound complications, and 30-day mortality. Statistical analysis was performed using SPSS software, version 18.0 (SPSS, Chicago, IL, USA). The χ2-test or Fisher’s exact test, as appropriate, was used for univariate analysis.
Results
There were 120 APERS performed between July 1, 2013, and January 31, 2015, and all were included in the analysis. There were 42 cases of ELAPER and 78 cases of conventional APER. The baseline patient characteristics are shown in Table 1. The two groups were comparable in all the parameters except levator involvement. Levator involvement was significantly higher in the ELAPER compared with conventional group (P=0.000). ELAPER was offered to female patients less often than male subjects although it did not reach statistical significance. Among the 46 patients who underwent laparoscopic surgery in both the groups, there was no conversion to open surgery in any of the patients.
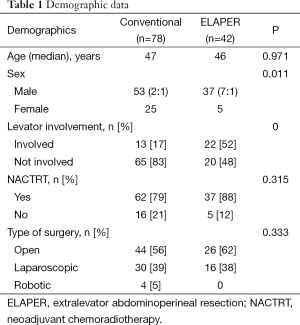
Full table
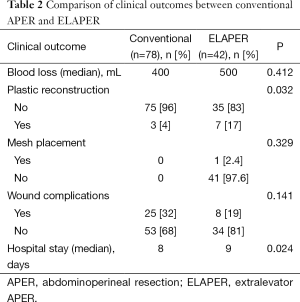
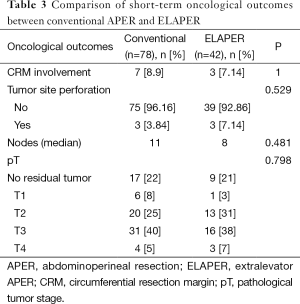
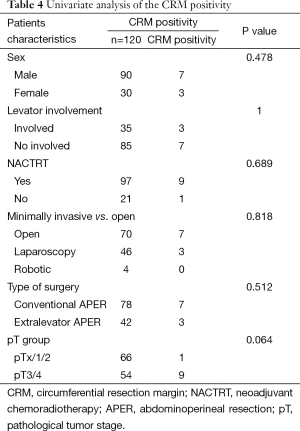
Clinical and oncological outcomes are shown in Tables 2 and 3, respectively. Although the median blood loss was higher, it did not reach statistical significance. Plastic reconstruction was required in significantly higher proportion of patients in the ELAPER group. Plastic reconstruction was in the form of V-Y advancement flap or gluteal flap in majority of the patients. Median hospital stay was significantly longer in ELAPER group compared with conventional group (P=0.024). CRM involvement was seen in seven patients (8.9%) in the conventional group compared with three patients (7.14%) in the ELAPER group. Tumor site perforation was seen in three patients (3.84%) in both the conventional group and the ELAPER group (7.14%). Difference between the two groups in terms of CRM positivity and tumor site perforation did not reach statistical significance. Although perineal wound complications, including wound infection and wound dehiscence, were higher in the conventional group compared with ELAPER, the difference did not reach statistical significance. Two patients in each group required major flap reconstruction for the perineal wound dehiscence. There were no cases of perineal hernia in either group. Univariate analysis of the various factors (Table 4) contributing to CRM involvement was performed although none of them significantly influenced CRM involvement.
Full table
Full table
Full table
Discussion
APER is the standard of care for low rectal cancers for many years. Despite advances in the management of rectal cancers including routine local staging with MRI pelvis, NACTRT for locally advanced disease and total mesorectal excision, outcomes of APER have remained suboptimal when compared with anterior resection (6). These outcomes were reflected with high CRM involvement (49.6%) and intra operative perforation rates (28.2%) even in specialized centers. Holm et al. (11) advocated a prone approach with gluteus maximus flap for APER with good oncological outcomes. Following this, multi centric studies compared results of ELAPER against conventional APER and found good outcomes with ELAPER (18). The major drawback of majority of these studies was that it was a historical comparison. As a result, improved outcomes might have been accounted for by changes in staging and treatment strategies rather than the surgery itself. This theory is further strengthened by the fact that many of the well-known centers across the world have shown quite good results with conventional APER (19).
ELAPER is not widely practiced in India, with no case series published in English literature. With the inception of dedicated colorectal unit at our institute, ELAPER was introduced for advanced tumors with either involvement of levators or proximity to prostate. ELAPER could not be offered to some patients owing to time constrains (as change of position leads to extra operative time) and concerns from the anesthesiologists.
In this study, despite higher proportion of patients with levator involvement (52% vs. 17% for ELAPER vs. conventional APER, respectively), ELAPER led to lower rates of CRM involvement compared with conventional APER in patients with low rectal cancer, although on univariate analysis, it did not reach statistical significance (Table 4). Rates of intra operative tumor site perforation were comparable between the two groups. Reported rates of CRM involvement and tumor site perforation in literature for APER are 11–52% and 10–19%, respectively. Those for ELAPER are 7–17% and 3.5–13%, respectively. Studies comparing these two surgical techniques are divided, with some of them clearly showing the superiority of ELAPER over APER for CRM involvement (13,15), whereas others having failed to demonstrate the same (12,20–22). Only one randomized trial did show significantly lower rates of local recurrence with ELAPER. But, it was a small study (n=67) and less than 30% of the patients received neoadjuvant treatment which is the standard of care at present (16). Owing to these issues, it cannot be considered as a robust evidence. Stelzner et al. (14) performed a systematic review of 1,097 patients comparing ELAPER with APER and found that rates of CRM involvement, tumor site perforation, and local recurrence were significantly lesser with ELAPER. In contrast, Krishna et al. (17) performed a similar review and questioned the role of ELAPER. In this study, the rates of CRM involvement were lower in both the groups compared with the reported series. This is the result of high volumes of rectal cancers at our center, standardization of the operative technique, and supervision of the perineal part of the surgeries by the two senior surgeons.
In this study, the need for flap reconstruction was higher with ELAPER compared with conventional, which is consistent with the literature APER (22). The rates of perineal wound complications were not significantly higher with ELAPER compared with conventional APER owing to better case selection with more liberal use of plastic reconstruction whenever tight primary closure was anticipated and expertise of plastic surgery team at our institute. Although the use of biological mesh in pelvic floor repair is advocated for reducing the incidence of perineal hernia, it was not used routinely as a result of higher cost and difficulty in procurement (23).
ELAPER is being looked upon as a better way of performing APER for low rectal cancers. LOREC project looked at training radiologist, surgeons, and pathologists using the cadaver models (24). Extent of levator involvement is the single most important factor in deciding the approach. We compared two groups of patients and found higher CRM involvement in patients undergoing conventional APER. In spite of smaller comparison groups, fewer numbers of events in both the groups and a possible selection bias in this study, ELAPER appears to be oncologically superior for tumors involving levators. Only a well-conducted prospective randomized trial comparing ELAPER with conventional APER can solve this dilemma.
Conclusions
ELAPER should be the preferred approach for low rectal tumors with involvement of levators. For those cases in which levators are not involved, as shown in preoperative MRI, the current evidence is insufficient to recommend ELAPER over conventional APER. This stresses the importance of preoperative MRI in determining the best approach for an individual patient. Time is right for a randomized trial comparing the results of ELAPER with conventional APER in this subgroup of patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- GLOBOCAN 2012. Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012. Lyon: IARC, 2012.
- van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011;12:575-82. [Crossref] [PubMed]
- Chau A, Maggiori L, Debove C, et al. Toward the end of abdominoperineal resection for rectal cancer? An 8-year experience in 189 consecutive patients with low rectal cancer. Ann Surg 2014;260:801-5; discussion 805-6. [Crossref] [PubMed]
- How P, Shihab O, Tekkis P, et al. A systematic review of cancer related patient outcomes after anterior resection and abdominoperineal excision for rectal cancer in the total mesorectal excision era. Surg Oncol 2011;20:e149-55. [Crossref] [PubMed]
- Shihab OC, Brown G, Daniels IR, et al. Patients with low rectal cancer treated by abdominoperineal excision have worse tumors and higher involved margin rates compared with patients treated by anterior resection. Dis Colon Rectum 2010;53:53-6. [Crossref] [PubMed]
- den Dulk M, Putter H, Collette L, et al. The abdominoperineal resection itself is associated with an adverse outcome: the European experience based on a pooled analysis of five European randomised clinical trials on rectal cancer. Eur J Cancer 2009;45:1175-83. [Crossref] [PubMed]
- Anderin C, Martling A, Hellborg H, et al. A population-based study on outcome in relation to the type of resection in low rectal cancer. Dis Colon Rectum 2010;53:753-60. [Crossref] [PubMed]
- Kelly SB, Mills SJ, Bradburn DM, et al. Effect of the circumferential resection margin on survival following rectal cancer surgery. Br J Surg 2011;98:573-81. [Crossref] [PubMed]
- Messenger DE, Cohen Z, Kirsch R, et al. Favorable pathologic and long-term outcomes from the conventional approach to abdominoperineal resection. Dis Colon Rectum 2011;54:793-802. [Crossref] [PubMed]
- Wibe A, Syse A, Andersen E, et al. Oncological outcomes after total mesorectal excision for cure for cancer of the lower rectum: anterior vs. abdominoperineal resection. Dis Colon Rectum 2004;47:48-58. [Crossref] [PubMed]
- Holm T, Ljung A, Haggmark T, et al. Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg 2007;94:232-8. [Crossref] [PubMed]
- Asplund D, Haglind E, Angenete E. Outcome of extralevator abdominoperineal excision compared with standard surgery: results from a single centre. Colorectal Dis 2012;14:1191-6. [Crossref] [PubMed]
- Stelzner S, Hellmich G, Schubert C, et al. Short-term outcome of extra-levator abdominoperineal excision for rectal cancer. Int J Colorectal Dis 2011;26:919-25. [Crossref] [PubMed]
- Stelzner S, Koehler C, Stelzer J, et al. Extended abdominoperineal excision vs. standard abdominoperineal excision in rectal cancer—a systematic overview. Int J Colorectal Dis 2011;26:1227-40. [Crossref] [PubMed]
- West NP, Finan PJ, Anderin C, et al. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol 2008;26:3517-22. [Crossref] [PubMed]
- Han JG, Wang ZJ, Wei GH, et al. Randomized clinical trial of conventional versus cylindrical abdominoperineal resection for locally advanced lower rectal cancer. Am J Surg 2012;204:274-82. [Crossref] [PubMed]
- Krishna A, Rickard MJ, Keshava A, et al. A comparison of published rates of resection margin involvement and intra-operative perforation between standard and ‘cylindrical’ abdominoperineal excision for low rectal cancer. Colorectal Dis 2013;15:57-65. [Crossref] [PubMed]
- West NP, Anderin C, Smith KJ, et al. Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg 2010;97:588-99. [Crossref] [PubMed]
- Davies M, Harris D, Hirst G, et al. Local recurrence after abdomino-perineal resection. Colorectal Dis 2009;11:39-43. [Crossref] [PubMed]
- Klein M, Fischer A, Rosenberg J, et al. Extralevatory abdominoperineal excision (ELAPE) does not result in reduced rate of tumor perforation or rate of positive circumferential resection margin: anationwide database study. Ann Surg 2015;261:933-8. [Crossref] [PubMed]
- Ortiz H, Ciga MA, Armendariz P, et al. Multicentre propensity score-matched analysis of conventional versus extended abdominoperineal excision for low rectal cancer. Br J Surg 2014;101:874-82. [Crossref] [PubMed]
- Prytz M, Angenete E, Ekelund J, et al. Extralevator abdominoperineal excision (ELAPE) for rectal cancer—short-term results from the Swedish Colorectal Cancer Registry. Selective use of ELAPE warranted. Int J Colorectal Dis 2014;29:981-7. [Crossref] [PubMed]
- Peacock O, Simpson JA, Tou SI, et al. Outcomes after biological mesh reconstruction of the pelvic floor following extra-levator abdominoperineal excision of rectum (APER). Tech Coloproctol 2014;18:571-7. [Crossref] [PubMed]
- Moran BJ, Holm T, Brannagan G, et al. The English national low rectal cancer development programme: key messages and future perspectives. Colorectal Dis 2014;16:173-8. [Crossref] [PubMed]


