Patient and caregiver awareness of pancreatic cancer treatments and clinical trials
Introduction
Although pancreatic cancer is the 11th most common cancer type in the United States, it ranks as the fourth leading cause of cancer-related mortality (1). By 2030, pancreatic cancer is expected to be the second leading cause of cancer-related death in the United States (2). In addition, the 5-year overall survival rate for patients diagnosed with pancreatic cancer at any stage is just 7% (1). Although these statistics are illustrative of a poor prognosis, recent advances in pancreatic cancer treatment options hold promise in improving outcomes for patients. The large number of active clinical trials suggests an intense interest in further advancing pancreatic cancer treatment. In addition to these developments, patients may also gain hope from support provided by caregivers and patient advocacy groups.
For pancreatic cancer, treatment options are highly specific to cancer stage (3,4), and each treatment is associated with a unique toxicity profile. For patients with metastatic disease, systemic chemotherapy regimens—such as gemcitabine alone, nab-paclitaxel plus gemcitabine, and FOLFIRINOX (leucovorin, 5-fluorouracil, irinotecan, and oxaliplatin)—are standard options (3). Both nab-paclitaxel plus gemcitabine and FOLFIRINOX have demonstrated significant efficacy advantages over gemcitabine alone in phase III trials; however, gemcitabine remains a recommended treatment for patients with poorer performance status (3,5,6). Treatment options for patients with locally advanced disease are generally the same as those for patients with metastatic disease, except that radiation therapy may be added. The standard treatment for resectable disease is surgery followed by chemotherapy with or without radiation (adjuvant therapy). However, preoperative (neoadjuvant) treatment may be used for some patients with resectable disease. Neoadjuvant therapy options are generally similar to those for adjuvant therapy (3,4). The most common side effects of standard chemotherapy options are bone marrow suppression, fatigue, vomiting, diarrhea, peripheral neuropathy, and elevated liver enzymes (3,5,6). The most common side effects of surgery are postsurgical complications, such as infection, pancreatic anastomotic leaks, or delayed gastric emptying (3,7). Lastly, the most common side effects of radiation are bone marrow suppression, liver dysfunction, vomiting, and nausea (8,9).
Current US treatment guidelines recommend that patients with pancreatic cancer participate in clinical trials (3). However, only 4.6% of US patients with pancreatic cancer actually enroll in trials (10). This does not appear to be due to a lack of clinical trials, as trials that were open in 2011 enrolled an average of 15% of their total target accrual (10). A more likely explanation may be a lack of communication about clinical trials—one publication on a study of 7,887 patients with solid tumors specified that only 14% of patients reported having discussed trial participation (11). Most patients in that study who did learn about trials did so from their physicians, and the 287 patients who went on to participate in trials included 3.6% of all patients and 26% of patients who had discussions about trials.
The Pancreatic Cancer Action Network designed a survey and distributed it to patients and caregivers to gauge their perceptions about a number of factors related to living with pancreatic cancer (12). Among the key findings in that study was the average of 2.4 months reported from the time of symptom onset to diagnosis. The survey also provided insight into the important role that caregivers play in the lives of patients diagnosed with pancreatic cancer. The most common caregiving roles included providing support on treatment days, updating family members and friends on the current state of the patient’s disease, communicating with physicians, and arranging and taking notes on medical appointments. Furthermore, caregivers are often involved in decisions about pancreatic cancer treatment.
The focus of this study was to analyze the survey results for information on patient and caregiver perceptions about treatment and enrollment in clinical trials, with the ultimate goal of uncovering possibilities to improve care and increase patient participation in trials.
Methods
The Pancreatic Cancer Action Network prepared a 25-minute survey of 70 questions that could be self-administered online (through funding by Celgene Corporation and described previously) (12). Surveys were completed between July 30, 2013, and September 18, 2013. All data were tested for statistical significance by the appropriate z or t-test at a confidence level of 95%, and results were reported on an unweighted basis. Demographic information on respondents was reported previously. Briefly, respondents included 184 patients and 213 caregivers in the United States (mean age, 50.6 years), and most respondents were female (80%) and white (90%). Most of the patients who completed the survey (79.9%) reported having a primary caregiver, usually a spouse or significant other (77.6%). Note that the caregivers who completed the survey were not necessarily caring for the patients who completed the survey.
Results
Patient and caregiver goals
When participants were asked to rank their top three concerns 1-2-3 at the time of the survey, the answers most frequently given were quality of life (70.7% for patients and 88.3% for caregivers), extending life (64.7% for patients and 69.5% for caregivers), and managing symptoms (32.6% for patients and 67.6% for caregivers).
Treatment options
According to the respondents, 30% of diagnosing physicians offered the patient treatment options at diagnosis. In cases in which the treatment options were not discussed at diagnosis, 44.4% of survey respondents indicated that treatment options were discussed within 1 week of diagnosis; conversely, 20.4% of respondents replied that the diagnosing physicians never discussed treatment options (Figure 1A). Most respondents (88.5%) stated that when treatment options were discussed (not specific to diagnosing physicians), the physician recommended a specific type of therapy, such as chemotherapy, surgery, or radiation. More than 80% of respondents reported the use of chemotherapy; surgery and radiation were also frequently reported (Figure 1B).

Following treatment recommendations
The vast majority of respondents (94.9%) reported that the patient followed the physician’s treatment recommendation. The reasons most often given for following the doctor’s recommendation were that the respondent trusted the doctor, to live as long as possible, it was the best/most realistic option, and it was the only option or there was a lack of options (Figure 2A). The top two reasons given for not receiving any therapy were that the doctor said nothing could be done (42.1%) and that the patient did not think therapy would help (36.8%).

Treatment side effects
The most common side effects of any treatment (surgery, radiation, drugs) were listed as fatigue (85.6%), loss of appetite (74.7%), and nausea/vomiting (67.4%). The side effects from these treatments that were most commonly described as extremely or very bothersome were pain (70.1%), fatigue (66.7%), and abdominal pain or cramping (66.4%). Participants also reported seeking or receiving treatment for the following conditions associated with pancreatic cancer: pain (54.9%), fatigue (38.3%), and weight loss (34.8%).
Clinical trials
Almost half of study participants (49.1%) reported that they or their loved one had never discussed clinical trials with their physician. Approximately one-quarter of respondents (23.7%) replied that the patient had discussed clinical trials with his or her physician at the time of diagnosis or before receiving his or her first treatment, and just 4.0% reported discussing trials after the first treatment did not work. In cases in which trials were discussed, oncologists were most commonly cited as the first to mention the possibility of clinical trial participation, followed by caregivers and patients (Figure 2B). In cases in which patients actually participated in clinical trials (11.6%), physicians were listed as the most common primary source of trial information (80.4%), followed by patients or caregivers (8.7%) and the Pancreatic Cancer Action Network (4.3%).
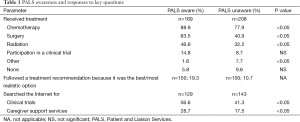
Patient Central
The Pancreatic Cancer Action Network offers a support and education service called Patient Central [referred to as the Patient and Liaison Services (PALS) program at the time of the survey]. Patient Central is a call-in information service available to the pancreatic cancer community. Approximately half of survey respondents indicated that they were aware of the PALS program (53.3% of patients and 42.7% of caregivers). A higher proportion of PALS aware respondents than PALS unaware respondents reported receiving treatment, following a recommendation because it was the best/most realistic option, and searching the Internet for information on clinical trials (Table 1). PALS aware respondents also more often reported participation of the patient in a clinical trial than PALS unaware respondents, although this difference was not statistically significant (14.8% vs. 8.7%; P= not significant).
Full table
Discussion
The results of this study provide real-world insight on the experience of patients and caregivers in learning about treatment options for pancreatic cancer. Although the list of treatment options for patients with pancreatic cancer continues to grow (3,4), a large proportion of respondents to this survey indicated a lack of discussion about possible treatments with their physicians. This is particularly concerning because approximately 95% of survey respondents reported that patients followed their physicians’ recommendations.
Of the respondents who stated that the patient did not receive treatment, more than 40% explained that the reason for this lack of treatment was that the physician said that nothing could be done. Although this is a reasonable approach in some situations, a separate study found evidence of undertreatment, in which 27% of patients with stage I to II pancreatic cancer received no treatment and only 47% underwent surgery (13). These findings highlight the importance of continuous medical education on the evolving pancreatic cancer treatment landscape and the need for clear and robust dialogue between physicians and patients.
In addition to the findings on patient and caregiver experiences in learning about and discussing treatment options with physicians, the study provided details specific to discussions about and potential participation in clinical trials. The pancreatic cancer community in the United States is very active in the design and execution of clinical studies. On average, there are at least 15 pancreatic cancer-specific trials open in the United States at any given time and available to patients in all stages of the disease (14). For example, on May 22, 2015, 144 trials were actively recruiting patients, with 26% for neoadjuvant and 8% for adjuvant treatments for pancreatic ductal adenocarcinoma (PDAC); 7% for locally advanced, 55% for metastatic, and 4% for recurrent PDAC; and 8% for pancreatic neuroendocrine tumors. However, just under half of survey respondents stated that they had never had a discussion with a doctor about trials. Of the respondents who did indicate that they had discussed clinical trials with a doctor, just over half named oncologists as the first to mention possible trial participation (Figure 2B). Overall, approximately 12% of respondents reported participation of the patient in a clinical trial (vs. the national average of approximately 4.6%) (10). In these cases, 4 of 5 respondents named the physician as the primary source of information on trials. These data seem to indicate an unmet need in the discussion of trials, which bears even greater importance considering that patients who participate in clinical trials report better outcomes than those receiving the same treatment outside of clinical trials (15). In an effort to increase awareness of pancreatic cancer trials, the Pancreatic Cancer Action Network launched an online Clinical Trial Finder, with a patient portal and a healthcare professional portal, in spring 2015 that provides access to its database of information on pancreatic cancer-specific trials in the United States.
Although this study focused primarily on the importance of physicians discussing treatments and trials with patients, the roles that caregivers can play in supporting the patient regarding treatment decisions should also be recognized. In a previous report, providing support on treatment days and communicating with physicians during medical appointments were listed among the key contributions of caregivers (12). In addition, 73% of respondents reported that the caregiver role included talking to the doctor and raising questions. Furthermore, 15.8% of respondents in the current study identified caregivers as being the first to mention clinical trials, second only to physicians (Figure 2B). Thus, caregivers are likely to have a major influence on the treatments that patients receive and the possibility of patients’ participation in clinical trials.
This study was subject to certain limitations, primarily because the population of survey respondents represented only a subset of the global pancreatic cancer community. These limitations have been described previously (12), but briefly, the main sources of potential bias appear to be based on geography (United States only), race (mostly white), sex (mostly female), and age (average age of 55.1 years, compared with the median age of pancreatic cancer diagnosis of 71 years) (16). In addition, a selection bias could exist in which this population of respondents who had an existing relationship with the Pancreatic Cancer Action Network might be more likely than average to have access to and actively seek information and treatment. The higher-than-average participation in clinical trials observed in this study could reflect this possibility.
The influence that physicians have in guiding patient choices regarding treatment and clinical trial participation, coupled with the likely benefit of each, should signal a call to action for physicians to remain alert to changes in treatment paradigms and to encourage in-depth dialogue with patients about treatments and trials. Potential benefits of active treatment and clinical trial participation include improvements in quality of life, survival, and symptom management, which were the three most important issues to respondents in this survey (12).
Acknowledgements
Writing assistance was provided by John McGuire, PhD, MediTech Media, and funded by Celgene Corporation. This work was supported by a grant provided by Celgene Corporation.
Footnote
Conflicts of Interest: Cara Thompson is an employee of Celgene Corporation. The other authors have no conflicts of interest to declare.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [PubMed]
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913-21. [PubMed]
- NCCN Clinical Practice Guidelines in Oncology. Pancreatic Adenocarcinoma. V2.2015. Available online: http://www.nccn.org/professionals/physician_gls/pdf/pancreatic.pdf, accessed July 8, 2015.
- Seufferlein T, Bachet JB, Van Cutsem E, et al. Pancreatic adenocarcinoma: ESMO-ESDO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol 2012;23 Suppl 7:vii33-40. [PubMed]
- Von Hoff DD, Ervin T, Arena FP, et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N Engl J Med 2013;369:1691-703. [PubMed]
- Conroy T, Desseigne F, Ychou M, et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med 2011;364:1817-25. [PubMed]
- Vincent A, Herman J, Schulick R, et al. Pancreatic cancer. Lancet 2011;378:607-20. [PubMed]
- Moertel CG, Frytak S, Hahn RG, et al. Therapy of locally unresectable pancreatic carcinoma: a randomized comparison of high dose (6000 rads) radiation alone, moderate dose radiation (4000 rads + 5-fluorouracil), and high dose radiation + 5-fluorouracil: The Gastrointestinal Tumor Study Group. Cancer 1981;48:1705-10. [PubMed]
- Cohen SJ, Dobelbower R Jr, Lipsitz S, et al. A randomized phase III study of radiotherapy alone or with 5-fluorouracil and mitomycin-C in patients with locally advanced adenocarcinoma of the pancreas: Eastern Cooperative Oncology Group study E8282. Int J Radiat Oncol Biol Phys 2005;62:1345-50. [PubMed]
- Hoos WA, James PM, Rahib L, et al. Pancreatic cancer clinical trials and accrual in the United States. J Clin Oncol 2013;31:3432-8. [PubMed]
- Kehl KL, Arora NK, Schrag D, et al. Discussion about clinical trials among patients with lung and colorectal cancer. J Clin Oncol 2014;32:abstr 6509.
- Engebretson A, Matrisian L, Thompson C. Pancreatic cancer: patient and caregiver perceptions on diagnosis, psychological impact, and importance of support. Pancreatology 2015;15:701-7. [PubMed]
- Enewold L, Harlan LC, Tucker T, et al. Pancreatic cancer in the USA: persistence of undertreatment and poor outcome. J Gastrointest Cancer 2015;46:9-20. [PubMed]
- The Pancreatic Cancer Action Network. Clinical trial finder. Available online: https://clinicaltrials.pancan.org, accessed July 8, 2015.
- Yang SH, Kuo YH, Tien YW, et al. Inferior survival of advanced pancreatic cancer patients who received gemcitabine-based chemotherapy but did not participate in clinical trials. Oncology 2011;81:143-50. [PubMed]
- Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975-2012. National Cancer Institute. Available online: http://seer.cancer.gov/csr/1975_2012/, accessed July 8, 2015.


