Percutaneous “Y” biliary stent placement in palliative treatment of type 4 malignant hilar stricture
Introduction
Malignant hilar strictures (MHS) at the liver hilum are caused by a heterogeneous group of tumors. Cholangiocarcinoma, a neoplasm originating from the intra- or extra-hepatic bile duct epithelium, is the leading cause of all MHS (1). Other MHS may be due to adjacent gallbladder, liver, and pancreatic tumors, or to metastatic hilar lymphadenopathy (2).
Stricture longitudinal extension can be assessed according to the Bismuth classification into types I to type IV (type I, tumor involves the common hepatic duct distal to the biliary confluence; type II, tumor involves the biliary confluence; type IIIa, tumor involves the biliary confluence plus the right hepatic duct; type IIIb, tumor involves the biliary confluence plus the left hepatic duct; type IV, multifocal or tumor involves the confluence and both the right and left hepatic ducts) (3).
Malignant stricture of the hepatic hilum are characterized by extremely poor prognosis resulting in a 5-year survival rate around 5%, and are also the most technically challenging biliary lesions for both endoscopic and interventional radiology management approaches (4).
The type 4 tumours have been generally regarded as inoperable except for liver transplantation (5).
For this reason most patients with an advanced disease receive palliative treatment rather than curative treatment. Palliative bilateral biliary drainage can be done percutaneously or endoscopically; however, in IV type biliary stenosis single tube drainage or stent may not take both primary bile ducts, so a bilateral drainage or multiple stent placement are necessary (6).
Newly designed stents for bilateral drainage with a “Y” configuration have been reported, but only a few reports including patients with Bismuth type IV strictures (7-9).
On the basis of this background we want to expose our experience about “stent-in-stent” (SIS) deployment technique with a “Y” configuration in the palliative treatment of type IV Bismuth, evaluating retrospectively its technical and clinical efficacy. Moreover, we examined the short-term and long-term complications associated with this method.
Methodology
Patients
Between March 2012 to November 2014, ten patients (four men and six women; mean age, 63±7 years) with type IV Bismuth-Corlette MHS underwent percutaneous bilateral SIS deployment using open cell-design stent with “Y” configuration: an excel database was prospectively recorded and retrospectively analysed. The study design was approved by the human ethics review board at our institution. Informed consent for data collection was obtained from each patient during this period. Main characteristics of patients are summarised in Table 1.
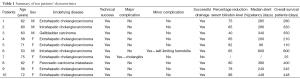
Full table
In the patient group, the causes of hilar obstruction included extrahepatic cholangiocarcinomas (n=6), intrahepatic cholangiocarcinomas (n=2), gallbladder carcinoma (n=1) and pancreatic carcinoma metastasis (n=1). The diagnosis of malignant biliary obstruction was obtained with tissue samples in seven patients, through percutaneous biopsies (n=3) or endoscopic brushing cytology and biopsy (n=4), and was made in the remaining three patients based on clinical-radiological findings (CT, MRCP or ERCP findings).
Patients were included if they had type IV Bismuth-Corlette MHS that could not be treated surgically, as a result of their tumor extension, advanced age or a comorbid condition. Patients who have abnormal coagulation status (international normalized ratio ≥1.5 and platelet count ≤50,000/mm3) or short life expectancy (<3 months) were excluded.
Technique
Before percutaneous transhepatic biliary drainage (PTBD), CT or MRI cholangiopancreatography was performed to assess the anatomy and plan the most appropriate approach for intervention; indeed, the pre-treatment work-out was important to evaluate possible congenital abnormalities in the biliary tree.
All procedures were performed by two senior interventional radiologists. Before stent placement bilateral internal-external PTBD was performed. All PTBD procedures and Y stent placement were performed in a digital subtraction angiography (DSA) suite under conscious sedation using IV tramadol hydrochloride (Contramal, Prodotti Formenti S.r.l.). Based on the MRI cholangiopancreatography dilated bilateral hepatic bile duct was initially punctured by a 21-gauge Chiba needle with fluoro-scopic or ultrasonography guidance. Cholangiography was obtained to assess the bile duct stenosis range and to evaluate the best way to pass stenosis. Subsequently, two 0.035" guide wire (Terumo, Japan) were passes separately into the distal section of the duodenum; we use hardened guide wire (Terumo) if it’s difficult cross the stenosis with normal ones.
Finally, two 8.5-French internal-external biliary drainage catheter was inserted bilaterally over the two guide wire to relieve jaundice or cholangitis before insertion of the stent (Figure 1A). Bilateral internal-external PTBD, washed with saline solution several times a day, allow to treat cholangitis, if present and decreasing the possibility of successive infectious complications. After 3-5 days stent insertion was accomplished.
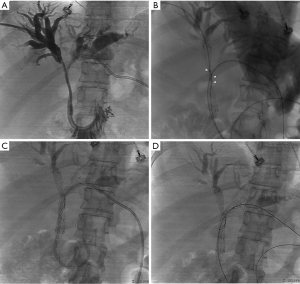
The stents used in this study were self-expandable nitinol stent. The transverse stent have Y-configuration, so called Y-stent (8.5 Fr, Niti-S Biliary Y-type, Taewoong Medical, Seoul, Korea). This stent type is composed by two single biliary stent, in which one has a central wide-open mesh region (2.5 cm in length) through which the latter one may be placed into the contralateral hepatic duct. This wide-open mesh region was pointed out by some visible markers (Figure 1B), through which pass second branch stent (8 Fr, Niti-S Biliary Y-type stent, Taewoong Medical, Seoul, Korea). Both branches stent were open cell-design stent, so as to allow passage of bile through the mesh. The fully expanded diameter of stents was 10 mm, and their fully expanded lengths were 6 and 8 cm, respectively. The length of the self-expandable metallic stents (SEMS) was chosen on the basis of the maximum size necessary to span the stenotic area using SIS deployment.
The technique of bilateral stent placement was carried out as follows. The site of obstruction was visualized after injecting contrast through drainage to show where begin biliary stricture so to decide at which level stent must reach into the healthy biliary tract. We prefer a second branch stent longer than first that open directly in duodenum. Subsequently, two long 0.035" guide wires (Radifocus; Terumo, Tokyo, Japan) was passed into the duodenum via the biliary drainage tubes. After removal of both drainage tubes a biliary routine predilatation was obtained with an 8 mm balloon catheter (Hurricane RX; Boston Scientific). The first branch Y stent was inserted over one of the double guide wires, and then it was released carefully observing its expansion and patency under fluoroscopy, trying to place radiopaque markers at the hepatic hilum. If complete implantation stent was difficult due to severe stenosis, the striction was dilated by balloon catheter previously used.
The second branch Y stent was inserted over contralateral guide wire passing through central wide open-mesh region, and then released; we used a balloon catheter if persisted stent strictures.
Subsequently, a temporary 8.5-French internal-external biliary drainage catheter was left so as to allow, washing frequently with saline solution, to remove possible blood clot or sludge, reducing the possibility of potential episodes of cholangitis (Figure 1C). A short-duration antibiotic prophylaxis therapy (3 days) was begun after stent placement with third generation cephalosporins and levofloxacin.
After 2-4 days the drainage catheter was removed over-the-wire if good stent patency, without any signs of bleeding, and a correct contrast agent flow through the “Y” stent into the common bile duct and the duodenum was confirmed (Figure 1D). Information about patients was obtained in all patients with medical records.
Study endpoints and definitions
Study endpoints include technical success, assessment of minor or major complications, successful internal drainage, stent patency, and patient survival.
Technical success was defined as stent deployment in an adequate position across the stricture with good contrast agent passage through the stents.
Major or minor complications were defined according to the guidelines of the society of Interventional Radiology Standards of Practice Commitee (10).
Successful drainage was defined as a decrease in bilirubin levels to more than half the pretreatment value during 2 weeks or its normalization within 1 month after stent placement.
Stent occlusion was defined as recurrence of jaundice, an increase in the bilirubin level, and dilatation of the intrahepatic bile duct demonstrated by imaging.
Stent patency time was defined as the elapsed time from the date of the drainage procedure to the date of stent malfunction (tumor ingrowth, tumor overgrowth and occlusion by sludge) as documented clinically or radiologically. If there was no evidence of obstruction during a patient’s lifetime, the patency period was considered equal to patient overall survival.
Overall survival is defined as the time from the biliary stenting to death for any cause.
Results
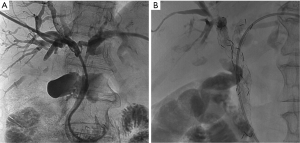
Clinical data of any patient were scheduled up until death or cut-off date of September, 2014. Technical success was obtained in all patients (100%; 10/10 cases) (Figure 2).
Major complication rate was 10% (1/10 cases) as one patients with cholangitis; however, we explain that for his poor general health due to rapid disease progression because we have obtained technical success. No other major complications such as peritonitis, biliary fistula and hematoma occurred during or after the operation.
Minor complication were observed in 1/10 patients (10%) as one patient with self-limiting hemobilia that completely resolved within 3 days without transfusion.
The temporary drainage catheters were removed from nine patients (90%) after the demonstration of good contrast agent passage through the stent through a follow-up cholangiography obtained 3-5 days after stent placement. In one patient (10%) the catheter was not removed because of the presence of cholangitis and an increased serum bilirubin level due to rapid disease progression (poor general health).
Successful drainage was obtained in nine patients in whom a decrease in total serum bilirubin level by 72.8% (range, 40-86%) was noted, result in in relief or improvement of symptoms.
The mean (± SD) serum total bilirubin level, which was 14.3±6.5 mg/dL before stent placement, decreased to 1.9±2.1 mg/dL in 1 month, with an obvious symptomatic relief in those patients.
Two (20%) patients presented with stent occlusion, in one owing to sludge formation, that required a percutaneous bilioplastic treatment, and in one owing to tumor overgrowth, that required repeat PTBD. In our experience tumor in-growth did not occur.
Median stent patency time was 315 days (range, 90-600 days) and overall survival patients’ time was 298 days (range, 25-600 days).
Discussion
The main cause of morbidity in MHS is cholestasis and its main complication is cholangitis. As matter of fact, many patients die not as a result of the expanding tumor but as a result of unresolvable cholangitis complicating the clinical course (5).
So the percutaneous or endoscopic biliary drainage have been established as effective and less invasive approach in unresectable MHS to resolve cholestasis, especially when compared with surgical biliary bypass (11).
In advanced MHS (Bismuth III and IV) percutaneous approach for biliary drainage is preferable to endoscopic one with a demonstrated high successful rate (93% vs. 77%, P=0.049) and a low level of procedure-related cholangitis. Moreover, percutaneous approach allows the precise lobar selection for drainage (12).
There is much controversy as to the importance of establishing drainage of adequate volume liver in malignant hilar obstruction. The goal of palliative drainage should be 50% or more liver volume; however, an undrained lobe or segment could incite cholangitis (13).
In patients with type IV Bismuth stricture some authors have reported superior patency rates and clinical outcomes when both biliary ducts were stented (8).
Moreover, in bifurcation tumors the best survival was noted in those with bilateral drainage, and the worst survival in those with cholangiographic opacification of both lobes but drainage of only one (14).
Two techniques are described in literature for bilateral biliary metallic stent placement: side-by-side (SBS) and SIS deployment techniques.
The SBS deployment technique results in the simultaneous insertion of two parallel metallic stents to drain the bile ducts of both hepatic lobes (15). The two metallic stent are parallel and closely itself at and below the hepatic confluence, preventing their full expansion with major probability of partial collapse of one or both stents.
In the SIS deployment technique, after placing the first metallic stent across the hilar stricture, a second stent is inserted into the undrained contralateral hepatic duct through the mesh of first stent (16). Thereby the single radial forces of both stents are added together opposing the centripetal force of biliary stricture, with a lower probability of stents displacement or collapse. So the entire length of stricture is expanded by a single stent caliber.
To date, a study that compares these two deployment technique with percutaneous approach does not exist. The main experience is on endoscopic approach where only two studies have examined the differences between SIS and SBS. The excessive expansion of the biliary duct especially in the region of SEMS overlap in SBS deployment technique is characterized by a high incidence of complications (cholecystitis, cholangitis, and liver abscess) compared to SIS deployment technique. Contrasting results there are about the stent patency time (17,18).
The experience about “Y” stent placement with percutaneous approach is limited a few study, in which are treated different kind of hilar strictures (from II to IV type Bismuth) with different types of stents. However, our results are in accordance with the results of this studies involving percutaneous bilateral metallic stent placement in patients with MHS (technical success rate, 95-100%; overall complication rates, 18-33%; successful drainage rates, 89-92%) (7-9).
The main technical difficulty is to pass a second metallic stent through the mesh of first one. The technical success was anyway the 100%, and post-procedural clinical response was very encouraging, with a serum total bilirubin level decrease in 90% of the cases. The operator skill and his experience on “Y” stent, however, have a great influence on the technical success.
Of note, there are some limitations in our study, one of which is the small sample size; moreover, even if we used the same “Y” stent type and all MHS is type 4 Bismuth, population is heterogeneous considering the different pathologies (cholangiocarcinoma, gallbladder carcinoma, and metastases). A multicentre future study with a large population is necessary. Further limitations of this study were the lack of a control group undergoing bilateral SBS stenting procedures, which would allow direct comparison.
In conclusion, percutaneous “Y” stent placement was proven a safe and clinically effective, minimally invasive palliative method for the management of malignant Bismuth IV biliary obstruction, alleviating the symptoms and improving the patients’ quality of life.
Acknowledgements
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Blechacz BR, Gores GJ. Cholangiocarcinoma. Clin Liver Dis 2008;12:131-50. ix. [PubMed]
- Larghi A, Tringali A, Lecca PG, et al. Management of hilar biliary strictures. Am J Gastroenterol 2008;103:458-73. [PubMed]
- Chung YE, Kim MJ, Park YN, et al. Staging of extrahepatic cholangiocarcinoma. Eur Radiol 2008;18:2182-95. [PubMed]
- Kim CW, Park AW, Won JW, et al. T-configured dual stent placement in malignant biliary hilar duct obstructions with a newly designed stent. J Vasc Interv Radiol 2004;15:713-7. [PubMed]
- Ruys AT, van Haelst S, Busch OR, et al. Long-term survival in hilar cholangiocarcinoma also possible in unresectable patients. World J Surg 2012;36:2179-86. [PubMed]
- Hwang JC, Kim JH, Lim SG, et al. Y-shaped endoscopic bilateral metal stent placement for malignant hilar biliary obstruction: prospective long-term study. Scand J Gastroenterol 2011;46:326-32. [PubMed]
- Gwon DI, Ko GY, Kim JH, et al. Percutaneous bilateral metallic stent placement using a stentin-stent deployment technique in patients with malignant hilar biliary obstruction. AJR Am J Roentgenol 2013;200:909-14. [PubMed]
- Inal M, Akgül E, Aksungur E, et al. Percutaneous placement of biliary metallic stents in patients with malignant hilar obstruction: unilobar versus bilobar drainage. J Vasc Interv Radiol 2003;14:1409-16. [PubMed]
- Rerknimitr R, Kongkam P, Kullavanijaya P. Outcome of self-expandable metallic stents in low-grade versus advanced hilar obstruction. J Gastroenterol Hepatol 2008;23:1695-701. [PubMed]
- Sacks D, McClenny TE, Cardella JF, et al. Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol 2003;14:S199-202. [PubMed]
- Rerknimitr R, Angsuwatcharakon P, Ratanachu-ek T, et al. Asia-Pacific consensus recommendations for endoscopic and interventional management of hilar cholangiocarcinoma. J Gastroenterol Hepatol 2013;28:593-607. [PubMed]
- Paik WH, Park YS, Hwang JH, et al. Palliative treatment with self-expandable metallic stents in patients with advanced type III or IV hilar cholangiocarcinoma: a percutaneous versus endoscopic approach. Gastrointest Endosc 2009;69:55-62. [PubMed]
- Vienne A, Hobeika E, Gouya H, et al. Prediction of drainage effectiveness during endoscopic stenting of malignant hilar strictures: the role of liver volume assessment. Gastrointest Endosc 2010;72:728-35. [PubMed]
- Chang WH, Kortan P, Haber GB. Outcome in patients with bifurcation tumors who undergo unilateral versus bilateral hepatic duct drainage. Gastrointest Endosc 1998;47:354-62. [PubMed]
- Saleem A, Baron TH, Gostout CJ. Large-diameter therapeutic channel duodenoscope to facilitate simultaneous deployment of side-by-side self-expandable metal stents in hilar cholangiocarcinoma. Gastrointest Endosc 2010;72:628-31. [PubMed]
- Chahal P, Baron TH. Expandable metal stents for endoscopic bilateral stent-within-stent placement for malignant hilar biliary obstruction. Gastrointest Endosc 2010;71:195-9. [PubMed]
- Naitoh I, Hayashi K, Nakazawa T, et al. Side-by-side versus stent-in-stent deployment in bilateral endoscopic metal stenting for malignant hilar biliary obstruction. Dig Dis Sci 2012;57:3279-85. [PubMed]
- Kim KM, Lee KH, Chung YH, et al. A comparison of bilateral stenting methods for malignant hilar biliary obstruction. Hepatogastroenterology 2012;59:341-6. [PubMed]


