Liver resection for metastatic colorectal leiomyosarcoma: a single center experience
Introduction
Leiomyosarcoma arising in the colorectum is a rare smooth muscle tumor that occurs primarily in the sigmoid and transverse colon (1,2), accounting for less than 1% of all malignancies of colon and rectum. It is most frequent occurring in middle-aged patients with an equal male: female ratio (3). Curative surgical resection of the primary can be achieved in 50% to 60% of cases. Hematogenous spread to the liver and lungs are described as the most common cause of death in these patients (4,5). There has been only one case of leiomyosarcoma of colonic origin with liver metastasis reported in the literature (6). We reviewed all the liver resections performed at the American University of Beirut Medical Center from 1998 to 2009. Of the 252 liver resections performed, five (0.012%) were in patients who had undergone surgical resection of metastatic leiomyosarcoma of colorectal origin with liver metastases. The aim of this small case series study is to present our experience in this rare pathological entity with a review of the literature.
Methods & results
From 1998 to 2009 five patients diagnosed with primary leiomyosarcoma of colorectal origin with metastatic liver disease underwent liver resections at the American University of Beirut Medical Center. The median overall survival for the five patients was 47 months with a range of 7-135 months.
Case 1
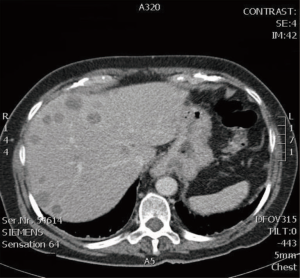
A 68-year-old female patient presented with abdominal pain of 3 weeks duration. There were no associated symptoms and physical examination was non-revealing. Laboratory investigations were normal, with carcinoembryonic antigen (CEA) level 1.4 ng/mL (normal range, 0-4 ng/mL). Computed tomography (CT) scan revealed a large 15 cm × 9 cm mass in the right hepatic lobe, with multiple smaller lesions in the right lobe of the liver (Figure 1). A fine needle aspiration of the liver lesion was performed and revealed a spindle cell tumor. The patient underwent a complete colonoscopy, which identified a right colonic mass. The patient underwent a synchronous right hepatectomy (segments 5, 6, 7, 8) with a right hemicolectomy. All surgical margins were negative. Final Pathology was consistent with leiomyosarcoma of the colon with liver metastases; there was high-grade atypia and atypical mitoses. Both operative and postoperative courses were uneventful. Adjuvant chemotherapy (doxorubicin) was started 4 weeks post-surgery. The patient passed away three years following resection from recurrent disease.
Case 2
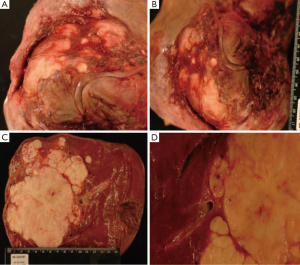
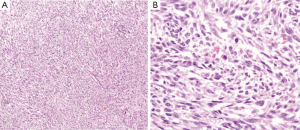
A 24-year-old female patient presented with right upper quadrant abdominal pain of one week duration. CT scan revealed a large 12 cm × 9 cm mass in the right lobe of the liver with other small lesions in the same lobe (Figure 2). Liver biopsy showed metastatic leiomyosarcoma. A colonoscopy identified a mass in the sigmoid colon. The patient underwent a left colectomy followed by an extended right hepatectomy (segments 4a, 4b, 5, 6, 7, 8) and cholecystectomy two weeks later. Margins, gross and microscopic, were negative for residual tumor. Pathology revealed metastatic leiomyosarcoma of colonic origin with severe nuclear atypia and a high number of mitoses (Figure 3). The patient passed away three and a half years following resection from recurrent disease.
Case 3
A 47-year-old female patient with a history of resected rectal leiomyosarcoma was found to have a 5 cm × 6 cm liver mass on follow-up imaging performed 2 years after surgery for the primary malignancy. She was asymptomatic at presentation of recurrence and no masses were palpable on abdominal examination. CT-guided fine needle aspiration of the liver lesion was consistent with leiomyosarcoma. A right hepatectomy (segments 5, 6, 7, 8) was performed and revealed two lesions in the right lobe of the liver. Pathology confirmed metastatic leiomyosarcoma of the rectum with high grade atypia. Both operative and postoperative courses were uneventful. The patient survived for 11 years and passed away after from recurrent disease.
Case 4
A 69-year-old male with a history of resected sigmoid leiomyosarcoma with small volume pulmonary metastases presented with early satiety, abdominal pain and weight loss. Physical examination revealed hepatomegaly. The patient had a low hemoglobin of 9.2 g/dL (range, 14-18 g/dL) and platelet count of 89×109/L (range, 130×109-400×109/L). His liver function tests were within normal range except for elevated alkaline phosphatase [246 IU/L (range, 20-125 IU/L)], and gamma-glutamyl transferase [262 IU/L (range, 0-65 IU/L)]. CT scan of the abdomen revealed two right liver metastases. The patient underwent a right hepatectomy (segments 5, 6, 7, 8) and cholecystectomy with negative margins. Pathology confirmed metastatic leiomyosarcoma of the colon (high grade spindle cell neoplasm). The patient had to be re-explored for post-operative bleeding from the surgical bed. The patient recovered and was discharged home day 11. He had lung and liver recurrence a few months after surgery and passed away 7 months post liver resection.
Case 5
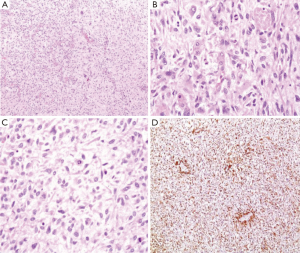
A 30-year-old male patient presented with short duration right upper quadrant abdominal pain. History and physical exam were otherwise negative. Laboratory tests were as follows: Hemoglobin 10 g/dL (range, male 13.0-18.0 g/dL), alkaline phosphatase 158 IU/L (range, 35-120 IU/L), and g-GT 162 IU/L (range, 10-50 IU/L). CT scan demonstrated two complex right liver cystic lesions and a left adrenal mass. A decision was made to proceed to exploratory laparotomy with resection of the complex liver cysts. The patient underwent a right hepatectomy (segments 5, 6, 7, 8) and left adrenalectomy. Margins were negative. The pathology revealed a high-grade pleiomorphic sarcoma with numerous mitoses and myxoid features consistent with pleiomorphic leiomyosarcoma of the colon (Figure 4). Both operative and postoperative courses were uneventful. Thereafter the patient underwent a colonoscopy, which demonstrated a 3 cm × 4 cm right colonic lesion which was subsequently resected. The patient received adjuvant chemotherapy (doxorubicin/ifosfamide). He passed away 1.5 years following resection from recurrent disease.
Discussion
Leiomyosarcoma is a rare malignant tumor of smooth muscle origin. It occurs primarily in the alimentary tract (stomach, small bowel and colon), the genitourinary tract (uterus, bladder, prostate, kidney), and the retroperitoneum (inferior vena cava) (7). Leiomyosarcoma of colonic origin originates from the smooth muscle cells of the muscularis mucosa, muscularis propria, or the wall of blood vessels (2,8). In the gastrointestinal tract, smooth muscle tumors account for less than 1% (9,10). Of these rare cases of smooth muscle tumors, colon involvement occurs in only 3.4% of them (10). The incidence of leiomyosarcoma of colonic origin is reported to be 0.45 cases per million people annually, thus accounting for less than 0.1% of all types of malignancies of colonic origin (11,12). Leiomyosarcoma of rectal origin develops at least twice as frequently as in the colon (1,13). In the latter, mucosal involvement occurs in 30% to 50% of patients (4). There is no general consensus on the frequency of metastasis of these tumors to the liver. While described by some to be rare (14), others report that 62% of all visceral sarcomas metastasize to the liver (15), gastrointestinal leiomyosarcomas being the most common of these. Leiomyosarcoma arising in the colon are mostly found in individuals between 50 and 70 years of age (3), although cases involving a newborn and an 82-year-old have been reported (16,17).
There is no definite site of origin predilection for the location of leiomyosarcomas in the colon (17), although sigmoid and transverse colon sites are observed to be the most common (1,2). Leiomyosarcomas originating from the colon are relatively avascular, non-capsular, well-circumscribed lesions, varying in diameter from 5 to 15 cm. They are more frequently rounded and lobulated, although sometimes pedunculated and rarely multifocal (18). Histologically, these lesions show interlacing bundles of spindle-shaped smooth-muscle cells, as well as cellular pleomorphism, vasoinvasion, large hyperchromatic nuclei with prominent nucleoli and presence of bizarre tumor cells, including giant cells (4,19). The most important histologic criterion, however, is mitotic activity, as it is the best predictor of both prognosis and tendency to metastasize (19). The histologic grading of malignant tumors is based on the Broder classification (19,20). Grade 1 was characterized as having one mitosis per 10 to 20 high power field (HPF), grade 2 as having one mitosis per 10 HPF, grade 3 as having two to five mitoses per HPF and grade 4 as having more than five mitoses per HPF. There were, nonetheless, findings of tumors with minimal atypia that have metastasized (21). In all our patients, the degree of atypia was very high with numerous mitoses, although the number per HPF was not documented. This criterion, however, applies to primary tumors rather than metastatic findings as is the case in our results.
Leiomyosarcomas can remain asymptomatic for long periods of time (22). This emphasizes the importance of routine examination and extended follow-up, which greatly increases the probability of early detection, thus increasing survival rates, especially since these malignancies can have a variable clinical course and late presentations of metanchronous metastases can occur years later In the few series reporting leiomyosarcomas with hepatic spread (6,14,23), none described an initial presentation with synchronous liver metastasis. In the case of our patients, the most common symptom at initial presentation was abdominal pain. Only one out of five patients was asymptomatic at presentation, and his tumor was discovered incidentally on routine follow-up.
No specific tumor markers have been found for leiomyosarcoma. Colonoscopy with tumor biopsy remains the most important diagnostic modality (24). Nonetheless, Cox et al. also reported increased uptake of indium-111 antimyosin in leiomyosarcoma tissue because of increased permeability, suggested as a potential tool for diagnosis of recurrent disease (25). In a study by Ren et al. in 2007, lower levels of the adhesive molecule integrin α7 mRNA were found in leiomyosarcoma specimens as compared to normal tissue (26).
The most common sites of metastasis for leiomyosarcoma arising in the colorectum are the lungs and the peritoneum (27,28). The frequency of liver metastases is debated (14,15), although hematogenous spread to the liver and lungs are the most common cause of death (4,5). Regional lymph node metastasis is relatively uncommon (1,5,8,29) (Table 1).
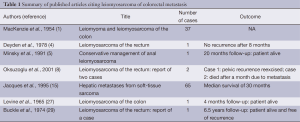
Full table
In the literature, only one report involved the colon as a primary site of leiomyosarcoma (6). Leiomyosarcoma arising in the colorectum metastatic to the liver has commonly been described as cystic (5,30-32), with a homogeneous hypodense consistency and thin nonenhancing wall (14). Calcification was also reported in a liver metastasis from leiomyosarcoma originating from the colon (6), although rare (14). CT imaging of the liver in patients with metastatic leiomyosarcoma arising in the colorectum shows a characteristic central necrosis (6), more frequent in larger tumors, but not always exhibited by smaller lesions (33). However, when the characteristic CT findings are present, the specific diagnosis of leiomyosarcoma may be suggested (6). Liver cysts were identified by CT scan in one of our patients.
Although there is no definitive treatment strategy for leiomyosarcoma arising in the colon, surgery remains the mainstay, like other sarcomas, it is relatively chemoresistant and radioresistant (8). There are no randomized controlled data, however based on current literature, chemotherapy and radiation appear to have no beneficial effect on recurrence or survival in patients with leiomyosarcoma (22,34,35). Initially, anorectal leiomyosarcoma was treated by local excision or enucleation. However, because of high recurrence rates and spread leading to death (34), a more radical surgical approach including abdominoperineal resection was later used (12,36), even for cases demonstrating mild atypia (37). Nonetheless, Randleman et al. (34) found that tumor-free period after surgery for an anorectal leiomyosarcoma was not significantly affected by the conservative or radical nature of the procedure (P=0.36), where 9 out of 11 patients who underwent radical surgery remained tumor free after 2 years, while 7 out of 10 patients who underwent conservative surgery remained tumor free after the same period of time. Khalifa et al. (36) reported a recurrence rate of 67.5% (27 out of 40 patients) after treatment with local excision as compared to a 19.5% (8 out of 41 patients) recurrence rate after abdominoperineal resection. Other authors including Oksuzoglu (8) suggest that radical approaches should be reserved to high grade and/or large tumors (>5 cm) which tend to have a worse prognosis, whereas small (<3 cm) and localized (< T2) with low grade histology can be treated with parenchymal sparing liver surgery such as wide local excision. Long-term follow-up is recommended in all gastrointestinal smooth muscle tumors, because late recurrence has been noted (38).
In our series, two patients had a previous surgical history of leiomyosarcoma of the colon; and both were treated by local excision of the tumor rather than a more radical approach. Metastasis to the liver occurred 2 and 1.5 years after the excision of the primary tumor in each of the patients respectively.
Regarding liver metastasis from leiomyosarcoma, there are no randomized controlled data for management; however, based on current literature, liver resection has been shown to prolong survival (23). In a study by Chen et al. in 1998, survival of the patients with hepatic metastasis of leiomyosarcoma arising in the colorectum depended on resection status of the liver mass (positive versus negative margins), and not on other parameters such as histologic grade, number of liver lesions or size of liver lesions, where 11 patients who underwent resection of isolated metastases from leiomyosarcoma were reviewed. In our series all five patients all had negative margins for the hepatic resection (23).
In conclusion, leiomyosarcoma of colorectal origin with liver metastasis is a very rare entity that has not been well discussed in the literature. Liver spread is cited as one of the most common cause of death in patients with leiomyosarcoma (4,5). In our experience, wide surgical excision with negative margins is the treatment of choice for these patients and can selectively lead to prolonged survival.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- MacKenzie DA, McDonald JR, Waugh JM. Leiomyoma and leiomyosarcoma of the colon. Ann Surg 1954;139:67-75. [PubMed]
- Rogers V. Leiomyosarcoma of the colon. Br J Radiol 1961;34:748-50. [PubMed]
- Akwari OE, Dozois RR, Weiland LH, et al. Leiomyosarcoma of the small and large bowel. Cancer 1978;42:1375-84. [PubMed]
- Deyden WE, Wilkinson CA. Leiomyosarcoma of the rectum. South Med J 1978;71:743-5. [PubMed]
- Minsky BD, Cohen AM, Hajdu SI. Conservative management of anal leiomyosarcoma Cancer 1991;68:1640-3. [PubMed]
- Clark RA, Alexander ES. Computed tomography of gastrointestinal leiomyosarcoma. Gastrointest Radiol 1982;7:127-9. [PubMed]
- McLeod AJ, Zornoza J, Shirkhoda A. Leiomyosarcoma: computed tomographic findings. Radiology 1984;152:133-6. [PubMed]
- Oksuzoglu B, Guler N, Uner A, et al. Leiomyosarcoma of the rectum: report of two cases. Turkish J Cancer 2001;31:131-4.
- Rao BK, Kapur MM, Roy S. Leiomyosarcoma of the colon: a case report and review of the literature. Dis Colon Rectum 1980;23:184-90. [PubMed]
- Baker HL Jr, Good CA. Smoothmuscle tumors of the alimentary tract; their roentgen manifestations. Am J Roentgenol Radium Ther Nucl Med 1955;74:246-55. [PubMed]
- Friesen R, Moyana TN, Murray RB, et al. Colorectal leiomyosarcomas: a pathobiologic study with long-term follow-up. Can J Surg 1992;35:505-8. [PubMed]
- Diamante M, Bacon HE. Leiomyosarcoma of the rectum: report of a case. Dis Colon Rectum 1967;10:347-51. [PubMed]
- Buxton RW. Smooth muscle tumors of the gastrointestinal tract. Am Surg 1960;26:666-77. [PubMed]
- Soyer P, Bluemke DA, Riopel M, et al. Hepatic leiomyosarcomas: CT features with pathologic correlation. Eur J Radiol 1995;19:177-82. [PubMed]
- Jaques DP, Coit DG, Casper ES, et al. Hepatic metastases from soft-tissue sarcoma. Ann Surg 1995;221:392-7. [PubMed]
- Kriss N. Leiomyosarcoma of the colon in an infant. Am J Roentgenol Radium Ther Nucl Med 1960;84:540-5. [PubMed]
- Cho KC, Smith TR. Multiple leiomyosarcoma of the transverse colon: report of a case and discussion. Dis Colon Rectum 1980;23:118-21. [PubMed]
- Stavorovsky M, Jaffa AJ, Papo J, et al. Leiomyosarcoma of the colon and rectum. Dis Colon Rectum 1980;23:249-54. [PubMed]
- Warkel RL, Stewart JB, Temple AJ. Leiomyosarcoma of the colon: report of a case and analysis of the relationship of histology to prognosis. Dis Colon Rectum 1975;18:501-6. [PubMed]
- Anderson PA, Dockert MB, Buie LA. Myomatous tumors of the rectum (leiomyomas and myosarcomas). Surgery 1950;28:642-50. [PubMed]
- Matsuda T, Condon RE. Leiomyosarcoma of the colon with metastasis to the liver: right hepatic lobectomy in presence of variant hepatic artery. J Surg Oncol 1971;3:533-8. [PubMed]
- Astarjian NK, Tseng CH, Keating JA, et al. Leiomyosarcoma of the colon: report of a case. Dis Colon Rectum 1977;20:139-43. [PubMed]
- Chen H, Pruitt A, Nicol TL, et al. Complete hepatic resection of metastases from leiomyosarcoma prolongs survival. J Gastrointest Surg 1998;2:151-5. [PubMed]
- Iwasa K, Taniguchi K, Noguchi M, et al. Leiomyosarcoma of the colon presenting as acute suppurative peritonitis. Surg Today 1997;27:337-44. [PubMed]
- Cox PH, Verweij J, Pillay M, et al. Indium 111 antimyosin for the detection of leiomyosarcoma and rhabdomyosarcoma. Eur J Nucl Med 1988;14:50-2. [PubMed]
- Ren B, Yu YP, Tseng GC, et al. Analysis of integrin alpha7 mutations in prostate cancer, liver cancer, glioblastoma multiforme, and leiomyosarcoma. J Natl Cancer Inst 2007;99:868-80. [PubMed]
- Levine S, Kiehl PV, Serfas LS. Leiomyosarcoma of the colon. Am J Surg 1965;109:816-8. [PubMed]
- Meszaros WT. Leiomyosarcoma of the colon. Am J Roentgenol Radium Ther Nucl Med 1963;89:766-70. [PubMed]
- Buckle AE, Evans IL. Leiomyosarcoma of the rectum: report of a case. Dis Colon Rectum 1974;17:109-11. [PubMed]
- Noon MA, Young SW, Castellino RA. Leiomyosarcoma metastatic to the liver: CT appearance. J Comput Assist Tomogr 1980;4:527-30. [PubMed]
- Federle MP, Filly RA, Moss AA. Cystic hepatic neoplasms: complementary roles of CT and sonography. AJR Am J Roentgenol 1981;136:345-8. [PubMed]
- Arrive L, Kraiem C, Roche A. Morphological diagnosis of pseudocystic tumors of the liver. Gastroenterol Clin Biol 1988;12:516-20. [PubMed]
- Skandalakis JE, Gray SW, Shepard D. Smooth muscle tumors of the stomach. Int Abstr Surg 1960;110:209-26. [PubMed]
- Randleman CD Jr, Wolff BG, Dozois RR, et al. Leiomyosarcoma of the rectum and anus. A series of 22 cases. Int J Colorectal Dis 1989;4:91-6. [PubMed]
- Asuncion CM. Leiomyosarcoma of the rectum: report of two cases. Dis Colon Rectum 1969;12:281-7. [PubMed]
- Khalifa AA, Bong WL, Rao VK, et al. Leiomyosarcoma of the rectum. Report of a case and review of the literature. Dis Colon Rectum 1986;29:427-32. [PubMed]
- Nuessle WR, Magill TR 3rd. Leiomyosarcoma of the transverse colon. Report of a case with discussion. Dis Colon Rectum 1990;33:323-6. [PubMed]
- Evans HL. Smooth muscle tumors of the gastrointestinal tract. A study of 56 cases followed for a minimum of 10 years. Cancer 1985;56:2242-50. [PubMed]


