
Current status of laparoscopic liver resection for the management of colorectal liver metastases
Introduction
Colorectal cancer (CRC) poses a significant health burden globally. Presently, with over 1.8 million new cases and 881,000 deaths per year, its incidence and mortality rank as third and second amongst all cancers worldwide (1). The liver is the commonest site for metastatic spread from CRC. About 15–20% of patients have synchronous colorectal liver metastasis (CLRM) at the time of diagnosis, and up to 40% develop metastatic lesions during follow-up (2). Liver resection when feasible combined with chemotherapy offers the best chance of cure, with reported 5-year survival and 10-year survival rates of 33–58% and 23–39%, respectively.
The arrival of minimally invasive procedures has completely revolutionized the landscape of abdominal surgery in the last few decades. However, even though the first laparoscopic liver resection (LLR) was reported in 1991 by Reich et al. (3), liver surgeons were hesitant to jump on the bandwagon due to initial concerns about technical challenges, hemorrhage control and oncologic outcomes. Fortunately, advances in surgical technology, refinements of operative technique as well as diffusion of standardized good practices have allowed these barriers to be overcome. In a recent large systematic review of 9,527 LLR worldwide, 65% were performed for malignant lesions (4), which was a significant increase from 50% just a decade ago (5). More impressively, the mortality rate was extremely low at only 0.39%. This study demonstrated the growing safety of this complex procedure in selected patients when performed by expert surgeons in high-volume centers.
Today, CLRM presents one of the commonest indications for LLR. Several meta-analyses (2,6-13) and two randomized trials have been published to date on this topic (14,15), with additional prospective trials underway. In the recent Southampton Consensus Guidelines for laparoscopic liver surgery (16), LLR was recommended as a valid alternative to open liver resection (OLR) in experienced hands due to superior short-term outcomes and non-inferior oncologic and survival outcomes.
We present here a brief review of the literature on the current status of LLR for CLRM, and discuss potential benefits and limitations of the laparoscopic approach unique to this pathology.
Perioperative and short-term outcomes
The recent OSLO-COMET randomized controlled trial (RCT) was a landmark study which demonstrated that LLR for CLRM was associated with lower postoperative complication rates (19% vs. 31%, P=0.021) and shorter postoperative hospital stay (53 vs. 96 hours, P<0.001) as compared to open liver resection (OLR), with no differences in bloodloss, operation time or 90-day mortality rates (14). In a subgroup analysis of this trial considering only patients with tumours in the posterosuperior segments, the LLR group similarly enjoyed shorter postoperative length of stay (LOS) and significantly better health related quality of life (17). The recently published LapOpHuva study was only the second prospective RCT to date comparing outcomes following laparoscopic vs. open hepatectomy for CLRM (15). In keeping with the results of the OSLO-COMET trial, patients undergoing LLR had lower overall morbidity (11.5% vs. 23.7%, P=0.025) and shorter hospital stay (4 vs. 6 days, P<0.001), but similar surgical times, bloodloss, blood transfusion and mortality rates as the OLR cohort.
Retrospective studies seem to suggest that the laparoscopic approach confers even more benefits. Table 1 highlights several meta-analyses which have been published on this topic (2,6-13), with 2 of the largest studies involving more than 4,000 patients each (2,12). The common theme from these seems to be that LLR is associated with lower blood loss and blood transfusion rates in addition to shorter length of stay and reduced post-operative complications, with similar mortality rates to OLR. This is similar to studies analyzing the application of LLR in HCC, which also report improved short-term outcomes even in major hepatectomies (18,19). Surprisingly, surgical times are reported to be longer in LLR in only 2 studies by 14 (12) and 40 minutes (13) respectively, while the rest reported no significant differences.
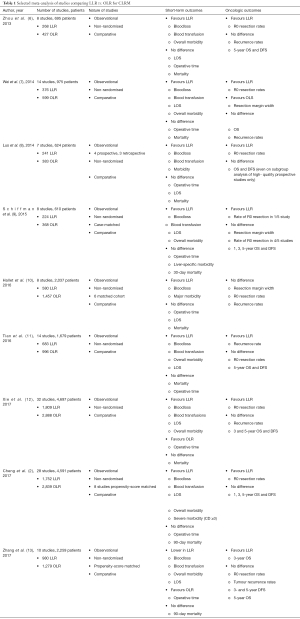
Full table
In order to mitigate selection bias which is inherently present in retrospective studies, Zhang et al. performed a meta-analysis of 10 propensity-matched studies involving 2,259 patients (980 LLR, 1,279 OLR) (13). They concluded similarly that LLR resulted in lower bloodloss (WMD −124.68 mL), blood transfusion rates, overall morbidity and shorter length of stay, but slightly longer operative time (WMD 39.48 minutes) although there was significant heterogeneity in these studies. The same benefits of laparoscopic resection persisted in Schiffman’s meta-analysis of 8 case-matched studies, where both groups were well-balanced in terms of demographics, tumour characteristics and extent of operation (9). In another recent interesting study, Ciria et al. analysed 21 manuscripts by subgroups, depending on whether they involved only minor or major liver resections, synchronous resections, or ‘combined’ resections if they could not be allocated to any of the categories (20). For minor resections, the LLR group enjoyed lower bloodloss and shorter LOS, with similar complication rates and operative time. When only major resections were considered, LLR resulted in reduced LOS only, with no differences in bloodloss, operative duration or post-operative morbidity rates. Five studies involving 212 open vs. 187 laparoscopic synchronous colorectal-liver resections demonstrated comparable short-term outcomes between both groups except for shorter LOS in the LLR group. However, in the ‘combined’ subgroup (both major and minor resections), LLR was associated with fewer complications, blood transfusions and shorter LOS, with no differences in bloodloss or surgical time.
Several reasons have been proposed to account for the encouraging peri-operative and short-term outcomes following laparoscopic resection of CLRM. The magnified view presented by the camera facilitates meticulous dissection of vasculobiliary structures; pneumoperitoneum tamponades venous ooze from the liver while the smaller incisions result in less bleeding from the abdominal wall (6). This is particularly useful in minimizing bloodloss during hepatectomy for CLRM, where chemotherapy-associated sinusoidal obstruction, regenerative nodular hyperplasia or steatohepatitis of the liver may render patients more susceptible to bleeding (21,22). In LLR, all blood is aspirated and collected for charting, hence the estimated bloodloss is likely to be more accurate compared to open surgery where sponges are used to absorb and tamponade bleeding (9). This may facilitate a more restrictive blood transfusion policy in laparoscopic resections. Reduced surgical trauma, intra-operative bleeding and blood product replacement are in turn closely linked to post-operative morbidity which is therefore similarly lowered. The smaller incisions used in laparoscopy result in less postoperative pain and analgesia use (23), with earlier return of bowel function and tolerance of diet (24). These facilitate early ambulation and quicker recovery after surgery, hence allowing patients to be discharged sooner. A predefined substudy of the OSLO-COMET trial proved definitively that patients undergoing LLR for CLRM enjoyed better postoperative health-related quality of life (HRQoL) at 1 and 4 months compared to their counterparts in the open resection group (25).
Oncologic and long-term outcomes
When indications for LLR expanded to include malignant conditions, the adequacy of resection margin status was one of the foremost concerns. This was especially because in laparoscopy, the loss of tactile feedback no longer permitted the palpation of solid lesions within liver parenchyma. To overcome this and other limitations involving laparoscopic liver mobilization particularly of posterosuperior segments, hand-assisted laparoscopic surgery (HALS) was initially employed (26). However, the presence of a gloved hand in a limited field often impaired the surgical view. Hence, surgeons learned to perform careful intra-operative ultrasonography (IOUS) to identify deep-seated malignant lesions, thus ensuring that acceptable resection margins were being achieved even in laparoscopic resections (27). As seen in Table 1, most meta-analyses to date have concluded that resection margin status and recurrence rates following LLR are not inferior to the open approach, with several studies reporting even higher rates of R0 resection in the laparoscopic groups (2,6,8,9,12). Only Tian’s study concluded otherwise, but even than the LLR patients had lower recurrence rates in their report (11). In the OSLO-COMET prospective trial, there were similarly no differences in rates of R0 resection or positive resection margins between the LLR and OLR groups (14). Recently, real-time indocyanine green (ICG) fluorescence imaging has also been reported to be useful in laparoscopy for the detection and localization of hepatic tumours including CLRM (28-30).
The long-awaited survival outcomes of the OSLO-COMET trial were revealed very recently (31). Median overall survival (OS) was 80 months (95% CI: 52–108) in the LLR group and 81 months (95% CI: 42–120) in the open surgery group (P=0.91). By modified intention-to-treat analysis of only patients that had R0/R1 resection, the median recurrence-free survival (RFS) was 19 months (95% CI: 10–27) in the laparoscopic group and 16 months (95% CI: 11–21) in the open group (P=0.96). In the LapOpHuva randomized trial, a secondary endpoint was to compare long-term outcomes, which were also found to be similar between both laparoscopic and open surgery groups (15). The cumulative 1, 3, 5, 7-year OS for LLR and OLR were 92.5%, 71.5%, 49.3%, 35.6% vs. 93.6%, 69.7%, 47.4%, 35.5%, respectively (P=0.82). Disease-free survival (DFS) for LLR and OLR was 72.7%, 33.5%, 22.7%, and 20.8% vs. 61.6%, 27.2%, 23.9%, and 17.9%, respectively (P=0.23). In keeping with the findings from these trials, almost all the meta-analyses of retrospective studies found no significant differences in OS, DFS or RFS between the laparoscopic and open groups (2,6-12). Interestingly, in a meta-analysis of propensity-matched studies comprising of 2,259 patients, LLR was associated with a better 3-year OS (P=0.003), although this evened out by 5 years (13). Similarly, a recently published meta-analysis of individual patient data from 2 randomized trials and 13 propensity-matched studies found a survival advantage of laparoscopic resection of CLRM even at the 10-year mark, and in elderly patients (32).
Selection bias may explain these results to a certain extent. In early studies, patients chosen to undergo laparoscopic resection were a highly selected population with small tumours in easily accessible peripheral segments, while large complex tumours invading vessels or adjacent organs were reserved for the open approach (6,9). Furthermore, LLR was mainly performed by very experienced surgeons in high-volume centers. For example, the LapOpHuva trial was only started after the authors had completed at least 50 LLR and had standardized their surgical technique, while OSLO-COMET was commenced after more than 400 laparoscopic resections were performed in the center (14,15). Surgical expertise and experience are independent predictors of overall survival, and hence this may have influenced outcomes (33-35).
There are several other plausible mechanisms to explain the encouraging survival outcomes following LLR. Blood transfusion and post-operative morbidity are well-known to be independently associated with survival (36-38), and the reduced rates of these in LLR may have contributed to the long-term outcomes. A sizeable fraction of patients experiences intrahepatic recurrence of CLRM after the index hepatectomy. For these individuals, an initial laparoscopic approach has been shown to increase the feasibility of future salvage hepatectomies through the reduction in the burden of dense adhesions (39). Adjuvant chemotherapy is a pivotal component in the treatment of CRC with metastatic liver disease, and patients undergoing LLR can resume chemotherapy regimens sooner than their counterparts who undergo open surgery (40-43). Immune-mediated mechanisms must also be considered—in an exploratory biomarker analysis of the Oslo-CoMet trial, open resection was found to induce heightened levels of pro-inflammatory molecules such as the HMGB-1 chemokine (44). Indeed, recent translational studies have demonstrated that inflammatory molecules that aid wound healing after surgery also promote oncogenesis and trigger the outgrowth of dormant metastases, and this biological phenomenon has been proposed to account for the sharp rise in distant recurrence rates after surgery for certain cancer types such as breast cancer (45). Anti-cancer immunosurveillance has been found to be diminished by surgical stress, therefore the higher levels of surgical stress after an open laparotomy may render patients more susceptible to cancer recurrence than their counterparts who undergo laparoscopy (46-49).
Repeat liver resection
CLRM tend to recur in up to 70–80% of patients. Although repeat liver resection together with chemotherapy offers patients the best chance of survival (22,50), it is technically challenging due to anatomical distortions and adhesions induced by the index surgery. Indeed, in the Southampton Guidelines for LLR, it is suggested that repeat liver resection via a laparoscopic approach should be avoided in the initial learning curve (16). However, a number of studies from high-volume centers have demonstrated the safety and feasibility of laparoscopic repeat liver resection (LRLR) in expert hands. A recent meta-analysis of 8 studies confirmed that LRLR may be performed with no increase in morbidity rates or hospital stay compared to open RLR (ORLR), even if the original hepatectomy was performed open (51). A propensity score-matched study of repeat liver resection for CLRM conducted across 9 high-volume European centers showed that LRLR was associated with a shorter duration of surgery {median 200 [inter-quartile range (IQR) 123–273] vs. 256 [199–320] min; P <0.001}, less intraoperative blood loss [200 mL (50–450 mL) vs. 300 mL (100–600 mL); P=0.077] and a shorter postoperative hospital stay [5 days (3–8 days) vs. 6 days (5–8 days); P=0.028] (52). Postoperative morbidity and mortality rates were also similar after LRLR and ORLR. Nomi et al. analysed patients who underwent second and third LLR for recurrent CLRM, and found no significant differences in postoperative overall and major morbidity rates, as well as mortality rates (53). While these results seem to contradict guideline recommendations, a number of explanations exist. An initial LLR may result in minimal adhesions, thereby facilitating subsequent repeat procedures (54,55). Stretching of adhesion bands by pneumoperitoneum, together with a magnified laparoscopic view, enables meticulous adhesiolysis and dissection during RLR. Laparoscopy also requires a smaller working space (56), and some adhesions may be circumvented by laparoscopic equipment without compromising the operative view, thereby minimizing the need for extensive adhesiolysis (57-60).
Synchronous resection of CLRM
Increasing familiarity with minimally invasive abdominal surgery has allowed us to push the boundaries further, and some units even perform synchronous resection of colorectal and liver lesions in order to eliminate the need for two major operations and minimise the economic and psychological burden on the patient. In a systematic review of 12 studies analysing total laparoscopic synchronous resection (LSR) of CLRM, the LSR group had very encouraging outcomes, with a median operative time of 335.5 mins (range, 240–495), median bloodloss 266.5 mL (range, 50–500 mL), median LOS 8.3 days (range, 6–16.2 days) and postoperative morbidity of 19.9% (61). Ye et al. performed a meta-analysis of 10 retrospective studies involving 502 patients [216 minimally invasive (MIS), 286 open resections] who underwent synchronous resection (1). Unsurprisingly, the MIS approach was associated with less intraoperative blood loss (P=0.002) and blood transfusion (P=0.03), faster recovery of intestinal function (P=0.01) and diet (P<0.0001), shorter length of postoperative hospital stay (P<0.0001), and lower rates of surgical complications (P=0.04). The extent of liver resection during synchronous resection is a matter of contention. While most surgeons err on the side of caution and recommend that only minor hepatectomies should be performed in the same setting as a colectomy, some authors have recently demonstrated that simultaneous major liver resections can be performed with comparable outcomes to staged resection (62-64). In the systematic review by Moris et al. although the majority (83.6%) of cases were minor liver resections only, 4 comparative studies were included where synchronous major liver resections were performed with low conversion rates and similar morbidity and mortality outcomes compared to the open resection groups (65-68). Although there was significant heterogeneity amongst most of these studies, this provides early evidence of the safety and feasibility of LSR in selected cases.
Two-stage hepatectomy (TSH)
In the presence of extensive bilobar CLRM, an inadequate future remnant liver (FRL) is a contraindication to surgical resection. To circumvent this, Adam et al. introduced the concept of TSH in 2000 (69). Typically, the left liver lobe with lower disease burden is cleared in the first stage. The contralateral portal vein branches are occluded either by surgical ligation in the same surgery, or by post-operative radiological embolization. After an adequate time-interval to allow hypertrophy of the FLR, a standard or extended right hepatectomy is performed in the second stage. This was a remarkable breakthrough because it allowed patients who were formerly considered to have inoperable disease, to safely undergo liver resection and enjoy 32–70% 5-year OS (70,71). A number of case series demonstrated the safety and feasibility of performing LLR for the first stage procedure, with the advantages of minimal post-operative pain, short LOS, early commencement of chemotherapy, low morbidity and mortality rates, frequent progression to second stage surgery with no eventual compromise of oncologic results (72,73). The second stage surgery is more complex because it is technically a repeat hepatectomy, hence surgeons have to deal with post-operative adhesions, altered hepatic anatomy after initial resection and hypertrophy of the FRL, chemotherapy-induced liver injury and an inflamed porta hepatis following portal vein embolization/ligation which makes hilar dissection treacherous. Machado was the first to describe totally LLR for both stages (74). Gayet’s group reported their early experience with laparoscopic TSH, where almost 80% of patients completed the second stage, with 3- and 5-year OS and DFS rates of 78% and 41% and 26% and 13% respectively (75). Some years later, they compared outcomes following laparoscopic vs. open TSH in a bi-institutional, propensity-score matched study (76). LLR in the first stage was associated with shorter LOS (4 vs. 7.5 days; P<0.001), while in the second stage it resulted in lower blood loss (250 vs. 500 mL; P=0.040), fewer postoperative complications (32% vs. 60%; P=0.047), shorter LOS (9 vs. 16 days; P=0.013), and earlier administration of chemotherapy (1.6 vs. 2 months; P=0.039). Both groups had comparable OS, RFS and liver-recurrence-free survival, but RLR for recurrent disease was performed more frequently in the laparoscopic TSH group (56% vs. 0%; P=0.006). Fewer adhesions following a laparoscopic first-stage procedure, reduced bleeding due to pneumoperitoneum and magnified visualization of the surgical field were cited as some of the factors responsible for producing such positive outcomes in the MIS group (77).
Associating liver partition with portal vein ligation (ALPPS)
ALPPS is a relatively new surgical procedure developed to rapidly augment an insufficient FRL in the presence of high tumour load, and hepatectomy for CLRM is the commonest indication for this (78). A meta-analysis of 9 retrospective studies in patients with unresectable CLRM confirmed a faster kinetic growth rate of the FRL in ALPPS compared to TSH (79), while the LIGRO multicenter randomized control trial showed that ALPPS was associated with a higher resection rate, with no differences in morbidity, 90-day mortality or R0 resection rates compared to TSH (80). Initial enthusiasm surrounding ALPPS was curbed by reports citing high morbidity and mortality rates (81,82), which were subsequently systematically lowered by careful patient selection and adopting a less aggressive approach in stage-1 ALPPS (83). Using a minimally invasive approach for the first stage offers the benefits of reduced bloodloss, surgical trauma and inter-stage adhesions (84). A recent systematic review of 15 studies comparing MIS-ALPPS to the open procedure found that the laparoscopic patients experienced low morbidity rates (15.4% complications of Clavien-Dindo Grade 3b) and no procedure failures between the first and second stages, with 0% perioperative mortality after either stage (85).
‘Partial’ or ‘Mini’ ALPPS is another technical modification to minimize complications after stage 1. This entails strict avoidance of liver mobilization, ligation of the portal vein followed by partial transection of the liver parenchyma only halfway up to the middle hepatic vein which is preserved in order to maintain outflow and prevent congestion of the excluded liver segment. Truant et al. reported a series of 5 patients who underwent laparoscopic partial-ALPPS with impressive results of median FRL volume increase of +60% (+18.6% to +108.1%) and median FRL function increase of +47% (+37% to +64%) (83). These changes occurred earlier, allowing the second stage surgery to be done successfully within a week with no liver failure or deaths in their series. Another innovation that has been described combines MIS Mini-ALPPS with laparoscopic-assisted percutaneous cannulation of the inferior mesenteric vein (IMV) for embolization of the portal vein (instead of ligation) (86). Even ALPPS stage 2 may be performed laparoscopically, whereby the liver is fully mobilised, followed by division of inflow Glissonean pedicles and outflow veins using endostaplers (83). Although these procedures have all been described in highly selected patients, the encouraging results hint at the vast potential for expanded indications of laparoscopy in the surgical treatment of CLRM.
Limitations of LLR
Despite the plethora of advantages associated with minimally invasive liver resection, certain limitations still exist which must be acknowledged. These apply to the laparoscopic liver surgery regardless of the indication, and not just for resection of CLRM per se. When performing LLR, surgeons have to adapt to a caudal to cranial view as compared to the hepatic bird’s eye overview in OLR, hence lesions high up in the dome of the liver or in very lateral positions can be difficult to visualize (87). Laparoscopic instruments do not offer the same degree and freedom of movement as the human hand, thus liver mobilization may be difficult and hemorrhage can no longer be controlled manually. Despite modifications such as using 3D cameras with flexible tips or various devices like the Harmonic Scalpel (Ethicon Endosurgery, Cincinnati, OH, USA), Thunderbeat (Olympus, Tokyo, Japan), bipolar device (Biclamp, Erbe, Tuebingen, Germany) or even the laparoscopic Cavitron Ultrasonic Surgical Aspirator (CUSA) (Valleylab, Boulder, CO, USA), LLR remains a technically demanding undertaking with a steep learning curve (LC). Guilbaud et al. recently published a systematic review of 19 retrospective articles analysing the LC in LLR (88). 13 studies assessed the LC in real-life LLR, of which 7 used the cumulative sum (CUSUM) method, while 6 studies were undertaken using simulation and training programmes. The LC for minor hepatectomy ranged from 15−64 cases across studies, while for major resection an average of 50 cases were required (provided the surgeons were already proficient in minor LLR). Limitations of this review included the fact that most reports were single surgeon experiences only and there was significant heterogeneity in defining the endpoints for LC (operative time, conversion rate, bloodloss, morbidity). Furthermore, results may be skewed as more experienced surgeons tend to take on more difficult cases which would invariably affect the endpoint outcome. LC may also vary in different eras for self-taught pioneers vs. surgeons who had the benefit of receiving formalised training by established seniors. In the Southampton Consensus Guidelines, it is recommended that surgeons should embark on LLR only after completing formalised training via fellowships, courses or proctoring programmes (16). They should be comfortable with open liver resection and advanced laparoscopic surgery before starting LLR, and proceed in a stepwise manner with minor resections of lesions in anterolateral segments first before performing major hepatectomies. Tumours which are very large, situated close to major vessels or located in difficult posterosuperior segments [1, 4a, 7, 8] should be reserved for proficient operators only. Finally, these procedures should be ideally performed in high-volume liver centers where there are at least 2 or more surgeons with competency in LLR.
Another major factor prohibiting the rapid uptake of LLR is concerns about cost. Laparoscopic surgery requires usage of additional instruments which are usually disposable. Prolonged surgical times also contribute additional operating room and anesthetic charges. A systematic review of 11 manuscripts analyzing comparative costs of LLR and OLR was done as part of the Morioka consensus (89). This comprised of 443 laparoscopic resections, of which the majority (306/443 or 69%) were minor hepatectomies. Operating room costs were similar between laparoscopic and open hepatic resection in 7 studies; 1 study reported significantly lower costs in laparoscopic left lateral sectionectomy while 2 studies found higher operating room expenses in laparoscopic right hepatectomy. Most authors concluded that LOS was shorter after LLR which resulted in reduced hospital ward costs and subsequently, 7/11 articles demonstrated lower total hospital costs. In a recent study comparing 145 laparoscopic major hepatectomies (LMH) to 61 open major hepatectomies (OMH), on intention-to-treat analysis, higher intraoperative room expenses (+32.1%, P<0.001) of LMH were offset by postoperative savings (−27.2%, P=0.030), resulting in a global cost-neutrality (−7.2%, P=0.807) (90). This was largely attributed to reduced blood loss and blood transfusion rates, fewer complications requiring lesser additional post-operative investigations and medication and shorter LOS following laparoscopic resection. Taking into account the 14.5% conversion rate, a per-protocol analysis of the completed LMH showed fewer severe complications (P=0.042), interventional procedures (P=0.027) and lower readmission rates (P=0.031). Consequently, postoperative savings increased to −71.3% (P=0.003), resulting in a 29.9% cost advantage of completed LMH (P=0.020). One of the main limitations of existing studies on cost analysis of laparoscopic hepatectomies is that they are restricted only to the direct hospital costs, without considering indirect costs related to loss of productivity, return to work, caregiver expenses. Hence the true cost-effective of LLR may be under-estimated, especially if they allow patients to transition more quickly and smoothly back into their daily lives to resume their dedicated roles in society.
Future prospects
There is a paucity of high-quality, prospective data regarding the safety and feasibility of laparoscopic major hepatectomies, as well as LLR for lesions in difficult locations such as the right posterior sector or the venous outflow. To this end, two large, international, multi-center randomized trials are currently ongoing. The ORANGE II Plus study compares outcomes following laparoscopic vs. open right hepatectomy (91), while the ORANGE segments trial analyses laparoscopic compared to open liver resection for tumours involving segments 7, 8 or 4a (92). It remains to be seen if the results from these will be concordant with current evidence which is derived largely from retrospective studies.
Conclusions
After almost 3 decades, LLR for CLRM has been shown to produce superior perioperative and short-term results compared to OLR, with comparable oncologic and survival outcomes. As such, every aspiring liver surgeon should strive to include this requisite skill set in their technical armamentarium. This may be achieved by structured, rigorous training under the close supervision of experts from high-volume centers which presently exist in practically every continent. The surgical world eagerly awaits the results of prospective randomized trials currently underway to tackle important questions in order to further advance the management of this disease.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Nan Zun Teo, James Chi-Yong Ngu) for the series “Current Strategies in Colon Cancer Management” published in Journal of Gastrointestinal Oncology. The article was sent for external peer review organized by the Guest Editors and the editorial office.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jgo.2020.02.05). The series “Current Strategies in Colon Cancer Management” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ye SP, Qiu H, Liao SJ, et al. Mini-invasive vs. open resection of colorectal cancer and liver metastases: A meta-analysis. World J Gastroenterol 2019;25:2819-32. [Crossref] [PubMed]
- Cheng Y, Zhang L, Li H, et al. Laparoscopic vs. open liver resection for colorectal liver metastases: a systematic review. J Surg Res 2017;220:234-46. [Crossref] [PubMed]
- Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor. Surg Endosc 1992;6:97-8.
- Ciria R, Cherqui D, Geller DA, et al. Comparative Short-term Benefits of Laparoscopic Liver Resection: 9000 Cases and Climbing. Ann Surg 2016;263:761-77. [Crossref] [PubMed]
- Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg 2009;250:831-41. [Crossref] [PubMed]
- Zhou Y, Xiao Y, Wu L, et al. Laparoscopic liver resection as a safe and efficacious alternative to open resection for colorectal liver metastasis: a meta-analysis. BMC Surg 2013;13:44. [Crossref] [PubMed]
- Wei M, He Y, Wang J, et al. Laparoscopic vs. open hepatectomy with or without synchronous colectomy for colorectal liver metastasis: a meta-analysis PLoS One 2014;9:e87461. [Crossref] [PubMed]
- Luo LX, Yu ZY, Bai YN. Laparoscopic hepatectomy for liver metastases from colorectal cancer: a meta-analysis. J Laparoendosc Adv Surg Tech A 2014;24:213-22. [Crossref] [PubMed]
- Schiffman SC, Kim KH, Tsung A, et al. Laparoscopic vs. open liver resection for metastatic colorectal cancer: a meta analysis of 610 patients. Surgery 2015;157:211-22. [Crossref] [PubMed]
- Hallet J, Beyfuss K, Memeo R, et al. Short and long-term outcomes of laparoscopic compared to open liver resection for colorectal liver metastases. Hepatobiliary Surg Nutr 2016;5:300-10. [Crossref] [PubMed]
- Tian ZQ, Su XF, Lin ZY, et al. Meta-analysis of laparoscopic vs. open liver resection for colorectal liver metastases Oncotarget 2016;7:84544-55. [Crossref] [PubMed]
- Xie SM, Xiong JJ, Liu XT, et al. Laparoscopic Vs. Open Liver Resection for Colorectal Liver Metastases: A Comprehensive Systematic Review and Meta-analysis. Sci Rep 2017;7:1012. [Crossref] [PubMed]
- Zhang XL, Liu RF, Zhang D, et al. Laparoscopic vs. open liver resection for colorectal liver metastases: A systematic review and meta-analysis of studies with propensity score-based analysis. Int J Surg 2017;44:191-203. [Crossref] [PubMed]
- Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, et al. Laparoscopic vs. open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 2018;267:199-207. [Crossref] [PubMed]
- Robles-Campos R, Lopez-Lopez V, Brusadin R, et al. Open vs. minimally invasive liver surgery for colorectal liver metastases (LapOpHuva): a prospective randomized controlled trial. Surg Endosc 2019;33:3926-36. [Crossref] [PubMed]
- Abu Hilal M, Aldrighetti L, Dagher I, et al. The Southampton Consensus Guidelines for Laparoscopic Liver Surgery: From Indication to Implementation. Ann Surg 2018;268:11-8. [Crossref] [PubMed]
- Aghayan DL, Fretland ÅA, Kazaryan AM, et al. Laparoscopic vs. open liver resection in the posterosuperior segments: a sub-group analysis from the OSLO-COMET randomized controlled trial. HPB (Oxford) 2019;21:1485-90. [Crossref] [PubMed]
- Chen K, Pan Y, Hu GY, et al. Laparoscopic Vs. Open Major Hepatectomy for Hepatocellular Carcinoma: A Meta-Analysis. Surg Laparosc Endosc Percutan Tech 2018;28:267-74. [PubMed]
- Ciria R, Gomez-Luque I, Ocaña S, et al. A Systematic Review and Meta-Analysis Comparing the Short- and Long Term Outcomes for Laparoscopic and Open Liver Resections for Hepatocellular Carcinoma: Updated Results from the European Guidelines Meeting on Laparoscopic Liver Surgery, Southampton, UK, 2017. Ann Surg Oncol 2019;26:252-63. [Crossref] [PubMed]
- Ciria R, Ocaña S, Gomez-Luque I, et al. A systematic review and meta-analysis comparing the short- and long-term outcomes for laparoscopic and open liver resections for liver metastases from colorectal cancer. Surg Endosc 2020;34:349-60. [Crossref] [PubMed]
- Aloia T, Sebagh M, Plasse M, et al. Liver histology and surgical outcomes after preoperative chemotherapy with fluorouracil plus oxaliplatin in colorectal cancer liver metastases. J Clin Oncol 2006;24:4983-90. [Crossref] [PubMed]
- Zhao J, van Mierlo KMC, Gómez-Ramírez J, et al. Systematic review of the influence of chemotherapy-associated liver injury on outcome after partial hepatectomy for colorectal liver metastases. Br J Surg 2017;104:990-1002. [Crossref] [PubMed]
- Mala T, Edwin B, Gladhaug I, et al. A comparative study of the short-term outcome following open and laparoscopic liver resection of colorectal metastases. Surg Endosc 2002;16:1059-63. [Crossref] [PubMed]
- Qiu J, Chen S, Pankaj P, et al. Laparoscopic hepatectomy is associated with considerably less morbidity and a long-term survival similar to that of the open procedure in patients with hepatic colorectal metastases. Surg Laparosc Endosc Percutan Tech 2014;24:517-22. [PubMed]
- Fretland ÅA, Dagenborg VJ, Waaler Bjørnelv GM, et al. Quality of life from a randomized trial of laparoscopic or open liver resection for colorectal liver metastases. Br J Surg 2019;106:1372-80. [Crossref] [PubMed]
- Coelho FF, Kruger JA, Fonseca GM, et al. Laparoscopic liver resection: Experience based guidelines. World J Gastrointest Surg 2016;8:5-26. [Crossref] [PubMed]
- Uchiyama K, Ueno M, Ozawa S, et al. Combined use of contrast-enhanced intraoperative ultrasonography and a fluorescence navigation system for identifying hepatic metastases. World J Surg 2010;34:2953-9. [Crossref] [PubMed]
- Liu B, Liu T, Su M, et al. Improving the Surgical Effect for Primary Liver Cancer with Intraoperative Fluorescence Navigation Compared with Intraoperative Ultrasound. Med Sci Monit 2019;25:3406-16. [Crossref] [PubMed]
- Rossi G, Tarasconi A, Baiocchi G, et al. Fluorescence guided surgery in liver tumors: applications and advantages. Acta Biomed 2018;89:135-40. [PubMed]
- Terasawa M, Ishizawa T, Mise Y, et al. Applications of fusion-fluorescence imaging using indocyanine green in laparoscopic hepatectomy. Surg Endosc 2017;31:5111-8. [Crossref] [PubMed]
- Fretland ÅA, Aghayan D, Edwin B. Long-term survival after laparoscopic vs. open resection for colorectal liver metastases. J Clin Oncol 2019;37:LBA3516. [Crossref]
- Syn NL, Kabir T, Koh YX, et al. Survival Advantage of Laparoscopic Vs. Open Resection For Colorectal Liver Metastases: A Meta-analysis of Individual Patient Data From Randomized Trials and Propensity-score Matched Studies. Ann Surg 2019. [Epub ahead of print]. [Crossref]
- Goh BK, Chan CY, Wong JS, et al. Factors associated with and outcomes of open conversion after laparoscopic minor hepatectomy: initial experience at a single institution. Surg Endosc 2015;29:2636-42. [Crossref] [PubMed]
- Goh BKP, Lee SY, Teo JY, et al. Changing trends and outcomes associated with the adoption of minimally invasive hepatectomy: a contemporary single-institution experience with 400 consecutive resections. Surg Endosc 2018;32:4658-65. [Crossref] [PubMed]
- Goh BK, Teo JY, Lee SY, et al. Critical appraisal of the impact of individual surgeon experience on the outcomes of laparoscopic liver resection in the modern era: collective experience of multiple surgeons at a single institution with 324 consecutive cases. Surg Endosc 2018;32:1802-11. [Crossref] [PubMed]
- Kooby DA, Stockman J, Ben Porat L, et al. Influence of transfusions on perioperative and long-term outcome in patients following hepatic resection for colorectal metastases. Ann Surg 2003;237:860-9. [Crossref] [PubMed]
- Ito H, Are C, Gonen M, et al. Effect of Postoperative Morbidity on Long-term Survival After Hepatic Resection for Metastatic Colorectal Cancer. Ann Surg 2008;247:994-1002. [Crossref] [PubMed]
- Laurent C, Sa Cunha A, Couderc P, et al. Influence of postoperative morbidity on long-term survival following liver resection for colorectal metastases. Br J Surg 2003;90:1131-6. [Crossref] [PubMed]
- Montalti R, Berardi G, Laurent S, et al. Laparoscopic liver resection compared to open approach in patients with colorectal liver metastases improves further resectability: oncological outcomes of a case-control matched-pairs analysis. Eur J Surg Oncol 2014;40:536-44. [Crossref] [PubMed]
- Tohme S, Goswami J, Han K, et al. Minimally Invasive Resection of Colorectal Cancer Liver Metastases Leads to an Earlier Initiation of Chemotherapy Compared to Open Surgery. J Gastrointest Surg 2015;19:2199-206. [Crossref] [PubMed]
- Mbah N, Agle SC, Philips P, et al. Laparoscopic hepatectomy significantly shortens the time to postoperative chemotherapy in patients undergoing major hepatectomies. Am J Surg 2017;213:1060-4. [Crossref] [PubMed]
- Figueras J, Valls C, Rafecas A, et al. Resection rate and effect of postoperative chemotherapy on survival after surgery for colorectal liver metastases. Br J Surg 2001;88:980-5. [Crossref] [PubMed]
- Kawai T, Goumard C, Jeune F, et al. Laparoscopic liver resection for colorectal liver metastasis patients allows patients to start adjuvant chemotherapy without delay: a propensity score analysis. Surg Endosc 2018;32:3273-81. [Crossref] [PubMed]
- Fretland AA, Sokolov A, Postriganova N, et al. Inflammatory response after laparoscopic vs. open resection of colorectal liver metastases: data from the oslo-CoMet trial. Medicine (Baltimore) 2015;94:e1786. [Crossref] [PubMed]
- Krall JA, Reinhardt F, Mercury OA, et al. The systemic response to surgery triggers the outgrowth of distant immune-controlled tumors in mouse models of dormancy. Sci Transl Med 2018. [Crossref] [PubMed]
- Andersen BL, Farrar WB, Golden-Kreutz D, et al. Stress and immune responses after surgical treatment for regional breast cancer. J Natl Cancer Inst 1998;90:30-6. [Crossref] [PubMed]
- Ananth AA, Tai L-H, Lansdell C, et al. Surgical Stress Abrogates Pre-Existing Protective T Cell Mediated Anti-Tumor Immunity Leading to Postoperative Cancer Recurrence. PLoS One 2016;11:e0155947. [Crossref] [PubMed]
- Seth R, Tai LH, Falls T, et al. Surgical Stress Promotes the Development of Cancer Metastases by a Coagulation-Dependent Mechanism Involving Natural Killer Cells in a Murine Model. Ann Surg 2013;258:158-68. [Crossref] [PubMed]
- Syn NL, Teng MWL, Mok TSK, et al. De-novo and acquired resistance to immune checkpoint targeting. Lancet Oncol 2017;18:e731-41. [Crossref] [PubMed]
- Matsuoka H, Morise Z, Tanaka C, et al. Repeat hepatectomy with systemic chemotherapy might improve survival of recurrent livermetastasis from colorectal cancer-a retrospective observational study. World J Surg Oncol 2019;17:33. [Crossref] [PubMed]
- Wakabayashi T, Felli E, Memeo R, et al. Short-term outcomes of laparoscopic repeat liver resection after open liver resection: a systematic review. Surg Endosc 2019;33:2083-92. [Crossref] [PubMed]
- van der Poel MJ, Barkhatov L, Fuks D, et al. Multicentre propensity score-matched study of laparoscopic vs. open repeat liver resection for colorectal liver metastases. Br J Surg 2019;106:783-9. [Crossref] [PubMed]
- Nomi T, Fuks D, Ogiso S, et al. Second and third laparoscopic liver resection for patients with recurrent colorectal liver metastases. Ann Surg 2016;263:e68-e72. [Crossref] [PubMed]
- Gutt CN, Oniu T, Schemmer P, et al. Fewer adhesions induced by laparoscopic surgery? Surg Endosc 2004;18:898-906. [Crossref] [PubMed]
- Schäfer M. Krähenb hl L, Büchler MW. Comparison of adhesion formation in open and laparoscopic surgery. Dig Surg 1998;15:148-52. [Crossref] [PubMed]
- Morise Z. Status and perspective of laparoscopic repeat liver resection. World J Hepatol 2018;10:479-84. [Crossref] [PubMed]
- Goh BKP, Syn N, Teo JY, et al. Perioperative Outcomes of Laparoscopic Repeat Liver Resection for Recurrent HCC: Comparison with Open Repeat Liver Resection for Recurrent HCC and Laparoscopic Resection for Primary HCC. World J Surg 2019;43:878-85. [Crossref] [PubMed]
- Goh BKP, Teo JY, Chan CY, et al. Laparoscopic repeat liver resection for recurrent hepatocellular carcinoma. ANZ J Surg 2017;87:E143-6. [Crossref] [PubMed]
- Zhang J, Zhou ZG, Huang ZX, et al. Prospective, single-center cohort study analyzing the efficacy of complete laparoscopic resection on recurrent hepatocellular carcinoma. Chin J Cancer 2016;35:25. [Crossref] [PubMed]
- Goh BK, Teo JY, Chan CY, et al. Review of 103 Cases of Laparoscopic Repeat Liver Resection for Recurrent Hepatocellular Carcinoma. J Laparoendosc Adv Surg Tech A 2016;26:876-81. [Crossref] [PubMed]
- Moris D, Tsilimigras DI, Machairas N, et al. Laparoscopic synchronous resection of colorectal cancer and liver metastases: A systematic review. J Surg Oncol 2019;119:30-9. [Crossref] [PubMed]
- Martin RCG 2nd, Augenstein V, Reuter NP, et al. Simultaneous vs. staged resection for synchronous colorectal cancer liver metastases. J Am Coll Surg 2009;208:842-50. [Crossref] [PubMed]
- Reddy SK, Pawlik TM, Zorzi D, et al. Simultaneous resections of colorectal cancer and synchronous liver metastases: a multi-institutional analysis. Ann Surg Oncol 2007;14:3481-91. [Crossref] [PubMed]
- Muangkaew P, Cho JY, Han HS, et al. Outcomes of Simultaneous Major Liver Resection and Colorectal Surgery for Colorectal Liver Metastases. J Gastrointest Surg 2016;20:554-63. [Crossref] [PubMed]
- Jung KU, Kim HC, Cho YB, et al. Outcomes of simultaneous laparoscopic colorectal and hepatic resection for patients with colorectal cancers: a comparative study. J Laparoendosc Adv Surg Tech A 2014;24:229-35. [Crossref] [PubMed]
- Ratti F, Catena M, Di Palo S, et al. Impact of totally laparoscopic combined management of colorectal cancer with synchronous hepatic metastases on severity of complications: a propensity-score-based analysis. Surg Endosc 2016;30:4934-45. [Crossref] [PubMed]
- Gorgun E, Yazici P, Onder A, et al. Laparoscopic vs. open 1-stage resection of synchronous liver metastases and primary colorectal cancer. Gland Surg 2017;6:324-9. [Crossref] [PubMed]
- Xu X, Guo Y, Chen G, et al. Laparoscopic resections of colorectal cancer and synchronous liver metastases: a case controlled study. Minim Invasive Ther Allied Technol 2018;27:209-16. [Crossref] [PubMed]
- Adam R, Laurent A, Azoulay D, et al. Two-stage hepatectomy: a planned strategy to treat irresectable liver tumors. Ann Surg 2000;232:777-85. [Crossref] [PubMed]
- Narita M, Oussoultzoglou E, Jaeck D, et al. Two-stage hepatectomy for multiple bilobar colorectal liver metastases. Br J Surg 2011;98:1463-75. [Crossref] [PubMed]
- Pamecha V, Nedjat-Shokouhi B, Gurusamy K, et al. Prospective evaluation of two-stage hepatectomy combined with selective portal vein embolisation and systemic chemotherapy for patients with unresectable bilobar colorectal liver metastases. Dig Surg 2008;25:387-93. [Crossref] [PubMed]
- Di Fabio F, Whistance R, Rahman S, et al. Exploring the role of laparoscopic surgery in two-stage hepatectomy for bilobar colorectal liver metastases. J Laparoendosc Adv Surg Tech A 2012;22:647-50. [Crossref] [PubMed]
- Kilburn DJ, Chiow AK, Lewin J, et al. Laparoscopic approach to a planned two-stage hepatectomy for bilobar colorectal liver metastases. ANZ J Surg 2016;86:811-5. [Crossref] [PubMed]
- Machado MA, Makdissi FF, Surjan RC, et al. Two-stage laparoscopic liver resection for bilateral colorectal liver metastasis. Surg Endosc 2010;24:2044-7. [Crossref] [PubMed]
- Fuks D, Nomi T, Ogiso S, et al. Laparoscopic two-stage hepatectomy for bilobar colorectal liver metastases. Br J Surg 2015;102:1684-90. [Crossref] [PubMed]
- Okumura S, Goumard C, Gayet B, et al. Laparoscopic vs. open two-stage hepatectomy for bilobar colorectal liver metastases: A bi-institutional, propensity score-matched study. Surgery 2019;166:959-66. [Crossref] [PubMed]
- Teo NZ, Chong D, Goh BK. Minimally-invasive 2-stage liver resection with portal vein ligation for bil-lobar colorectal liver metastases. Surg Gastroeterol Oncol 2019;24:159-61.
- Schadde E, Ardiles V, Robles-Campos R, et al. ALPPS Registry Group. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Ann Surg 2014;260:829-36. [Crossref] [PubMed]
- Moris D, Ronnekleiv-Kelly S, Kostakis ID, et al. Operative Results and Oncologic Outcomes of Associating Liver Partition and Portal Vein Ligation for Staged Hepatectomy (ALPPS) Vs. Two-Stage Hepatectomy (TSH) in Patients with Unresectable Colorectal Liver Metastases: A Systematic Review and Meta-Analysis. World J Surg 2018;42:806-15. [Crossref] [PubMed]
- Sandström P, Røsok BI, Sparrelid E, et al. ALPPS Improves Resectability Compared With Conventional Two-stage Hepatectomy in Patients With Advanced Colorectal Liver Metastasis: Results From a Scandinavian Multicenter Randomized Controlled Trial (LIGRO Trial). Ann Surg 2018;267:833-40. [Crossref] [PubMed]
- Eshmuminov D, Raptis DA, Linecker M, et al. Meta-analysis of associating liver partition with portal vein ligation and portal vein occlusion for two-stage hepatectomy. Br J Surg 2016;103:1768-82. [Crossref] [PubMed]
- Adam R, Imai K, Castro Benitez C, et al. Outcome after associating liver partition and portal vein ligation for staged hepatectomy and conventional two-stage hepatectomy for colorectal liver metastases. Br J Surg 2016;103:1521-9. [Crossref] [PubMed]
- Lang H, de Santibañes E, Schlitt HJ, et al. 10th Anniversary of ALPPS-Lessons Learned and quo Vadis. Ann Surg 2019;269:114-9. [Crossref] [PubMed]
- Truant S, El Amrani M, Baillet C, et al. Laparoscopic Partial ALPPS: Much Better Than ALPPS! Ann Hepatol 2019;18:269-73. [Crossref] [PubMed]
- Melandro F, Giovanardi F, Hassan R, et al. Minimally Invasive Approach in the Setting of ALPPS Procedure: a Systematic Review of the Literature. J Gastrointest Surg 2019;23:1917-24. [Crossref] [PubMed]
- Pekolj J, Alvarez FA, Biagiola D, et al. Totally Laparoscopic Mini-ALPPS Using a Novel Approach of Laparoscopic-Assisted Transmesenteric Portal Vein Embolization. J Laparoendosc Adv Surg Tech A 2018;28:1229-33. [Crossref] [PubMed]
- Kabir T, Goh BK. Contemporary techniques commonly adopted for performing laparoscopic liver resection. Laparosc Surg 2018;2:61. [Crossref]
- Guilbaud T, Birnbaum DJ, Berdah S, et al. Learning Curve in Laparoscopic Liver Resection, Educational Value of Simulation and Training Programmes: A Systematic Review. World J Surg 2019;43:2710-9. [Crossref] [PubMed]
- Cleary SP, Han HS, Yamamoto M, et al. The comparative costs of laparoscopic and open liver resection: a report for the 2nd International Consensus Conference on Laparoscopic Liver Resection. Surg Endosc 2016;30:4691-6. [Crossref] [PubMed]
- Cipriani F, Ratti F, Cardella A, et al. Laparoscopic Vs. Open Major Hepatectomy: Analysis of Clinical Outcomes and Cost Effectiveness in a High-Volume Center. J Gastrointest Surg 2019;23:2163-73. [Crossref] [PubMed]
- ORANGE II PLUS - Trial: Open vs. Laparoscopic Hemihepatectomy. Available online: https://Clinicaltrials.gov/ct2/show/NCT01441856
- ORANGE SEGMENTS: Open vs. Laparoscopic Parenchyma Preserving Postero-Superior Liver Segment Resection. Available online: https://Clinicaltrials.gov/ct2/show/NCT03270917


