
A case of gastric small cell carcinoma with metastases to bone and liver
Introduction
Gastric neuroendocrine carcinomas (G-NECs) are a group of poorly differentiated high grade neuro-endocrine tumors, and can be either small-cell or large-cell NECs. Gastric small cell carcinomas (GSCC) are a subtype of G-NECs that typically arise in the upper one-third of the stomach (1,2) and have histologic features similar to those of small-cell lung carcinoma (SCLC) (1). GSCC’s have an aggressive natural history that is characterized by early and widespread metastases. Prognosis is universally dismal with most patients having an overall survival of less than 12 months. GSCC is rare, with only a few hundred cases reported to date. The epidemiological, clinical and treatment data is lacking for these patients and little is known about the prognostic and predictive factors.
We report a rare case of primary GSCC, pure type with metastases to the bone, liver and lymph nodes, in an African-American woman from the United States.
Case presentation
A 79-year-old African-American woman presented with two weeks of progressive dysphagia associated with nausea, vomiting, foreign body sensation in the throat and a 15-pound weight loss. She had no history of dark stools, diarrhea, flushing, or palpitations. She had never had an upper endoscopy or a colonoscopy. Physical examination was notable for mild epigastric tenderness.
Laboratory investigations on the day of admission showed elevated liver enzymes with Alkaline phosphatase of 235 U/L (normal range, 40–150 U/L), AST 166 U/L (normal range, 8–34 U/L), ALT 78 U/L (normal range, 6–55 U/L) and normal bilirubin levels. LDH was elevated at 348 U/L (normal range, 125–220 U/L). Calcium was 8.9 MG/DL (normal range 8.4–10.2 MG/DL). Complete blood count was unremarkable.
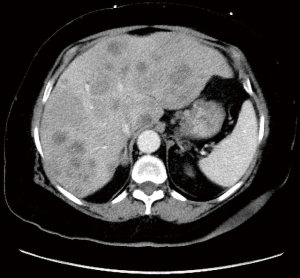
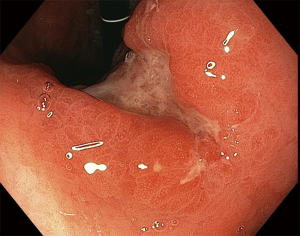
Computed tomography (CT) of the abdomen with contrast showed innumerable, ill-defined, hypodense lesions throughout the liver ranging from 1.1 to 3.1 cm. Several necrotic enlarged lymph nodes (2.7–3.1 cm × 1.9–2 cm) were seen in the gastro-hepatic ligament (Figure 1). Endoscopy revealed a single cratered and linear ulcer of size 8 cm × 1.5 cm seen on the lesser curvature of the stomach body 3 cm below the gastro-esophageal junction (Figure 2). Endoscopic ultrasound guided fine-needle aspiration was performed on the metastatic liver lesions. CT chest and MRI brain excluded any additional metastatic lesions.
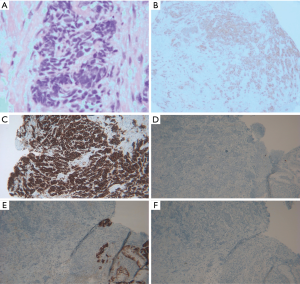
Gastric biopsy showed gastric mucosa with high-grade dysplasia and invasive small cell carcinoma (SCC) with necrosis. The tumor cells were positive for AE1/3, CK7, CD56, synaptophysin, E-cadherin, CDX2negative for chromogranin, CK20, TTF-1, WT1, mammaglobin, gcdfp-15 and PAX-8 by immune-histochemistry (IHC). Ki-67 was elevated to approximately 95%. The liver biopsy findings were consistent with GSCC suggestive of primary in the stomach (Figure 3).
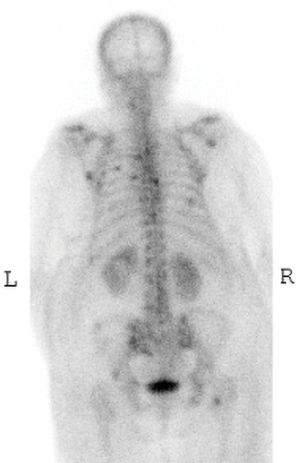
Palliative chemotherapy with cisplatin and etoposide was started for this stage IV GSCC. She presented a month later with back pain. Bone scan was done which showed multiple focal bony lesions at the thoracolumbar vertebrae, ribcage, bilateral scapulae, pelvic bones and right proximal femur consistent with multiple bony metastases (Figure 4). Patient completed 4 cycles of chemotherapy. Unfortunately with severe neutropenia and renal toxicity the patient decided for comfort care.
Discussion
Neuroendocrine tumors (NETs) are heterogeneous neoplasms, originating from the diffuse neuroendocrine cell system, distributed in a large variety of anatomical locations throughout the body and share a common neuroendocrine phenotype (3). In the gut and in the pancreas, these cells are located in the mucosa of the gastrointestinal tract or form islets in the pancreas. They derive from multipotent stem cells (4,5). SCC is a group of the most aggressive and highly malignant NETs, which are found in various locations, but arise most frequently from the lung.
Primary GSCC is an extremely rare NET found in <1% of all gastro-intestinal (GI) tract malignancies (3) and estimated to be even rarer, about 0.1% of all gastric cancer cases (4). Of the GI tract SCC cases, only about 11% to 20% are found in the stomach (3). It is most commonly seen in the Asian population, with the overwhelming majority of reported cases from China (5) and Japan which likely corresponds to higher incidence of gastric malignancy in that population. This cancer is reported to be three to five times more prevalent in men than women and average age of onset is greater than 60 (1). Less than twenty cases have been reported from the western hemisphere.
Clinically, GSCC is typically indistinguishable from the other histologic types of carcinoma of the stomach. Most patients present with epigastric discomfort, dysphagia, anemia and weight loss. In a case series of these patients it was observed that there was no significant difference in the incidence of epigastric discomfort (ranging from 47.83% to 80.00%) and dysphagia (ranging from 34.04% to 70.73%) when compared to patients with gastric adenocarcinoma. Some of the NETs can secrete hormones and amines, causing carcinoid syndrome and other clinical syndromes. However, GSCC is a type of non-functioning NET which may contribute to the late detection of such tumors and is usually diagnosed when the primary or metastatic lesions have grown large enough to cause symptoms.
GSCC most often metastasizes to the liver, followed by distant lymph nodes, bones, and bone marrow (3). On diagnoses most patients already have regional lymph node involvement and some have overt distant metastases (6). Also, GSCC can present with paraneoplastic syndromes associated with production of vasoactive intestinal peptide, gastrin but these presentations are rare (5,6).
Our case is one of the first to be identified in the western hemisphere with bone metastases. Bone metastases typically occurs in prostate, breast and lung cancer and is rare in all types of gastric cancer accounting for about 1% of all cases (7). Even in cases from Asia, we have been able to find only one case with metastases to the bone. Iwamuro et al. reported a 78-year-old Japanese male who presented with backache and was found to have metastatic GSCC to liver and bone (8). Brenner et al. did a retrospective study of 64 cases of the entire GI tract out of which they found 6 cases to have bone metastases. It wasn’t specified as to what the primary location of the tumor was in the GI tract (9).
Diagnostic methods are similar to those of the other histologic subtypes of gastric carcinoma with endoscopy being the preferred initial diagnostic test. However, GSCC has had a lower preoperative diagnostic rate likely because of small amount of tissue biopsied, frequent crush effect in the biopsy material, and the large number of cases that have composite histology (5). Imaging using CT is used especially in GSCC because of the likelihood of metastatic spread seen at presentation.
Under the microscope, GSCC is essentially indistinguishable from small cell lung cancer. GSCC is found to have sheets and nests of round fusiform cells with minimal cytoplasm and granular nuclear chromatin. Immunohistochemical staining with specific markers (chromogranin, synaptophysin and CD56) is used for diagnosis (3,6). It can be argued that differentiating primary GSCC and gastric metastasis from non-gastric SCC or poorly differentiated carcinoma is difficult to make. It is done by a combination of clinical and imaging characteristics with histology and IHC staining. In our case no other lesion was found including lung and brain on imaging studies. Also the markers that are usually positive in cancer with a pulmonary origin like TTF-1 were negative in our patient. GSCC has two histologic subtypes, pure and mixed. The pure-type only has features of SCC whereas the mixed or composite type has other histologic features as well, e.g., adenocarcinoma. The mixed variant is observed in 60–70% of cases (6,10). Our case was a pure-variant.
There is no universally accepted staging system for GSCC rendering comparison difficult between cases. There are two systems that are being used, the TNM system and the VALSG. The TNM system is the same staging system as that used for gastric cancer. The VALSG classifies tumors into limited disease (LD) which is a tumor within a localized anatomic region with or without lymph node involvement and extensive disease (ED) which is a tumor outside of the localized anatomic region (3,5,6).
GSCC has been found to have a dismal prognosis likely as most cases present with ED. The median survival is less than 12 months. The treatment used is similar to that of pulmonary small cell cancer. No randomized controlled trials have been done, likely because of the rarity of this disease. Therefore, the treatment protocols of GSCC have not been well established. For LD, patients undergo surgery and chemotherapy and for ED patients are treated with chemotherapy only, just like in most other malignancies. Chemotherapy used is with platinum-based compounds (3,5). Surgery and radiotherapy if used is used only for palliation (2). Genomic testing including p53, ERG rearrangement, CDX2 positivity, and SMARCA4 have been proposed for extrapulmonary SCCs and may be useful in future.
Conclusions
This report presented a case of gastric small cell cancer with metastases to the liver and the bone. This is one of the first cases in the western hemisphere to be reported with bone metastases. This case report shows the importance of having a full metastatic workup including a bone scan in such patients. More research needs to be conducted to identify optimal treatment regimens and prolong the overall survival in these patients.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
References
- Richards D, Davis D, Yan P, et al. Unusual case of small cell gastric carcinoma: case report and literature review. Dig Dis Sci 2011;56:951-7. [Crossref] [PubMed]
- Badger SA, Lee J, Vazir H, et al. Extra-pulmonary oat cell carcinoma: report of two cases. Ulster Med J 2005;74:63-5. [PubMed]
- Brenner B, Tang LH, Klimstra DS, et al. Small-cell carcinomas of the gastrointestinal tract: a review. J Clin Oncol 2004;22:2730-9. [Crossref] [PubMed]
- Bakogeorgos M, Kalkanis D, Katsaounis P, et al. Small cell carcinoma of the stomach: A report of two cases and a review of the literature. Mol Clin Oncol 2018;9:11-6. [PubMed]
- Wu QQ, Qiang WG, Wang F, et al. Management of primary gastric small cell carcinoma in China. Int J Clin Exp Med 2015;8:1589-97. [PubMed]
- Frances N, Zeichner SB, Francavilla M, et al. Gastric small-cell carcinoma found on esophagogastroduodenoscopy: a case report and literature review. Case Rep Oncol Med 2013;2013:475961.
- Ahn JB, Ha TK, Kwon SJ. Bone metastasis in gastric cancer patients. J Gastric Cancer. 2011;11:38-45. [Crossref] [PubMed]
- Iwamuro M, Tanaka S, Bessho A, et al. Two cases of primary small cell carcinoma of the stomach. Acta Med Okayama 2009;63:293-8. [PubMed]
- Brenner B, Shah MA, Gonen M, et al. Small-cell carcinoma of the gastrointestinal tract: a retrospective study of 64 cases. Br J Cancer 2004;90:1720-6. [Crossref] [PubMed]
- Toyokawa T, Tanaka H, Muguruma K, et al. Primary gastric small cell carcinoma: a series of seven cases. Anticancer Res 2015;35:563-7. [PubMed]


