|
References
- Wikipedia [Internet]. Florida: Wikimedia Foundation, Inc.; [cited 2010
Oct 15]. Available from: http://en.wikipedia.org/wiki/Obesity.[LinkOut]
- Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological
evidence and proposed mechanisms. Nat Rev Cancer 2004;4:579-91.[LinkOut]
- Larsson SC, Wolk A. Obesity and colon and rectal cancer risk: a metaanalysis
of prospective studies. Am J Clin Nutr 2007;86:556-65.[LinkOut]
- Sinicrope FA, Foster NR, Sargent DJ, O'Connell MJ, Rankin C. Obesity
is an independent prognostic variable in colon cancer survivors. Clin
Cancer Res 2010;16:1884-93.[LinkOut]
- Healy LA, Ryan AM, Sutton E, Younger K, Mehigan B, Stephens R,
et al. Impact of obesity on surgical and oncological outcomes in the
management of colorectal cancer. Int J Colorectal Dis 2010;25:1293-9.[LinkOut]
- Parr CL, Batty GD, Lam TH, Barzi F, Fang X, Ho SC, et al. Bodymass
index and cancer mortality in the Asia-Pacific Cohort Studies
Collaboration: pooled analyses of 424,519 participants. Lancet Oncol
2010;11:741-52.[LinkOut]
- Page C, Lin HJ, Jin Y, Ca st le VP, Nune z G, Huang M, et a l .
Overexpression of Akt/AKT can modulate chemotherapy-induced
apoptosis. Anticancer Res 2000;20:407-16.[LinkOut]
- Brognard J, Clark AS, Ni Y, Dennis PA. Akt/protein kinase B is
constitutively active in non-small cell lung cancer cells and promotes
cellular survival and resistance to chemotherapy and radiation. Cancer
Res 2001;61:3986-97.[LinkOut]
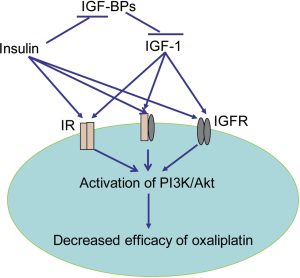
- Huang XF, Chen J. Obesity, the PI3K/Akt signal pathway and colon
cancer. Obes Rev 2009;10:610-6.[LinkOut]
- Gislette T, Chen J. The possible role of IL-17 in obesity-associated
cancer. ScientificWorldJournal 2010;10:2265-71.[LinkOut]
- Chen J. The Src/PI3K/Akt signal pathway may play a key role in
decreased drug efficacy in obesity-associated cancer. J Cell Biochem
2010;110:279-80.[LinkOut]
- Rose DP, Komninou D, Stephenson GD. Obesity, adipocytokines, and
insulin resistance in breast cancer. Obes Rev 2004;5:153-65.[LinkOut]
- Giovannucci E. Insulin and colon cancer. Cancer Causes Control
1995;6:164-79.[LinkOut]
- McKeown-Eyssen G. Epidemiology of colorectal cancer revisited: are
serum triglycerides and/or plasma glucose associated with risk? Cancer
Epidemiol Biomarkers Prev 1994;3:687-95.[LinkOut]
- Kaaks R, Toniolo P, Akhmedkhanov A, Lukanova A, Biessy C, Dechaud
H, et al. Serum C-peptide, insulin-like growth factor (IGF)-I, IGFbinding
proteins, and colorectal cancer risk in women. J Natl Cancer
Inst 2000;92:1592-600.[LinkOut]
- Ma J, Giovannucci E, Pollak M, Leavitt A, Tao Y, Gaziano JM, et al. A
prospective study of plasma C-peptide and colorectal cancer risk in
men. J Natl Cancer Inst 2004;96:546-53.[LinkOut]
- Wei EK, Ma J, Pollak MN, Rifai N, Fuchs CS, Hankinson SE, et al. A
prospective study of C-peptide, insulin-like growth factor-I, insulinlike
growth factor binding protein-1, and the risk of colorectal cancer in
women. Cancer Epidemiol Biomarkers Prev 2005;14:850-5.[LinkOut]
- Gunter MJ, Hoover DR, Yu H, Wassertheil-Smoller S, Rohan TE,
Manson JE, et al. Insulin, insulin-like growth factor-I, endogenous
estradiol, and risk of colorectal cancer in postmenopausal women.
Cancer Res 2008;68:329-37.[LinkOut]
- Tran TT, Medline A, Bruce WR. Insulin promotion of colon tumors in
rats. Cancer Epidemiol Biomarkers Prev 1996;5:1013-5.[LinkOut]
- Tran TT, Naigamwalla D, Oprescu AI, Lam L, McKeown-Eyssen G,
Bruce WR, et al. Hyperinsulinemia, but not other factors associated
with insulin resistance, acutely enhances colorecta l epithelia l
proliferation in vivo. Endocrinology 2006;147:1830-7.[LinkOut]
- Lasko CM, Bird RP. Modulation of aberrant crypt foci by dietary fat
and caloric restriction: the effects of delayed intervention. Cancer
Epidemiol Biomarkers Prev 1995;4:49-55.[LinkOut]
- Chen J. Is Src the key to understanding metastasis and developing new
treatments for colon cancer? Nat Clin Pract Gastroenterol Hepatol
2008;5:306-7.[LinkOut]
- Ozes ON, Mayo LD, Gustin JA, Pfeffer SR, Pfeffer LM, Donner DB. NFkappaB
activation by tumour necrosis factor requires the Akt serinethreonine
kinase. Nature 1999;401:82-5.[LinkOut]
- Wullschleger S, Loewith R, Hall MN. TOR signaling in growth and
metabolism. Cell 2006;124:471-84.[LinkOut]
- Keku TO, Lund PK, Galanko J, Simmons JG, Woosley JT, Sandler RS.
Insulin resistance, apoptosis, and colorectal adenoma risk. Cancer
Epidemiol Biomarkers Prev 2005;14:2076-81.[LinkOut]
- Goodwin PJ, Pritchard KI, Ennis M, Clemons M, Graham M, Fantus
IG. Insulin-lowering effects of metformin in women with early breast
cancer. Clin Breast Cancer 2008;8:501-5.[LinkOut]
- Goodwin PJ, Ligibel JA, Stambolic V. Metformin in breast cancer: time
for action. J Clin Oncol 2009;27:3271-3.[LinkOut]
- Wolpin BM, Meyerhardt JA, Chan AT, Ng K, Chan JA, Wu K, et al.
Insulin, the insulin-like growth factor axis, and mortality in patients
with nonmetastatic colorectal cancer. J Clin Oncol 2009;27:176-85.[LinkOut]
- Adlard JW, Richman SD, Seymour MT, Quirke P. Prediction of the response of colorectal cancer to systemic therapy. Lancet Oncol
2002;3:75-82.[LinkOut]
- Saif MW, Choma A, Salamone SJ, Chu E. Pharmacokinetically guided
dose adjustment of 5-f luorouracil: a rational approach to improving
therapeutic outcomes. J Natl Cancer Inst 2009;101:1543-52.[LinkOut]
- Kelland L. The resurgence of platinum-based cancer chemotherapy. Nat
Rev Cancer 2007;7:573-84.[LinkOut]
- Wakasugi T, Izumi H, Uchiumi T, Suzuki H, Arao T, Nishio K, et
al. ZNF143 interacts with p73 and is involved in cisplatin resistance
through the transcriptional regulation of DNA repair genes. Oncogene
2007;26:5194-203.[LinkOut]
- Torigoe T, Izumi H, Ishiguchi H, Yoshida Y, Tanabe M, Yoshida T,
et al. Cisplatin resistance and transcription factors. Curr Med Chem
Anticancer Agents 2005;5:15-27.[LinkOut]
- Chen J, Raymond K. Nuclear receptors, bile-acid detoxification, and
cholestasis. Lancet 2006;367:454-6.[LinkOut]
- Ekblad L, Kjellstrom J, Johnsson A. Reduced drug accumulation
is more important in acquired resistance against oxaliplatin than
against cisplatin in isogenic colon cancer cells. Anticancer Drugs
2010;21:523-31.[LinkOut]
- Lee W, Belkhiri A, Lockhart AC, Merchant N, Glaeser H, Harris EI, et
al. Overexpression of OATP1B3 confers apoptotic resistance in colon
cancer. Cancer Res 2008;68:10315-23.[LinkOut]
- Kopetz S, Lesslie DP, Dallas NA, Park SI, Johnson M, Parikh NU, et al.
Synergistic activity of the SRC family kinase inhibitor dasatinib and
oxaliplatin in colon carcinoma cells is mediated by oxidative stress.
Cancer Res 2009;69:3842-9.[LinkOut]
- Boyer J, Allen WL, McLean EG, Wilson PM, McCulla A, Moore S, et al.
Pharmacogenomic identification of novel determinants of response to
chemotherapy in colon cancer. Cancer Res 2006;66:2765-77.[LinkOut]
- Plasencia C, Martinez-Balibrea E, Martinez-Cardus A, Quinn DI, Abad
A, Neamati N. Expression analysis of genes involved in oxaliplatin
response and development of oxaliplatin-resistant HT29 colon cancer
cells. Int J Oncol 2006;29:225-35.[LinkOut]
- Iwatsuki M, Mimori K, Yokobori T, Tanaka F, Tahara K, Inoue H, et al.
A platinum agent resistance gene, POLB, is a prognostic indicator in
colorectal cancer. J Surg Oncol 2009;100:261-6.[LinkOut]
- Vie N, Copois V, Bascoul-Mollevi C, Denis V, Bec N, Robert B, et al.
Overexpression of phosphoserine aminotransferase PSAT1 stimulates
cell growth and increases chemoresistance of colon cancer cells. Mol
Cancer 2008;7:14.[LinkOut]
- Hector S, Bolanowska-Higdon W, Zdanowicz J, Hitt S, Pendyala L.
In vitro studies on the mechanisms of oxaliplatin resistance. Cancer
Chemother Pharmacol 2001;48:398-406.[LinkOut]
- Pollak M. Insulin and insulin-like growth factor signalling in neoplasia.
Nat Rev Cancer 2008;8:915-28.[LinkOut]
- Douglas JB, Silverman DT, Pollak MN, Tao Y, Soliman AS, Stolzenberg-
Solomon RZ. Serum IGF-I, IGF-II, IGFBP-3, and IGF-I/IGFBP-3
molar ratio and risk of pancreatic cancer in the prostate, lung, colorectal,
and ovarian cancer screening trial. Cancer Epidemiol Biomarkers Prev
2010;19:2298-306.[LinkOut]
- Wei EK, Ma J, Pollak MN, Rifai N, Fuchs CS, Hankinson SE, et al. A
prospective study of C-peptide, insulin-like growth factor-I, insulinlike
growth factor binding protein-1, and the risk of colorectal cancer in
women. Cancer Epidemiol Biomarkers Prev 2005;14:850-5.[LinkOut]
- Palmqvist R, Hallmans G, Rinaldi S, Biessy C, Stenling R, Riboli E,
et al. Plasma insulin-like growth factor 1, insulin-like growth factor
binding protein 3, and risk of colorectal cancer: a prospective study in
northern Sweden. Gut 2002;50:642-6.[LinkOut]
- Ma J, Giovannucci E, Pol lak M, Stampfer M. RESPONSE: Re: Prospective Study of Colorectal Cancer Risk in Men and Plasma Levels
of Insulin-Like Growth Factor (IGF)-I and IGF-Binding Protein-3. J
Natl Cancer Inst 1999;91:2052.[LinkOut]
- Giovannucci E, Pollak MN, Platz EA, Willett WC, Stampfer MJ, Majeed
N, et al. A prospective study of plasma insulin-like growth factor-1 and
binding protein-3 and risk of colorectal neoplasia in women. Cancer
Epidemiol Biomarkers Prev 2000;9:345-9.[LinkOut]
Cite this article as:
Chen J, Huang X, Qiao L, Katsifis A. Insulin caused drug resistance to oxaliplatin in colon cancer cell line HT29. J Gastrointest Oncol. 2011;2(1):27-33. DOI:10.3978/j.issn.2078-6891.2010.028
|