Medical record review of transition to lanreotide following octreotide for neuroendocrine tumors
Introduction
Neuroendocrine tumors (NETs), a relatively rare group of neoplasms derived from cells of the endocrine and nervous systems, occur most commonly in the intestine, where they have traditionally been called carcinoid tumors. However, NETs are also found in the pancreas, lung, and other organs (1). These heterogeneous tumors are classified by the primary tumor site, grade, and functional status. As most NETs are slow growing and lack obvious symptoms, they often present with locally advanced or metastatic disease by the time patients are accurately diagnosed (2-4). The overall median survival of patients with NETs is estimated to be 9.3 years, but survival varies considerably by tumor stage and grade (1). For patients with localized tumors, overall median survival is estimated to be >30 years. For patients with advanced disease, overall survival is lower and varies by disease site, but median survival has been increasing in recent years due to the introduction of more effective therapeutic options (1).
Short-acting octreotide has a role as “rescue” therapy in patients with breakthrough symptoms on therapeutic doses of long-acting somatostatin analogs (SSAs), and its use for this purpose has been shown to be safe and effective (5-8). In the United States (US), both lanreotide and octreotide are recommended as treatment options for patients with clinically significant metastatic disease (6). Octreotide has previously been established in a randomized controlled trial, PROMID, to have an antiproliferative effect on midgut grade 1 neuroendocrine tumors (3,6,9). In 2014, the Controlled Study of Lanreotide Antiproliferative Response in Neuroendocrine Tumors (CLARINET) study found that lanreotide significantly improved progression-free survival (PFS) compared with placebo in treatment-naïve patients with grade 1 or 2 enteropancreatic (midgut, pancreas, or unknown origin) tumors irrespective of hepatic tumor load (10). Estimated median PFS rates at 24 months were 65.1% (95% CI: 54.0% to 74.1%) for lanreotide compared with 33.1% (95% CI: 23.0% to 43.3%) for placebo (10). The median PFS in an open-label extension study for CLARINET was 38.5 months (95% CI: 30.9 to 59.4 months)(11). A prespecified subgroup analysis revealed the median PFS was 29.7 months (95% CI: 12.0 to 38.5) for patients with pancreatic NETs and 61.5 months [95% CI: 30.9 to not estimable (NE)] for patients with midgut NETs (11). In the ELECT trial, which evaluated lanreotide against placebo (with access to short-acting octreotide as rescue medication) and included both octreotide-naïve patients and those who had received prior octreotide treatment, the primary endpoint was use of short-acting octreotide as rescue medication. Results from this trial showed that lanreotide was effective in controlling carcinoid symptoms irrespective of prior exposure to octreotide (12). In a subgroup analysis restricted to patients previously treated with octreotide, improvement was observed in the control of carcinoid symptoms with lanreotide relative to placebo; however, statistical significance was not reached (13).
While both SSAs are indicated as treatment options for NET, additional factors such as effective symptom control, tolerability, ease of administration, and cost may affect treatment decisions. Octreotide requires reconstitution and is administered intramuscularly, whereas lanreotide is provided in a prefilled syringe and is administered as a deep subcutaneous injection (14,15). Given the differences in indication, perceived differences in administration convenience (16) and relatively recent approval of lanreotide, clinicians and patients may consider sequencing SSA therapy from octreotide to lanreotide. Understanding treatment-sequencing patterns is important for clinical decision-making but also has implications for assessments of value to the health care system. However, current real-world data on patients who transitioned from octreotide to lanreotide are limited. Therefore, we sought to evaluate clinical outcomes among patients with GEP-NET who had transitioned from long-acting octreotide monotherapy to lanreotide monotherapy in routine clinical practice.
Methods
Study design
We conducted a multicenter, noninterventional, retrospective medical record review of patients who had a confirmed diagnosis of locally advanced or metastatic GEP-NET (NCT03112694). Our primary aim was to describe the clinical course of transitioning patients from long-acting octreotide to lanreotide therapy. Abstractors entered the patient demographic and clinical data into a customized, web-based, case report form. Data were then compiled into a patient-level analytic file. Only anonymous data were collected for use in this study. The study was reviewed and approved by the institutional review boards (IRBs) of participating sites, including RTI International’s IRB, per individual site policies.
Population
Eligible patients were aged 18 years or older with a confirmed diagnosis of locally advanced or metastatic GEP-NET who sequenced treatment from long-acting octreotide to lanreotide. Data from the medical records of 93 patients who received treatment were abstracted at six US-based sites between April 2017 and October 2017. Patients must have received treatment with long-acting octreotide for at least 90 days before transitioning to lanreotide and to have received lanreotide for at least 90 days after the transition. Patients were excluded if they had been enrolled in a clinical trial for GEP-NET, had a history of other malignant disease (except basal cell carcinoma or carcinoma in situ of the cervix), were being treated with an SSA in combination with NET treatments other than immediate release (IR) subcutaneous octreotide, received other primary treatment (e.g., targeted therapy, chemotherapy, liver-directed therapy) for GEP-NET, or had a familial NET syndrome. After further review of data, two patients who were reported to have received liver-directed therapy while on treatment with lanreotide or within 60 days before the start of lanreotide monotherapy were excluded from the analysis; therefore, the final study population comprised 91 patients.
Study measures
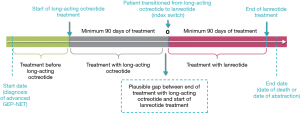
To capture the full range of clinical responses before, during, and after treatment with lanreotide, we collected data during three periods of variable duration (Figure 1). In addition, symptoms and other recorded adverse events (AE) were examined during each assessment period. Patients were considered to have functional disease if their tumors secreted bioactive substances and hormones leading to clinical symptoms (i.e., diarrhea and flushing), and patients without such tumors were considered to have nonfunctional disease.
Outcomes of tumor assessments, clinical evaluation of disease status, and clinician-defined PFS were assessed after patients were transitioned to lanreotide. Clinical evaluations of disease status, including progression, were made by individual physicians according to their routine practice and were not dictated by formal criteria [e.g., Response Evaluation Criteria in Solid Tumors (RECIST) criteria]. The analysis was stratified by disease status at the transition point (progressive disease, nonprogressive disease, or unknown status). Patients were considered to have progressive disease if it was the reported reason for transitioning treatment. In addition, patients whose disease status at the time of switch was not reported as responsive, stable disease, or unknown were considered to have progressive disease.
Patient demographics and baseline clinical characteristics at the initial diagnosis of GEP-NET and at diagnosis of locally advanced or metastatic disease were tabulated; treatment and outcome measures are reported during the periods of treatment with long-acting octreotide and lanreotide.
Statistical analyses
We descriptively evaluated continuous variables and frequency distributions for categorical variables (17,18). Clinician-defined PFS was estimated using the Kaplan-Meier method (19). Differences in the proportion of patients with symptoms while being treated with octreotide versus lanreotide were assessed using McNemar tests. All analyses were conducted using SAS (version 9.4) statistical software (SAS Institute Inc., Cary, North Carolina).
Results
Patient and clinical characteristics
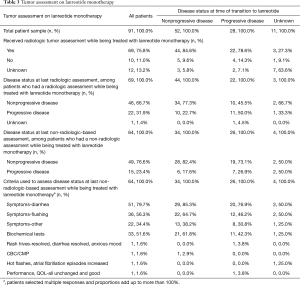
At initial diagnosis of GEP-NET, 65 (71.4%) of the 91 patients included in the study had stage IV disease (Table 1). The stage of disease was unknown for nearly all other patients [20 (22.0%)] included in the study. Small intestine [58 (63.7%)] and pancreas [13 (14.3%)] were the most common primary tumor sites. The mean [standard deviation (SD)] total duration of follow-up from diagnosis of locally advanced or metastatic disease to the earlier of death or date of data abstraction was 70.6 (41.3) months, with a minimum follow-up of 9.2 months.
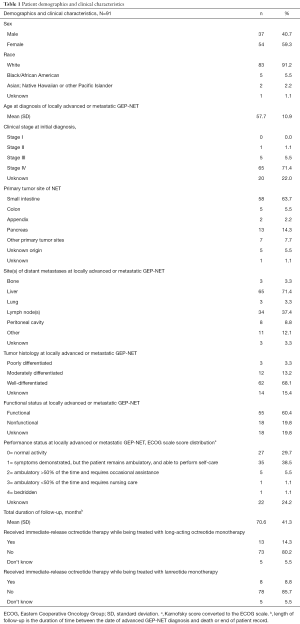
Full table
At diagnosis of locally advanced or metastatic GEP-NET, the mean (SD) age of patients was 57.7 (10.9) years. Of the 91 patients, 83 (91.2%) patients were white and 54 (59.3%) were female. Sixty-two (68.2%) had an Eastern Cooperative Oncology Group performance status score or converted Karnofsky score of either 0 or 1. The most common sites of metastases were liver [65 patients (71.4%)], lymph nodes [34 (37.4%)], and peritoneal cavity [8 (8.8%)]. Patients with well-differentiated tumors [62 (68.1%)] constituted the majority, followed by those with moderately differentiated tumors; histology was unknown for 14 (15.4%) patients. Functional disease was present in 55 (60.4%) patients and the functional status was not known for 18 (19.8%) patients.
Treatments before lanreotide
Only 23 of 91 patients (25.3%) had received another treatment prior to starting long-acting octreotide for locally advanced or metastatic GEP-NET; for 68 patients (74.7%), long-acting octreotide monotherapy was the initial systemic treatment. Patients began treatment with long-acting octreotide a mean (SD) of 17.0 (24.7) months after initial diagnosis. During the period between initial diagnosis and the start of long-acting octreotide treatment, most patients [67 (73.6%)] did not receive immediate release (IR) octreotide therapy and about half [43 (47.3%)] had surgery, while few patients (4) received chemotherapy or targeted therapy (2).
Patients received long-acting octreotide for a mean (SD) of 38.4 (32.8) months. At the start of treatment, most patients received 30 mg of long-acting octreotide every 4 weeks [65 (71.4%)], while 20 (22.0%) patients received 20 mg every 4 weeks. Immediately before transitioning to lanreotide monotherapy, the dose of long-acting octreotide was 30 mg every 4 weeks for 59 (64.8%) patients, 20 mg every 4 weeks for 10 (11.0%) patients, 30 mg every 2 weeks for 8 (8.8%) patients, and 40 mg every 4 weeks for 6 (6.6%) patients. Along with long-acting octreotide, 13 (14.3%) patients also received IR octreotide therapy (Table 1), with a mean (SD) total daily dose of 357.7 (269.1) µg. While being treated with long-acting octreotide, 75 (82.4%) patients received a radiologic assessment, and 48 (64.0%) patients had nonprogressive disease at the last radiologic assessment before the transition to lanreotide.
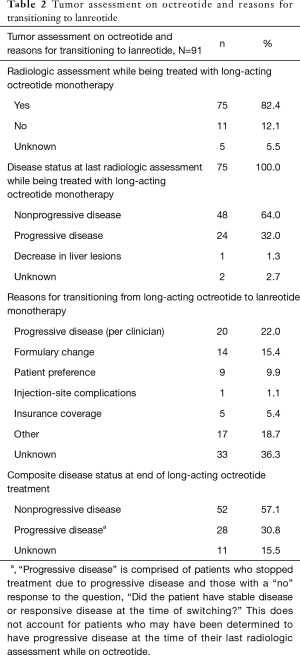
Transition to lanreotide
At the time of their transition to lanreotide, 52 (57.1%) patients had nonprogressive disease; 28 (30.8%) patients had progressive disease, and the remainder had unknown disease status (Table 2). The most common known reasons for switching from octreotide to lanreotide were progressive disease [20 patients (22.0%)], formulary change [14 (15.4%)], and patient preference [9 (9.9%)]. More than one-third of patients [33 (36.3%)] did not have a documented reason for switching from long-acting octreotide monotherapy to lanreotide monotherapy.
Full table
Treatment with lanreotide
Table 3 presents the primary outcomes. Sixty-nine of the 91 patients (75.8%) included in the study had a radiologic assessment such as magnetic resonance imaging (MRI) or computed tomography (CT) scan while being treated with lanreotide. The mean (SD) time from start of lanreotide to last radiologic assessment was 10.0 (8.9) months and from last radiologic assessment to last medical record date (if treatment was ongoing) or discontinuation of lanreotide was 3.1 (2.9) months. At the last radiologic assessment, 46 (66.7%) patients had nonprogressive disease, while 22 (31.9%) had progressive disease.
Full table
Among the 52 patients who were assessed to have clinician-assessed nonprogressive disease at the time they transitioned to lanreotide, 44 (84.6%) had a subsequent radiological assessment. Many of these patients continued to have nonprogressive disease [34 (77.3%)] at the last radiologic assessment while on lanreotide.
Among the 28 patients with clinician-assessed progressive disease at the time they transitioned to lanreotide, 22 (78.6%) had subsequent radiological assessment. Of the 22 who had a radiologic assessment after mean (SD) time of 10.6 (7.3) months following transition to lanreotide, 10 (45.5%) had stable disease and 1 had unknown disease status. The other 11 patients had progressive disease. Among the 26 patients who had clinician-assessed progressive disease at the time of transition to lanreotide and who had a non-radiologic tumor assessment subsequently, most had nonprogressive disease [19 (73.1%)].
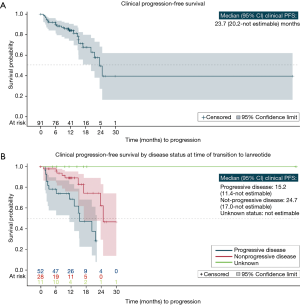
Table 4 presents clinician-assessed progression data for patients treated with lanreotide. During treatment, 22 patients (24.2%) experienced disease progression. The median (95% CI) clinician-defined PFS following treatment with lanreotide was estimated to be 23.7 months (20.2 months to NE), and the clinician-defined 24-month PFS rate (standard error) was estimated to be 49.5% (0.11%) (Figure 2A). Among patients who had clinician-defined progressive disease at the time of transitioning to lanreotide, the median (95% CI) clinician-defined PFS was estimated to be 15.2 months (11.4 months to NE) (Table 4; Figure 2B), while among patients who had nonprogressive disease at the time of transitioning to lanreotide, the median (95% CI) clinician-defined PFS was 24.7 months (17.0 months to NE). Estimates for duration of response following treatment with lanreotide (including treatment discontinuation due to AE as an event, along with clinician-defined progression and death) were similar to those of clinician-defined PFS (Table 4).

Full table
The median (95% CI) duration of treatment with lanreotide was estimated to be 24.7 (16.7−59.9) months. At the end of follow-up, 67 of the 91 patients in the study were still receiving lanreotide treatment. The 24 patients who stopped treatment with lanreotide received it for mean (SD) duration of 12.4 (12.3) months. At the start of treatment, all but 4 patients received 120 mg of lanreotide every 4 weeks. Only 4 patients increased either the dose or frequency of lanreotide and those who did increased only once. Among patients who discontinued treatment with lanreotide, 6 restarted lanreotide with additional NET treatment, 3 stopped treatment due to progressive disease, 3 reported that patient decision was the reason for stopping lanreotide, 2 patients died and 4 were lost to follow-up.
Symptoms and other adverse events
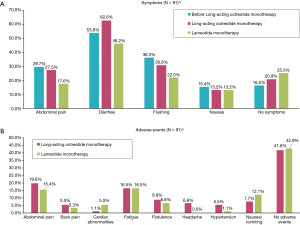
Descriptive statistics comparing symptoms experienced by patients during the three defined treatment periods are presented in Figure 3A. Diarrhea was the most commonly reported symptom during all treatment periods. While taking lanreotide, fewer patients [42 (46.2%)] were reported to experience diarrhea than while taking octreotide [57 (62.6%)] (P=0.001). The next most common symptom experienced during long-acting octreotide was flushing [28 (30.8%)]. Fewer patients were reported to experience flushing and abdominal pain during treatment with lanreotide than during long-acting octreotide therapy [flushing: 20 (22.0%) versus 28 (30.8%), P=0.021]; abdominal pain: [16 (17.6%) versus 25 (27.5%), P=0.020]; however, follow-up time differed between the two phases. At diagnosis of locally advanced or metastatic GEP-NET, functional disease was reported in 55 (60.4%) patients who eventually transitioned from octreotide to lanreotide, but functional status was not known for 19.8% of patients. Among the 55 patients reported to have functional disease, 47 (85.5%) and 42 (76.4%) were reported to have experienced any symptoms while taking octreotide and lanreotide, respectively. During treatment with long-acting octreotide alone, abdominal pain [18 (19.8%)], fatigue [15 (16.5%)], and flatulence [8 (8.8%)] were the most common AEs reported (Figure 3B). While being treated with lanreotide, fatigue [15 (16.5%)], abdominal pain [14 (15.4%)], and nausea/vomiting [11 (12.1%)] were the most common AEs reported.
Discussion
We reviewed the medical records of 91 patients with locally advanced or metastatic GEP-NET who transitioned from octreotide to lanreotide for a variety of reasons, including physician decision, changes in formulary coverage, and patient preference. Outcomes were evaluated among patients who had progressive disease and patients who had nonprogressive disease at the point of transition to lanreotide therapy.
Among patients who were reported to have progressive disease when they transitioned to lanreotide, the median (95% CI) clinician-defined PFS of 15.2 months (11.4 months to NE) months reported here aligns with the findings of a retrospective case series reported by Fong et al. (20) In that study, the mean duration of response was 15 months among patients with NETs who were sequenced to lanreotide after octreotide. A similar study by Saif et al. (21) found lanreotide to be safe and well tolerated. Most patients in these studies were responsive to lanreotide treatment and had either stable or decreased biomarker levels after making the transition to lanreotide. In both studies, lanreotide was found to be well tolerated.
In our study, 26 patients who were reported as having progressive disease at transition were reported as having nonprogressive disease after the transition. Ten of these patients (38.5%) were reported to have disease stabilization based on radiologic assessment. This finding was unexpected because the two agents have similar mechanisms of action. Typically, disease control would not be expected without adding agents with a different mode of action (i.e., combination therapy).
While our primary aim was to describe the clinical course of transitioning patients from octreotide to lanreotide therapy, our secondary finding that some patients experienced disease stabilization after the treatment transition warrants further examination. Although there are some biochemical similarities between the two medications, they are not identical (22,23), and it is possible that lanreotide’s route of administration might account for the disease stabilization experienced by some patients. Previous research on mode of administration showed that only 52% of octreotide doses were successfully delivered to the muscle, as assessed by computed tomography of the injection site (24). In contrast, a comparative study among nurses found that deep subcutaneous injection of lanreotide delivery was convenient and that, more importantly, it resulted in greater confidence that the full dose was delivered (16). In a small cohort study, lanreotide’s deep subcutaneous mode of administration was shown to offer similar bioavailability as its intramuscular mode, when injected by mistake, whereas subcutaneous injection provided slightly better late-phase release and a better overall long-term release profile (25). Further, the autoinjector had a low clogging risk (26).
In addition, despite their similar mechanism of action, octreotide and lanreotide have been shown to have different pharmacokinetic profiles (22) and different affinities for somatostatin receptors (23). It has been suggested that patients refractory to one SSA may respond to another (23). Most of the patients in our study were on the recommended 30 mg/mo dose of long-acting octreotide (6) immediately before the transition to lanreotide; however, some patients in our study received IR octreotide therapy and had experienced dose escalation prior to the switch, presumably due to inadequate symptom control. Dose escalations of long-acting octreotide above the recommended dose are common in cases of refractory carcinoid syndrome (23,27). Analysis of Medicare data found that 86 of 355 patients (24%) with NETs who were taking octreotide required a dose escalation during the first year of therapy (28). A similar retrospective study of patients with neuroendocrine tumors included in a US National Comprehensive Cancer Network database revealed that 40% of carcinoid tumor patients and 23% of NET patients received dose escalations of octreotide, mainly due to inadequate symptom control or disease progression (29). It is possible that a subset of patients included in our study had become refractory to octreotide therapy, but were responsive to lanreotide therapy. The finding that only four patients (4.4%) had experienced a dose escalation while taking lanreotide supports this hypothesis.
Consistent with published literature, abdominal pain, flushing, and diarrhea were the most commonly reported signs or symptoms while patients were on treatment with long-acting octreotide alone or lanreotide (7,30,31). Of note, the proportions of patients with diarrhea, abdominal pain, and flushing tended to be less commonly recorded during lanreotide than during octreotide. Episodes of flushing were less commonly reported in patients who received successful injections in a study of octreotide delivery (24). However, patients experienced different durations of exposure to each treatment and follow-up periods were variable; therefore, any differences in AEs or symptoms reported should be interpreted with caution due to confounding factors.
Along with delaying progression and improving symptom control, sequencing patients from octreotide to lanreotide before initiating treatment with targeted agents or chemotherapy may result in cost savings. For example, other than octreotide and lanreotide, everolimus, a mammalian target of rapamycin (mTOR) inhibitor, is recommended for patients with progressive metastatic GEP-NET (6). A recent economic evaluation estimated the total annual per-patient cost (2016 US dollars) for treating patients with gastrointestinal NET with octreotide (up to 30 mg every 4 weeks) to be $54,671; with lanreotide (up to 120 mg every 4 weeks) to be $63,951; and with everolimus (up to 10 mg daily) to be $118,217 (32). The feasibility of sequencing patients with lanreotide after octreotide (including patients who had progressive disease on octreotide) may, therefore, result in cost savings. Pokuri et al. showed that transitioning patients to lanreotide versus higher doses of octreotide (40 or 60 mg) saved $10,400 per patient per year in a single institution (33).
Limitations
Patients included in the study were selected from a convenience sample of six major cancer centers. Therefore, study findings may not be generalizable to the overall population of patients with locally advanced or metastatic GEP-NET. However, the average age of patients in our study was similar to the average age reported in previous studies conducted among patients with advanced NET (7,10).
All data, including reported symptoms and other AEs, were limited to those available in patients’ medical records and were captured retrospectively. Our medical record abstraction may not have captured all patients with functional disease due to the fact that biochemical testing may not have been conducted for all patients. Additionally, health care services received outside of each site’s care setting were not included. However, we do not expect underreporting to have affected either the octreotide or lanreotide treatment phases disproportionately. Data were entered by abstractors and therefore may have been subject to entry errors and resulting inaccuracies in reporting. Data checks were in place to ensure internal consistency of the data, but responses were not validated against the patients’ medical records by an independent reviewer. Time to progression or death were calculated from the start of lanreotide treatment, and therefore due to the 90-day treatment minimum, patients who either died or discontinued lanreotide treatment within 90 days of initiation were excluded, introducing a potential for immortal person-time bias.
Because our study was conducted within the context of routine medical practice and no formal criteria for evaluation of disease progression was followed, the data reflect physician judgments; such evaluations may have been subject to individual differences among physicians or even by the same physician at different time points. Abstraction of data from medical records may cause some upward bias in PFS and contribute to a greater variation in the PFS distribution than would typically be seen in a clinical trial. Finally, the type and frequency of testing to assess tumor status in a real-world practice may differ (and is typically more variable) from that required in a clinical trial protocol. Taking these limitations into account, caution should be exercised when evaluating the PFS estimates from this study, as our patient population was different from the patient populations included in clinical trials.
Conclusions
Lanreotide appears to be safe and effective as a second-line treatment in a subset of patients who received octreotide as a first-line treatment, particularly among patients with more indolent disease. Among the 22 patients who had progressive disease at the time of treatment transition to lanreotide and a subsequent radiologic assessment, nearly half (45.5%) experienced stabilization of their disease at last radiologic assessment. The unanticipated patient responses observed in this medical record review warrant further exploration through prospective and/or larger retrospective studies.
Acknowledgments
This work was supported by IPSEN through a research contract between IPSEN and RTI Health Solutions. IPSEN participated in study design, research, data collection, analysis and interpretation of data, writing, reviewing, and approving the publication. The authors acknowledge the contributions of Michael DeSordi and Catherine Lubeck during the conduct of this study. Karyn Hede and Kate Lothman of RTI Health Solutions provided medical writing services, which were funded by IPSEN.
Footnote
Conflicts of Interest: At the time the study was conducted, R Parikh, SK Kurosky, JA Kaye, and S Nagar were full-time employees of RTI Health Solutions, which received research funding from IPSEN Biopharmaceuticals, Inc. (IPSEN) to conduct the study. D Ray, T Beveridge, and B Mirakhur were employees of IPSEN at the time of the study. R Ramirez has consulted for Novartis, and Advanced Accelerator Applications, and is a member of the speakers’ bureau for IPSEN, Merck, Guardant Health, Genentech, and Astra-Zeneca. K Thomas has no conflicts of interest to declare. TR Halfdanarson is an advisory board member for Lexicon, and Advanced Accelerator Applications and has received research support from IPSEN, Agios, ArQule, and Thermo Fisher Scientific. H Soares has consulted for IPSEN, Novartis, Bayer, and Lexicon.
Ethical Statement: The study was reviewed and approved by the institutional review boards (IRBs) of participating sites, including RTI International’s IRB, per individual site policies.
References
- Dasari A, Shen C, Halperin D, et al. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol 2017;3:1335-42. [Crossref] [PubMed]
- Yao JC, Hassan M, Phan A, et al. One hundred years after "carcinoid": epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008;26:3063-72. [Crossref] [PubMed]
- Oberg KE. The management of neuroendocrine tumours: current and future medical therapy options. Clin Oncol (R Coll Radiol) 2012;24:282-93. [Crossref] [PubMed]
- Strosberg JR, Nasir A, Hodul P, et al. Biology and treatment of metastatic gastrointestinal neuroendocrine tumors. Gastrointest Cancer Res 2008;2:113-25. [PubMed]
- Giustina A, Bonadonna S, Bugari G, et al. High-dose intramuscular octreotide in patients with acromegaly inadequately controlled on conventional somatostatin analogue therapy: a randomised controlled trial. Eur J Endocrinol 2009;161:331-8. [Crossref] [PubMed]
- NCCN. NCCN clinical practice guidelines in oncology (NCCN guidelines). Neuroendocrine tumors version 3: National Comprehensive Cancer Network 2017.
- Strosberg J, Casciano R, Stern L, et al. United States-based practice patterns and resource utilization in advanced neuroendocrine tumor treatment. World J Gastroenterol 2013;19:2348-54. [Crossref] [PubMed]
- Wolin EM. The expanding role of somatostatin analogs in the management of neuroendocrine tumors. Gastrointest Cancer Res 2012;5:161-8. [PubMed]
- Rinke A, Muller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol 2009;27:4656-63. [Crossref] [PubMed]
- Caplin ME, Pavel M, Cwikla JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med 2014;371:224-33. [Crossref] [PubMed]
- Wolin EM, Pavel M, Cwikla JB, et al. Final progression-free survival (PFS) analyses for lanreotide autogel/depot 120 mg in metastatic enteropancreatic neuroendocrine tumors (NETs): The CLARINET extension study. J Clin Oncol 2017;35:4089. [Crossref]
- Vinik AI, Wolin EM, Liyanage N, et al. Evaluation of lanreotide depot/autogel efficacy and safety as a carcinoid syndrome treatment (elect): A randomized, double-blind, placebo-controlled trial. Endocr Pract 2016;22:1068-80. [Crossref] [PubMed]
- Fisher GA Jr, Wolin EM, Liyanage N, et al. Lanreotide therapy in carcinoid syndrome: Prospective analysis of patient-reported symptoms in patients responsive to prior octreotide therapy and patients naive to somatostatin analogue therapy in the elect phase 3 study. Endocr Pract 2018;24:243-55. [Crossref] [PubMed]
- Octreotide acetate for injectable suspension (Sandostatin® LAR) Depot (prescribing information). East Hanover (NJ) 2016.
- Lanreotide (Somatuline®) Depot (prescribing information). Basking Ridge (NJ) 2017.
- Adelman DT, Burgess A, Davies PR. Evaluation of long-acting somatostatin analog injection devices by nurses: a quantitative study. Med Devices (Auckl) 2012;5:103-9. [Crossref] [PubMed]
- Forthofer RN, Lee ES, Hernandez M. Biostatistics: a guide to design, analysis and discovery. 2nd ed. Academic Press; 2007.
- Rosner B. Fundamentals of biostatistics. 7th ed. Cengage Learning; 2010.
- Klein JP, Moeschberger ML. Survival analysis: techniques for censored and truncated data. New York: Springer-Verlag; 2003.
- Fong MK, Pokuri VK, Causebrook A, et al. Safety and tolerability of sequencing somatostatin analogs (octreotide to lanreotide depot) in the treatment of neuroendocrine tumors: an institutional case series. Int J Clin Exp Med 2016;9:19771-7.
- Saif MW, Fu J, Smith M, et al. Lanreotide autogel/depot (LAN) post-octreotide long-acting release (OCT) for safe and tolerable treatment of gastroenteropancreatic neuroendocrine tumors (GEP-NETs). North American Neuroendocrine Tumor Society Meeting; Sept 30-Oct 1; Jackson, WY 2016.
- Astruc B, Marbach P, Bouterfa H, et al. Long-acting octreotide and prolonged-release lanreotide formulations have different pharmacokinetic profiles. J Clin Pharmacol 2005;45:836-44. [Crossref] [PubMed]
- Riechelmann RP, Pereira AA, Rego JF, et al. Refractory carcinoid syndrome: a review of treatment options. Ther Adv Med Oncol 2017;9:127-37. [Crossref] [PubMed]
- Boyd AE, DeFord LL, Mares JE, et al. Improving the success rate of gluteal intramuscular injections. Pancreas 2013;42:878-82. [Crossref] [PubMed]
- Manon A, Wolin EM, Chassaing C, et al. Pharmacokinetic differences between subcutaneous and intramuscular administration of lanreotide: Results from a phase I study. J Clin Oncol 2015;33:e15186-e.
- Marty R, Roze S, Kurth H. Decision-tree model for health economic comparison of two long-acting somatostatin receptor ligand devices in France, Germany, and the UK. Med Devices (Auckl) 2012;5:39-44. [PubMed]
- Broder MS, Beenhouwer D, Strosberg JR, et al. Gastrointestinal neuroendocrine tumors treated with high dose octreotide-LAR: a systematic literature review. World J Gastroenterol 2015;21:1945-55. [Crossref] [PubMed]
- Xu Y, Shih Y-CT, Leary C, et al. Dosing patterns of octreotide LAR among elderly patients with neuroendocrine tumors: Analysis of the SEER-Medicare database. J Clin Oncol 2012;30:e14550.
- Strosberg JR, Bobiak S, Zornosa CC, et al. Dosing patterns for octreotide LAR in neuroendocrine tumor (NET) patients: NCCN NET outcomes database. J Clin Oncol 2013;31:4142.
- Alexandraki KI, Karapanagioti A, Karoumpalis I, et al. Advances and current concepts in the medical management of gastroenteropancreatic neuroendocrine neoplasms. Biomed Res Int 2017;2017:9856140. [Crossref] [PubMed]
- Boutzios G, Kaltsas G. Clinical syndromes related to gastrointestinal neuroendocrine neoplasms. Front Horm Res 2015;44:40-57. [Crossref] [PubMed]
- Rose DB, Nellesen D, Neary MP, et al. Budget impact of everolimus for the treatment of progressive, well-differentiated, non-functional neuroendocrine tumors of gastrointestinal or lung origin that are advanced or metastatic. J Med Econ 2017;20:395-404. [Crossref] [PubMed]
- Pokuri VK, Fong MK, Iyer R. Octreotide and Lanreotide in Gastroenteropancreatic Neuroendocrine Tumors. Curr Oncol Rep 2016;18:7. [Crossref] [PubMed]