Do clinicopathologic features of rectal and colon cancer guide us towards distinct malignancies?
Introduction
Rectal and colonic cancers account for about 10% of all malignancies (1). Traditionally, colorectal cancer was known to be a disease of developed and high-income countries (2). Its geographic variation suggests the effect of western lifestyle in the incidence of this cancer. Like other parts of Asia, Middle East was a low risk region regarding colonic and rectal cancers but recent studies show an increasing trend in the incidence rate for this part of the world (2-4).
As a result of their similarities, rectal and colon cancer are generally considered as one organ malignancy; colorectal carcinoma. However, the different embryological origin, anatomical structure and physiologic function of colon and rectum guided some researchers to examine probable molecular, clinical and pathologic differences of rectal and colonic cancers (5,6). Moreover, some studies imply considerable variation in response to the same treatment for rectal cancer versus colonic cancer in an equal stage (7). For example, Kornmann and colleagues claimed that Folonic Acid improves the overall survival in patients with colon cancer but not in ones with rectal cancer (7). These differences show the necessity to consider colorectal cancers in two groups namely colon and rectal cancer.
Unlike developed countries where studies on all aspects of colorectal cancers are widely numerous, Iran as a Middle Eastern country show very few studies especially ones comparing the differences between colon and rectal cancer. Therefore, we conducted this study to compare clinical and pathologic findings of colon and rectal carcinoma in Shiraz, south of Iran. In this study, firstly we report demographic, clinical and pathologic characteristics of patients with rectum and colon cancer and secondly compare these findings in order to investigate probable differences.
Methods
In this cross-sectional study we utilized data of 452 colonic or rectal cancer patients gathered by the disease registry of Colorectal Research Center, Shiraz University of Medical Sciences. This database was gathered prospectively from patients with colorectal cancer who referred to Faghihi Hospital, the main colorectal surgery center in south of Iran.
According to the International Classification of Diseases, all patients were divided into two groups: the rectal cancer group and the colonic cancer group. The rectal cancer group included carcinomas of the recto sigmoid, rectum and anal canal. The colonic cancer group included carcinomas of sigmoid and, descending colon, splenic flexure, transverse colon, hepatic flexure, ascending colon and cecum.
Both groups were compared regarding demographic, clinical and pathologic information of patients which included age, gender, BMI, family history, clinical presentation, lab findings and pathologic reports. Type of disease was classified as colon or rectal cancer, tumor stage was categorized using Tumor-Node-Metastasis (TNM) classification, and type of lesion was categorized as ulcerative, fungative, polypoid, or infiltrative by a colorectal surgeon. Patients with preoperative therapy and synchronous colon and rectum malignancy were excluded from the study. All statistical calculations were performed using Stata version 12. Differences in clinical and pathological characters between colonic and rectal cancer were performed by Pearson’s Chi-squared for categorical variables and t-test for interval ones. Differences were considered significant when P value (two tailed) was less than 0.05.
This study was evaluated and approved by the ethics committee of vice chancellery for research affairs of Shiraz University of Medical Sciences (Code: IR.SUMS.REC.1395.S1103).
Results
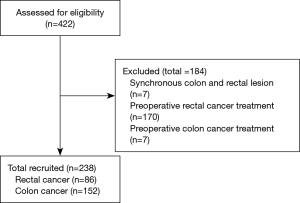
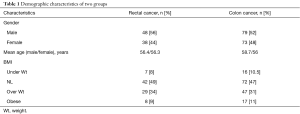
We assessed 422 colon and rectal cancer cases of registry of Colorectal Research Center, Shiraz University of Medical Sciences out of which 238 met the inclusion criteria. Seven patients (1.66%) were omitted due to synchronously colon and rectal lesions and 177 other cases (42%) excluded due to preoperative chemotherapy or radiotherapy (Figure 1). Demographic characteristics of the remaining 238 patients with colon or rectal cancers are shown in Table 1. Patients were divided into rectal cancer group including 86 patients with mean age 56.4 and colon cancer group with 152 patients with mean of age 57.4. There were no statistical differences between the two groups regarding age and gender and BMI.
Full table
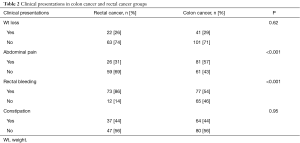
Regarding clinical presentation, the proportion of rectal bleeding was significantly higher in colon cancer group (P<0.001). Moreover, abdominal pain was significantly more frequent in colon cancer group (P<0.001). Presentations such as weight loss and constipation showed no statistically significant difference (Table 2).
Full table
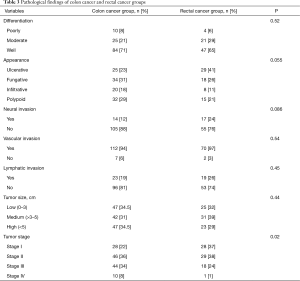
In terms of surgical and pathological findings tumor size, tumor gross type (appearance), tumor differentiation (grade), vascular invasion, neural invasion, lymphatic invasion and tumor stage are compared and reported in Table 3. As it is seen, only in the tumor stage there was a significant statistical difference between the two groups.
Full table
Discussion
Our study showed similarities between rectal and colon cancer regarding characteristics such as age, gender and BMI. For clinical findings, frequency of patients’ complaints about weight loss and constipation were the same in patients with rectal versus those with colon cancer. However, other complaints about abdominal pain and rectal bleeding appeared in different proportions comparing the two cancer groups; with the former more in colon cancer group and the latter more in rectal cancer group. Pathologic finding was almost the same in both groups except for the stage of tumors which showed a statistically significant difference between these two.
There are reports showing the proportion of young patients with colon and rectal cancer in the Middle East more than western countries (8-11). A study conducted by Malekzadeh et al. in Iran reported that up to 20% of patients with colorectal cancer were under the age 40 compared to only 2% to 8% in USA (12). This proportion is even larger in Yemen and Egypt (13,14). In our study only 13% of all patients were under 40 years old. Considering the two groups of colon cancer and rectal cancer, this proportion was 10% in patients with rectal cancer and 16% in colon cancer cases. For the rectal cancer group, the mentioned proportion is not much different from the proportion in Western countries but for the colon cancer group, it is at least twice of that of Western countries, even though it is, less than other reports from Iran.
Anatomic and other characteristics of colon versus rectum make some symptoms more common in each. In patients with colon cancer, abdominal pain is more common than in those with rectal cancer and as a result of total or partial obstruction. Overall, pain in patients with rectal cancer is rare except in case of involvement of neural plexus of anal canal or the surroundings (15). In our study as, abdominal pain is seen more in colon cancer patients compared to rectal cancer ones as well. Rectorrhagia (rectal bleeding) is the most common symptom in the rectal cancer group and this may be explained this way; the more a lesion is distal the redder and more noticed the bleeding is. In our study over 80% of patients with rectal cancer complained from rectal bleeding.
Regarding pathologic features, staging and grading of tumor are of more importance. In our study, considering tumor differentiation, no significant difference was detected in colon versus rectal cancer group. Almost two-thirds of all patients of both groups had well differentiated tumors. This proportion was about one-fourth of moderately differentiated tumors. Our findings show a considerable variation with in some reports from of developed and developing countries. To illustrate, in a review article Fleming et al. from David Geffen School of Medicine at University of California claimed that about 70% of colorectal tumors are moderately differentiated (16). Another study from Medina, Saudi Arabia reported more than 90% of moderately differentiated tumors in patients with colorectal cancer (17).
On the other hand, regarding stage, there was a statistically significant difference between colon cancer group and rectal cancer group. The proportion of patients with rectal cancer of stage I were just less than twice of patients with colon cancer at the same stage. This is probably because of sooner rectal bleeding in patients with rectal cancer which results in sooner complaint thus diagnosis at earlier stages. Moreover, although just less than one tenth of patients with colon cancer were in stage IV, the number was 6 times of the count of patients with rectal cancer. This seems logical due to anatomic characteristics of colon and rectum which makes diagnosis of rectal cancers sooner than colon cancers. A small number of patients with stage IV should be mentioned as a limitation for our study. Overall, the proportion of patients with stage II in both groups is in concordance with other reports in the region.
Conclusions
To sum up, we did not find enough evidences to conclude that rectal cancer and colon cancer should be investigated as two distinct malignancies but findings showed significant differences such as stage at diagnosis encouraged us in order to conduct other appropriate studies for better evaluation of this issue.
Acknowledgements
The authors would like to express their gratitude to this Mrs. Mahbobeh Pourahmad for data collection of this study.
Funding: This study was extracted from the dissertation of Dr. Salar Rahimikazerooni supported by Shiraz University of Medical Sciences (grant number: 11315).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was evaluated and approved by the ethics committee of vice chancellery for research affairs of Shiraz University of Medical Sciences (Code: IR.SUMS.REC.1395.S1103) and written informed consent was obtained from all patients.
References
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Center MM, Jemal A, Ward E. International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomarkers Prev 2009;18:1688-94. [Crossref] [PubMed]
- Rezaianzadeh A, Safarpour AR, Marzban M, et al. A Systematic Review Over the Incidence of Colorectal Cancer in Iran. Ann Colorectal Res 2015;3:e25724. [Crossref]
- Haggar FA, Boushey RP. Colorectal cancer epidemiology: incidence, mortality, survival, and risk factors. Clin Colon Rectal Surg 2009;22:191-7. [Crossref] [PubMed]
- Li M, Li JY, Zhao AL, et al. Colorectal cancer or colon and rectal cancer? Clinicopathological comparison between colonic and rectal carcinomas. Oncology 2007;73:52-7. [Crossref] [PubMed]
- Tamas K, Walenkamp AM, de Vries EG, et al. Rectal and colon cancer: Not just a different anatomic site. Cancer Treat Rev 2015;41:671-9. [Crossref] [PubMed]
- Kornmann M, Staib L, Wiegel T, et al. Long-term results of 2 adjuvant trials reveal differences in chemosensitivity and the pattern of metastases between colon cancer and rectal cancer. Clin Colorectal Cancer 2013;12:54-61. [Crossref] [PubMed]
- Aghili M, Izadi S, Madani H, et al. Clinical and pathological evaluation of patients with early and late recurrence of colorectal cancer. Asia Pac J Clin Oncol 2010;6:35-41. [Crossref] [PubMed]
- Ahmadi A, Mosavi-Jarrahi A, Pourhoseingholi MA. Mortality determinants in colorectal cancer patients at different grades: a prospective, cohort study in Iran. Asian Pac J Cancer Prev 2015;16:1069-72. [Crossref] [PubMed]
- Moradi A, Khayamzadeh M, Guya M, et al. Survival of colorectal cancer in Iran. Asian Pac J Cancer Prev 2009;10:583-6. [PubMed]
- Beckmann K, Moore J, Wattchow D, et al. Short-term outcomes after surgical resection for colorectal cancer in South Australia. J Eval Clin Pract 2017;23:316-24. [Crossref] [PubMed]
- Malekzadeh R, Bishehsari F, Mahdavinia M, et al. Epidemiology and molecular genetics of colorectal cancer in iran: a review. Arch Iran Med 2009;12:161-9. [PubMed]
- Moore MA, Eser S, Igisinov N, et al. Cancer epidemiology and control in North-Western and Central Asia - past, present and future. Asian Pac J Cancer Prev 2010;11 Suppl 2:17-32. [PubMed]
- Salim EI, Moore MA, Bener A, et al. Cancer epidemiology in South-West Asia - past, present and future. Asian Pac J Cancer Prev 2010;11 Suppl 2:33-48. [PubMed]
- Corman M. Corman’s Colon and Rectal Surgery. In: Corman ML, Nicholls RJ, Fazio VW, et al. editors. Colorectal Disease. Philadelphia: Wolters Kluwer, Lippincott Williams and Wilkins, 2013.
- Fleming M, Ravula S, Tatishchev SF, et al. Colorectal carcinoma: Pathologic aspects. J Gastrointest Oncol 2012;3:153-73. [PubMed]
- Albasri A, Yosef H, Hussainy AS, et al. Histopathological features of colorectal cancer in Al-Madinah region of Saudi Arabia: 8 years experience. Asian Pac J Cancer Prev 2014;15:3133-7. [Crossref] [PubMed]