Pancreatic head carcinoma and right hepatic artery: embolization management—A case report
Introduction
An aberrant hepatic artery is a common anatomical variant (1). The right hepatic artery (RHA) arising from the superior mesenteric artery (SMA), is frequently encountered and can be problematic in pancreatic ductal adenocarcinoma (PDAC) (2). Pancreaticoduodenectomy (PD) is the intervention of choice in periampullary carcinoma. The preservation of the RHA is necessary to avoid ischemic complications but can impact margins resection. Another option consisting in arterial resection followed by reconstruction is possible but is known to increase complication rates. We reported a case of preoperative embolization of the RHA in a patient with pancreatic head tumor. That embolization allowed the development of collaterals from the left branch of the hepatic artery to the right liver lobe.
Case report
A 53-year-old man, with history of ischemic heart disease, arterial hypertension and alcohol intoxication presented altered general status with weight loss and jaundice since one month. The blood analysis showed cholestasis (total bilirubin =125 mg/L) and cytolysis [aspartate aminotransferase (ASAT) =258 UI/L, alanine aminotransferase (ALAT) =625 UI/L]. The serum carbohydrate antigen level (CA19-9) was slightly increased at 50.9 U/mL while carcinoembryonic antigen (CEA) level was normal at 2.6 µg/L.
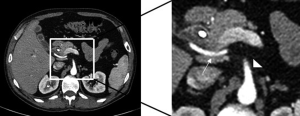
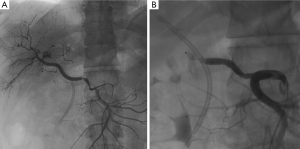
The abdominal computed tomography (CT) revealed a 16 mm × 18 mm mass of the pancreas head coming in contact with the underside of the portal vein but with no abutment or invasion of the superior mesenteric vessels. There was a 12 mm retro-portal lymph node, with no distant metastasis. The left branch of the hepatic artery had a regular origin from the middle hepatic artery, whereas there was a RHA arising from the SMA that was exclusive for the right liver lobe (i.e., replaced RHA Michels 3) (3). There was a close contact between the tumor and the RHA (Figure 1). The complementary investigations were also negative. Embolization of this artery was carried out by percutaneous puncture of the right femoral artery. After catheterization of the RHA, we set up a plug of 7 mm of diameter obtaining immediately the complete obstruction of the RHA (Figure 2). A concomitant biliary drainage had been previously performed to reduce jaundice and avoid septic complications.
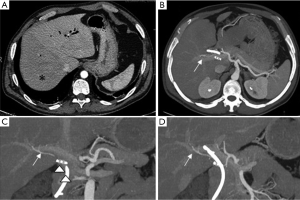
A CT was done on the first postembolization day and after three weeks. The first CT revealed total obstruction of the RHA with subsequent right hepatic ischemia. The second CT demonstrated the disappearance of the right hepatic ischemia and the development of a collateral system arising from the left branch and revascularizing the right liver lobe (Figure 3).
The patient was operated 22 days after the embolization. After an abdominal exploration, PD was performed. The liver parenchyma did not show any signs of ischemia. There was a macroscopic invasion of both the portal vein and the RHA requiring a monobloc resection. After segmental resection, the portal vein was reconstructed through an end-to-end anastomosis. The complete retro-portal lamina excision was particularly difficult due to inflammation caused by embolization. The histopathological examination of the specimen revealed a pancreatic duct adenocarcinoma with 3 metastatic lymph nodes out of 15 resected. The RHA was not microscopically invaded but located at 0.5 mm from the tumor edge. All margins, especially the vascular one, were negative.
Discussion
The hepatic arterial vasculature is extremely variable (1). In most cases, the hepatic artery arises from the celiac axis, dividing into two branches destinated to both hepatic lobes (3,4). However, anatomical variants are observed in up to 30% to 46% of patients (1,3). A replaced RHA is one of the most common anatomical variant. It takes origin from the SMA and access to the hepatic pedicle by following the retroportal lamina behind the head of pancreas. Michels reported a classification of anatomic variation of hepatic artery supply in 1966 (3). In 200 specimens, 26% of aberrant RHA were encountered, of which 18% were replaced and 8% were accessory. The exact knowledge of this variant by surgeons is required to prevent a vascular injury during PD. In fact, the vascularization of the common bile duct is provided by both the gastroduodenal artery (GDA) and the right branch of the hepatic artery or the RHA if it’s replaced. In PD, the GDA is ligated and injury or ligation of the RHA can favor ischemic complications and secondary biliary fistula or stenosis (5,6). This arterial interruption can also promote ischemic cholangitis and hepatic abscess in some cases (7). Turrini et al. reported RHA identification by radiologists in preoperative CT in only 30% of patients, while it was detected by surgeons in 50% of cases (4).
Several series have reported the impact of the RHA on PDAC management and outcome. Eshuis et al. described a similar surgical morbidity rate in patients with RHA compared with patients with no arterial variation (8). The presence of RHA in patients with PDAC did not appear to affect resectability in most series (4,9,10). Turrini et al. reported no difference in rates of positive resection margins despite the preservation of a replaced or accessory RHA during PD (4). However, these data were published before standardization of histopathological analysis and could have underestimated the rates of R1 vascular margin (11). When this artery is invaded or in contact with the tumor, its resection is necessary to obtain free resection margins, especially for the vascular margin. This latter is reported as a major predictor of long-term survival following PD for PDAC (11). Some authors reported that RHA ligation with reconstruction is safe and feasible (4,12). The preoperative embolization of RHA is an interesting alternative as it prepares the patient to the intervention by allowing the development of the collaterals from the left branch. In our patient, hepatic ischemia was observed on CT performed 1day after embolization demonstrating the real existence of ischemia and its potential consequences for the patient after PD if the RHA would have been injured or sacrificed without reconstruction. A follow-up CT performed three weeks after embolization demonstrated the development of a collateral system arising from the left branch to the right liver lobe with no residual ischemia. The tumor size remained stable. No adverse effect was reported.
The patient underwent PD three weeks after embolization. The excision of retroportal lamina was especially challenging due to important inflammation caused by the plug in the proximal part of the RHA. We now advise that RHA embolization should be performed at the level of the hepatic pedicle, away of the RHA origin to prevent this inflammation. On the other hand, very distal embolization must be avoided because it may hinder the collaterals development. The histological examination confirmed an R0 resection. To our knowledge, there are only few cases of RHA embolization before PD reported in the literature. Cloyd et al. reported the first description of embolization of RHA in two patients with periampullary tumors (13). Some authors described preoperative embolization of a replaced common hepatic artery arising from the SMA in patients with pancreatic cancer without any serious complications (14,15).
In conclusion, the knowledge of hepatic artery variation is essential in pancreatic surgery. Preoperative embolization of RHA that is exclusive for the vascularization of the right liver lobe can be useful.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Hiatt JR, Gabbay J, Busuttil RW. Surgical anatomy of the hepatic arteries in 1000 cases. Ann Surg 1994;220:50-2. [PubMed]
- Yang SH, Yin YH, Jang JY, et al. Assessment of hepatic arterial anatomy in keeping with preservation of the vasculature while performing pancreatoduodenectomy: an opinion. World J Surg 2007;31:2384-91. [PubMed]
- Michels NA. Newer anatomy of the liver and its variant blood supply and collateral circulation. Am J Surg 1966;112:337-47. [PubMed]
- Turrini O, Wiebke EA, Delpero JR, et al. Preservation of replaced or accessory right hepatic artery during pancreaticoduodenectomy for adenocarcinoma: impact on margin status and survival. J Gastrointest Surg 2010;14:1813-9. [PubMed]
- Traverso LW, Freeny PC. Pancreaticoduodenectomy. The importance of preserving hepatic blood flow to prevent biliary fistula. Am Surg 1989;55:421-6. [PubMed]
- Northover JM, Terblanche J. A new look at the arterial supply of the bile duct in man and its surgical implications. Br J Surg 1979;66:379-84. [PubMed]
- Kayaalp C, Nessar G, Kaman S, et al. Right liver necrosis: complication of laparoscopic cholecystectomy. Hepatogastroenterology 2001;48:1727-9. [PubMed]
- Eshuis WJ, Olde Loohuis KM, Busch OR, et al. Influence of aberrant right hepatic artery on perioperative course and longterm survival after pancreatoduodenectomy. HPB (Oxford) 2011;13:161-7. [PubMed]
- Lee JM, Lee YJ, Kim CW, et al. Clinical implications of an aberrant right hepatic artery in patients undergoing pancreaticoduodenectomy. World J Surg 2009;33:1727-32. [PubMed]
- Jah A, Jamieson N, Huguet E, et al. The implications of the presence of an aberrant right hepatic artery in patients undergoing a pancreaticoduodenectomy. Surg Today 2009;39:669-74. [PubMed]
- Delpero JR, Bachellier P, Regenet N, et al. Pancreaticoduodenectomy for pancreatic ductal adenocarcinoma: a French multicentre prospective evaluation of resection margins in 150 evaluable specimens. HPB (Oxford) 2014;16:20-33. [PubMed]
- Sarmiento JM, Panneton JM, Nagorney DM. Reconstruction of the hepatic artery using the gastroduodenal artery. Am J Surg 2003;185:386-7. [PubMed]
- Cloyd JM, Chandra V, Louie JD, et al. Preoperative embolization of replaced right hepatic artery prior to pancreaticoduodenectomy. J Surg Oncol 2012;106:509-12. [PubMed]
- Miyamoto N, Kodama Y, Endo H, et al. Embolization of the replaced common hepatic artery before surgery for pancreatic head cancer: report of a case. Surg Today 2004;34:619-22. [PubMed]
- Kondo S, Katoh H, Shimizu T, et al. Preoperative embolization of the common hepatic artery in preparation for radical pancreatectomy for pancreas body cancer. Hepatogastroenterology 2000;47:1447-9. [PubMed]


