
Direct oral anticoagulants in gastrointestinal malignancies: is the convenience worth the risk?
Venous thromboembolic disease (VTE) is a common cause of morbidity and mortality in patients with cancer. The landmark CLOT trial demonstrated low-molecular-weight heparin’s (LMWH) superiority to vitamin K antagonists for treatment of established VTE in cancer patients (1). LMWH has therefore been endorsed by major guidelines for cancer-associated thrombosis (CAT) for over a decade. However, several aspects of LMWH render it non-ideal for this indication, including its parenteral administration, renal clearance, relatively high cost, and an approximately 8% breakthrough thrombosis rate (1).
Over the last decade, several direct oral anticoagulants (DOACs) have been approved by the U.S. Food and Drug Administration (FDA) for treatment of VTE, including dabigatran, apixaban, rivaroxaban, and edoxaban. Patients with cancer, however, were heavily underrepresented in the initial randomized controlled trials (RCTs), leaving the safety and efficacy of DOACs for the treatment of CAT uncertain. Several recent RCTs specifically enrolling cancer patients, however, have attempted to address this question. The Hokusai-Cancer, SELECT-D, and ADAM VTE trials compared edoxaban, rivaroxaban and apixaban, respectively, to dalteparin for the treatment of CAT. While the results of these large, phase 3 trials seem to demonstrate DOACs are noninferior to LMWH for the prevention of recurrent VTE, a major point of ongoing analysis is the elevated incidence of gastrointestinal (GI) bleeding, particularly in patients with GI malignancies. Herein, we review the data on bleeding specific to patients with CAT treated with DOACs, focusing on GI malignancies.
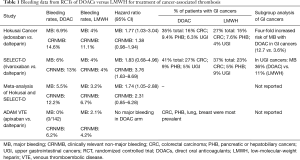
The Hokusai-Cancer trial found an almost two-fold increased risk of major bleeding (MB) with edoxaban compared to LMWH in the total study population (6.9% vs. 4.0%, HR 1.77, 95% CI: 1.03–3.04) for the treatment of CAT (2). Approximately one-third of subjects in each study arm had GI cancers. Subgroup analysis specific to GI cancer patients puts the increased risk of MB with edoxaban into even starker contrast, with a nearly 4-fold risk of MB compared with LMWH (12.7% vs. 3.6%). Analysis of patients with non-GI cancers found MB rates that were similar in both treatment arms. Of additional interest in Hokusai-Cancer is the equal distribution of upper and lower GI bleeds seen even among subjects with colorectal cancer; while overall numbers were small, this finding is inconsistent with the supposition that GI bleeding would originate from the primary tumor.
In the SELECT-D trial comparing rivaroxaban to LMWH for CAT, the rivaroxaban arm showed a non-statistically significant increase in the rate of MB (6% vs. 4%, HR 1.83; 95% CI: 0.68–4.96), while clinically relevant non-MB (CRNMB) was almost four-fold higher (3), and mostly of upper GI source. A subgroup analysis of patients with GI malignancies again revealed a substantially higher risk of MB with rivaroxaban compared to LMWH (36% vs. 11%); though overall numbers were small and bleeding events were mostly low grade, this increased GI bleeding signal prompted exclusion of additional subjects with GI cancers based on the recommendation of an independent Data Safety Monitoring Committee.
A systematic review and meta-analysis of the Hokusai-cancer and SELECT-D trials suggested that the risk of MB in cancer patients was approximately doubled when using DOACs compared with LMWH (4). An additional RCT recently presented in abstract form, the ADAM VTE trial, compared the DOAC apixaban with LMWH for CAT. This trial corroborated the favorable efficacy of DOACs compared with LMWH for thrombosis prevention seen in previous trials, though bleeding events were notably far milder (5), with no patients in the apixaban arm experiencing MB despite including a reportedly (though not numerically defined) large proportion of subjects with GI malignancies. More detailed analysis of the ADAM VTE trial will need to be performed upon its final publication.
While prospective RCTs have been fairly consistent in their finding that DOACs may increase GI bleeding risk (refer to Table 1), several smaller, non-randomized studies have contradicted these results. A prospective cohort study of patients treated for CAT in the Mayo Clinic VTE registry showed only non-statistically significant trends towards increased bleeding with DOACs compared with LMWH (6). A second cohort study of patients at the Cleveland Clinic also demonstrated statistically similar MB and CRNMB rates in the DOAC and LMWH arms, though GI bleeding did represent the majority of cases (7).
Full table
In aggregate, these findings raise several important questions: why do some DOACs cause an increased risk of GI bleeding, and why do GI malignancies, specifically upper GI cancers, have a higher propensity to bleed? Anatomic considerations, as well as DOAC-specific pharmacokinetics, may provide some potential explanations. The GI tract may be inherently more vulnerable to bleeding due to rich intra- and submucosal blood supply, high cell turnover, and regular mucosal disruption. DOAC specific effects may include direct topical anticoagulant or caustic actions on GI mucosal cells. For example, the tartaric acid component of dabigatran used to facilitate its absorption is known to cause dyspepsia, and could potentially compromise mucosal integrity. Intraluminal activation of the dabigatran pro-drug is also postulated to increase bleeding risk (8). The P-glycoprotein efflux pump that modulates intra-luminal DOAC concentration may also play a role, though this mechanism has not been firmly established (8). Additional mechanistic studies are clearly needed to clarify these points.
Available clinical trial data seem to support the efficacy of DOACs for treatment of CAT, though their safety is less consistent. The Scientific and Standardization Committee of the International Society of Thrombosis and Hemostasis has stated that DOACs may be considered for the treatment of CAT with several important caveats, including a warning against use in patients with intra-luminal GI cancers (9). If providers consider DOACs in these patients, it is important to discuss that despite their increased MB risk, fatal bleeding in major trials was rare (one patient each in Hokusai-Cancer and SELECT-D, none in ADAM VTE), bleeding events were mostly limited to grade 1–2, and similar frequencies and durations of withholding cancer-directed therapy were seen (3,10). The clinical impact of these considerations to providers and patients is ultimately subjective, and shared decision making remains crucial. Future trials in this area are warranted to determine safety of DOACs in GI cancer patients.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Lee AY, Levine MN, Baker RI, et al. Low-molecular-weight heparin versus a coumarin for the prevention of recurrent venous thromboembolism in patients with cancer. N Engl J Med 2003;349:146-53. [Crossref] [PubMed]
- Raskob GE, van Es N, Verhamme P, et al. Edoxaban for the Treatment of Cancer-Associated Venous Thromboembolism. N Engl J Med 2018;378:615-24. [Crossref] [PubMed]
- Young AM, Marshall A, Thirlwall J, et al. Comparison of an Oral Factor Xa Inhibitor With Low Molecular Weight Heparin in Patients With Cancer With Venous Thromboembolism: Results of a Randomized Trial (SELECT-D). J Clin Oncol 2018;36:2017-23. [Crossref] [PubMed]
- Li A, Garcia DA, Lyman GH, et al. Direct oral anticoagulant (DOAC) versus low-molecular-weight heparin (LMWH) for treatment of cancer associated thrombosis (CAT): A systematic review and meta-analysis. Thromb Res 2019;173:158-63. [Crossref] [PubMed]
- McBane RD, Wysokinski WE, Le-Rademacher J, et al. Apixaban, Dalteparin, in Active Cancer Associated Venous Thromboembolism, the ADAM VTE Trial. ASH Annual Meeting; San Diego, California; December 2, 2018. abstr 421.
- Houghton DE, Bott-Kitslaar DM, Vargas E, et al. Cancer-Associated Thrombosis and Bleeding Risk in Gastrointestinal Malignancies with Apixaban and Rivaroxaban Compared to Low Molecular Weight Heparin. ASH Annual Meeting; San Diego, California; December 2, 2018. abstr 362.
- Park DY, Poudel SK, Jia X, et al. Clinical Outcomes with Direct Oral Anticoagulants Compared to Low Molecular Weight Heparins in the Treatment of Cancer-Associated Venous Thromboembolism. ASH Annual Meeting; San Diego, California; December 1, 2018. abstr 1237.
- Vaduganathan M, Bhatt DL. Gastrointestinal Bleeding With Oral Anticoagulation: Understanding the Scope of the Problem. Clin Gastroenterol Hepatol 2017;15:691-3. [Crossref] [PubMed]
- Khorana AA, Noble S, Lee AYY, et al. Role of direct oral anticoagulants in the treatment of cancer-associated venous thromboembolism: guidance from the SSC of the ISTH. J Thromb Haemost 2018;16:1891-4. [Crossref] [PubMed]
- Kraaijpoel N, Di Nisio M, Mulder FI, et al. Clinical Impact of Bleeding in Cancer-Associated Venous Thromboembolism: Results from the Hokusai VTE Cancer Study. Thromb Haemost 2018;118:1439-49. [Crossref] [PubMed]


