
Adherence to surveillance guidelines following colonic polypectomy is abysmal
Introduction
Colorectal cancer (CRC) is the one of the most common cancers in the world with significant physical, financial, and psychological burdens to the patients, their families and societies as well (1). Screening for CRC has been proven to improve oncological outcomes and is strongly recommended in numerous countries worldwide (2-4). The removal of colonic adenomatous polyps via colonoscopy prevents the development of CRC.
In these individuals, due to their purported higher risks of developing new polyps and possibly CRC, several international guidelines have advocated surveillance colonoscopy. The interval of the subsequent colonoscopy is dependent on factors such as the patient’s inherent risks of developing colon cancer as well as the findings on colonoscopic evaluation and histological results of the polypectomy specimens (5-7).
Performing this procedure more frequently subjects patients to unnecessary risks of the invasive procedure and drive up the healthcare cost without much clinical benefit (8). Postponing the procedure could result in delayed diagnosis of the polyps and cancers.
Even though there may be existing, and regularly updated, guidelines, there is a lack of quantitative data which audits the compliance to them. There is also a lack of published data which evaluates the implications of non-compliance to the recommended guidelines. Our study aims to evaluate the adherence to existing polyp surveillance guidelines and evaluate the clinical implication of such non-compliance.
Methods
After institutional review board approval was obtained, a review of a prospectively-collected endoscopy database was performed for January to December 2008. This particular year was selected so that adequate long-term details of polyp recurrence and cancer development can be obtained from the individuals from surveillance endoscopic evaluation.
Patients who had at least one polypectomy performed during their colonoscopy were included in the study. Patients who had CRC diagnosed during the colonoscopy or had prior history of CRC were excluded from the study. Data such as demographic characteristics, findings of the colonoscopy and histopathological details were collected and analysed.
The dates of the surveillance colonoscopies were identified using the same endoscopic database and evaluated to be either appropriate, too early or too late based on the European Society of Gastrointestinal Endoscopy (ESGE) Guidelines. Outcomes of the surveillance colonoscopy were also captured.
Results
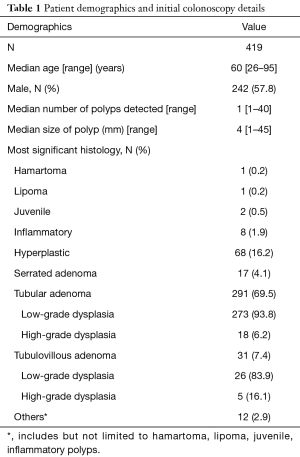
In 2008, 723 patients had polypectomies performed, out of this, 419 patients, with a median age of 60 (range, 26–95) years, were included in the study. The rest of the patients either had prior history of CRC or had cancer diagnosed during their 2008 colonoscopy.
The median number of polys detected and removed for each patient were 1 (range, 1–40), and 4 mm (range, 1–45 mm), respectively. Only the most clinically significant polyp for each individual was taken into account. The majority (n=291, 69.5%) of the polyps were tubular adenomas with low-grade dysplasia with only 80 individuals (19.1%) not having adenomatous polyps. Details of patient demographics and the initial colonoscopy can be found in Table 1.
Full table
Of the 419 patients, only 58 (13.8%) adhered to SAGES and ESGE polyp surveillance guidelines appropriately. Of those whose surveillance colonoscopy did not adhere to guidelines, more than half of them had their surveillance colonoscopy performed later (53.2%) with another 13.3% defaulting follow-up. Compliance details can be found in Table 2.

Full table
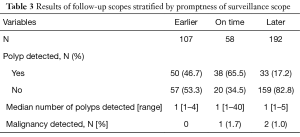
Two patients (1.0%) who had their surveillance colonoscopy later than recommended and another (1.7%) who had surveillance colonoscopy on time were found to have developed CRC.
In the group that was scoped later than recommended, the first patient was found to have three polyps, all 3 were tubular adenoma with low-grade dysplasia, the biggest being 4 mm, in the sigmoid colon. He was not offered a repeat colonoscopy till 6 years later when the patient experienced significant weight loss. A half-circumferential ascending colon tumour was found then. The second patient initially underwent a colonoscopy for haematochezia and was found to have radiation proctitis (on a background of treated prostate cancer) and a 2-cm sigmoid tubular adenoma with low-grade dysplasia. No repeated endoscopy was offered and he had a repeated scope 8 years later after surveillance PET-CT scan showed FDG-avidity in the distal sigmoid and rectum. The repeated scope revealed a half-circumferential proximal rectal cancer. Quality of bowel preparation for the initial colonoscopy for both patients were good and the patients tolerated the scope well.
In the group that had repeated colonoscopy on schedule, one patient had five polyps (ascending colon 5 mm, descending colon 2 mm × 7 mm, sigmoid 4 cm, rectal 3 mm). The largest polyp measuring 4 cm was a pedunculated tubular adenoma with high-grade dysplasia. This patient had a repeated colonoscopy 28 months later which found a circumferential transverse colon tumour. Quality of bowel preparation for the initial colonoscopy was good and the patient tolerated the scope well.
None of those who had their surveillance colonoscopy earlier than recommended were found to have developed CRC at point of surveillance. Detailed results of follow-up colonoscopy can be found in Table 3.
Full table
Discussion
The American Cancer Society, US Multi-Society Task Force against CRC and ESGE have all established and globally accepted evidence-based guidelines for polyp surveillance (5,6). These guidelines have been widely adopted all over the world. However, our data shows that there is poor compliance to these guidelines with only 13.6% of the patients actually receiving surveillance scope post-polypectomy at the appropriate time interval.
Poor compliance to these guidelines has been demonstrated elsewhere, however, extensive data is not available (9-12). There are likely a multitude of factors for this observation and it could be physician-, patient- and resource-related (13).
Some physicians may want to repeat the scope earlier in hope that new polyps are removed earlier to mitigate the chance of them developing into colon cancer, others may not be aware of the guidelines and the true importance of surveillance colonoscopy and have not guided the patients appropriately. These physicians may range from general practitioners to gastroenterologists and general surgeons. The “explosion” of information and extensive guidelines for almost all diseases, both benign and malignant, would definitely make it confusing for general physicians to remember the finer details for each condition.
Patients may also adopt two mentalities. First and foremost, the ordeals of the bowel preparation and the cost of the procedure could have deterred them from being compliant to the recommendation. In addition, these individuals are asymptomatic and the inconvenience of arranging the colonoscopy only made matters worse. On the other hand, some patients may get too worried about their risks of developing new polyps or cancers and hence were keener to undergo more frequent colonoscopy.
From a resource perspective, it is difficult to follow up these asymptomatic individuals over a long period of time. In many institutions in Singapore, these individuals are often discharged following their index colonoscopy and advised to return for their colonoscopy few years later. They are often not followed up so as to free up resources and reduce waiting times for new referrals from the community. In addition, the huge numbers of individuals with colonic polyps across the island made it difficult for a centralized system to monitor the status of these individuals.
This inability to adhere to guidelines may potentially result in implications for healthcare cost as well as the clinical outcome of the patient (14). Our study showed that 1% of these patients who had their surveillance scopes performed later had colon cancer. Whether this newly diagnosed cancer really developed in such a short period of time or was missed in the index colonoscopy is debatable. But what is certain is that the stage of the cancer would definitely be earlier if it was diagnosed earlier than later.
On the flip side, if surveillance colonoscopy was performed more frequently than recommended, patients may be subjected to the unnecessary risks of the procedure, the worst being colonic perforation (14). This practice may also deprive others of the availability of the endoscopy and also increase the healthcare cost. Our study showed that none of the 113 patients whom underwent surveillance colonoscopy earlier than recommended has colon cancer, though almost half of them (49.2%) had polyps detected. Whether these were missed at the index colonoscopy is questionable. There are likely to be some individuals who are perhaps more predisposed to polyp development due to inherent and acquired risks. Diagnosing and categorizing these “higher risk” individuals through further translational research in the future will be one way to better guide the screening protocol.
Currently, our audit showed that much work is necessary to improve compliance to the guidelines. The authors believed that this is a problem that is faced by numerous institutions worldwide. To tackle the issue of compliance following colonic polypectomy requires a multi-prong approach, education of patients and physicians on the importance of surveillance and its protocol is integral. It is no longer far-fetched how technological advancement will change the way healthcare is governed. Simple but massive changes such as personal automated reminders to the patients through whichever means and enabling physicians and hospital administrators the ease of conducting audits of compliance are such simplistic examples. The future of Artificial Intelligence and Big Data in the field of medicine is limitless.
But to focus on the sole issue of compliance to guidelines following colonic polypectomy is to miss the big picture of primary and secondary prevention of CRC. Research from both health-services and translational aspects are integral to reduce the burden of this disease. Better understanding of the barriers towards screening and targeted interventions to improve adoption of screening is a start. But if we were able to identify which individuals will ever develop polyps and CRC through further translational research using serological, colonic mucosal and even faecal samples would change the field of CRC screening altogether.
The authors acknowledge that this being a retrospective study conducted for the year 2008 is subjected to numerous biases. Several of the patients who were classified as “having their colonoscopy later or lost to follow up” could have had their colonoscopy done in other hospitals which is therefore not recorded. The small sample size by limiting the year of review to only 2008 is another limitation. Even though the number of colonoscopy is higher in the subsequent years and with better documentations of the colonoscopic findings, the authors felt that a 10-year follow-up period was necessary to evaluate long-term data.
Conclusions
The current compliance rate following colonoscopic polypectomy is abysmal and implications from non-compliance are considerable. More work is required from all parties to improve this observation.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Institutional Review Board of National Healthcare Group (No. 2013/00188) and informed consent from participants were waived in keeping with a review of medical records.
References
- Kuipers EJ, Rösch T, Bretthauer M. Colorectal cancer screening--optimizing current strategies and new directions. Nat Rev Clin Oncol 2013;10:130-42. [Crossref] [PubMed]
- Zorzi M, Fedeli U, Schievano E, et al. Impact on colorectal cancer mortality of screening programmes based on the faecal immunochemical test. Gut 2015;64:784-90. [Crossref] [PubMed]
- Libby G, Brewster DH, McClements PL, et al. The impact of population-based faecal occult blood test screening on colorectal cancer mortality: a matched cohort study. Br J Cancer 2012;107:255-9. [Crossref] [PubMed]
- Faivre J, Dancourt V, Lejeune C, et al. Reduction in colorectal cancer mortality by fecal occult blood screening in a French controlled study. Gastroenterology 2004;126:1674-80. [Crossref] [PubMed]
- Hassan C, Quintero E, Dumonceau JM, et al. Post-polypectomy colonoscopy surveillance: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2013;45:842-51. [Crossref] [PubMed]
- Lieberman DA, Rex DK, Winawer SJ, et al. Guidelines for colonoscopy surveillance after screening and polypectomy: a consensus update by the US Multi-Society Task Force on Colorectal Cancer. Gastroenterology 2012;143:844-57. [Crossref] [PubMed]
- Yang DH, Hong SN, Kim YH, et al. Korean guidelines for postpolypectomy colonoscopy surveillance. Clin Endosc 2012;45:44-61. [Crossref] [PubMed]
- Dominitz JA, Eisen GM, Baron TH, et al. Complications of colonoscopy. Gastrointest Endosc 2003;57:441-5. [Crossref] [PubMed]
- Menees SB, Elliott E, Govani S, et al. The impact of bowel cleansing on follow-up recommendations in average-risk patients with a normal colonoscopy. Am J Gastroenterol 2014;109:148-54. [Crossref] [PubMed]
- Goodwin JS, Singh A, Reddy N, et al. Overuse of screening colonoscopy in the Medicare population. Arch Intern Med 2011;171:1335-43. [Crossref] [PubMed]
- Schoen RE, Pinsky PF, Weissfeld JL, et al. Utilization of surveillance colonoscopy in community practice. Gastroenterology 2010;138:73-81. [Crossref] [PubMed]
- Saini SD, Nayak RS, Kuhn L, et al. Why don't gastroenterologists follow colon polyp surveillance guidelines?: results of a national survey. J Clin Gastroenterol 2009;43:554-8. [Crossref] [PubMed]
- Iskandar H, Yan Y, Elwing J, et al. Predictors of Poor Adherence of US Gastroenterologists with Colonoscopy Screening and Surveillance Guidelines. Dig Dis Sci 2015;60:971-8. [Crossref] [PubMed]
- Patel N, Tong L, Ahn C, et al. Post-polypectomy Guideline Adherence: Importance of Belief in Guidelines, Not Guideline Knowledge or Fear of Missed Cancer. Dig Dis Sci 2015;60:2937-45. [Crossref] [PubMed]


