A case report of HCC cutaneous metastasis
Introduction
Hepatocellular carcinoma (HCC) is one of the most common solid tumors in the world. The prognosis is severe according to the stage at diagnosis, the degree of differentiation and the possibility of a curative treatment. The 50% of recurrences in patients undergoing surgery occurs in the intrahepatic site. The extrahepatic metastases are uncommon and they usually occur in the lung, adrenal, bone. HCC muscle and skin metastases are rare and may occur by hematogenous spread or during surgical procedures.
Case report
In January 1999 a 47-year-old Caucasian man, otherwise healthy, smoker, obese, no alcohol use, underwent an abdominal ultrasound which revealed a severe fatty liver and an isoechoic mass (5 cm × 6 cm in diameter) in liver segment 2-4.
Liver function test and alpha-fetoprotein were within normal range, hepatitis viral markers were all negative.
Computed tomography (CT) scan confirmed the hepatic injury without distant metastases. Arteriography of the celiac, superior mesenteric and hepatic artery revealed 5.6 cm hypervascular hepatic mass. Percutaneous liver biopsy was performed followed by surgical resection of liver segment 3 in February 1999.
Histopathological examination showed a moderately differentiated HCC (according to Edmondson-Steiner).
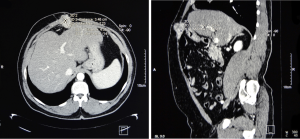
Follow-up was negative until February 2010, when the patient presented to our attention with hard, non painful, 4 cm, palpable nodules in the surgical scar of the anterior abdominal wall. Oncological markers (alpha-fetoprotein, CEA, CA19.9) and hepatitis viral markers were all negative. Laboratory results showed mildly elevated transaminases (AST 50 IU, ALT 56 IU) and GGT (161 IU). Abdominal CT revealed a solid inhomogeneous and hypervascular tissue (3.5 cm × 4.3 cm × 5.4 cm in diameter) close to the right abdominal rectus muscle extending into the subcutaneous adipose tissue (Figure 1).
The patient underwent en bloc resection of the tumor with the right abdominal rectus muscle and liver biopsy.
Histological examination
Macroscopic: skin of 9.5 cm × 2 cm which underlied fibro-adipose and muscle tissue, in the middle of adipose tissue and at 1.5 cm from the skin there was a lobulated brown nodular tumor with indistinct margins (5 cm × 4 cm × 4 cm).
Microscopic: moderately differentiated (grade II according to Edmondson and Steiner) HCC cutaneous metastasis, pseudoglandular pattern, with lymphovascular invasion, infiltration of muscular tissue, presence of biliar pigment. Hepatocyte was positive, alpha-fetoprotein, CEA, EMA, CK7, CK19, NSE, Chromogranin, Synaptophysin and HMB-45 were negative. Skin and resection margins were free (Figure 2).
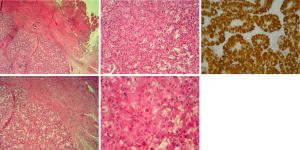
Follow-up was negative until March 2011 when the patient presented with two hard, fixed, palpable, painless nodules in the epigastric surgical scar. Laboratory tests showed increased transaminases (AST 78 IU, ALT 64 IU), and GGT (432 IU), alkaline phosphatase (156 IU), normal alphafetoprotein; a CT revealed close to liver in the muscle wall two contiguous solid nodules (1.5 cm and 2.7 cm × 1.4 cm × 2.8 cm in diameter) with intense and homogeneous contrastographic impregnation compatible with locoregional recurrence. In May 2011 the patient underwent resection of the tumor. Histopathological examination showed moderately differentiated HCC subcutaneous metastases. The morphology was similar to the previous (Figure 2).
In November 2011 the patient presented with an intrahepatic relapse so we started Sorafenib. He had stable disease until February 2013 when CT revealed hepatic progression.
Discussion
Our case has three peculiarities:
- Skin and muscle metastatic site probably caused by tumor cells seeding. In literature HCC muscle and cutaneous metastases are caused by diagnostic procedures or locoregional ablative treatments (1). Risk of tumor seeding with liver biopsy is estimated of 2.29%, with PEI (percutaneous ethanol injection) and biopsy was 1.4% while 0.61% with radiofrequency ablation (RFA) without biopsy and 0.95% with RFA and biopsy (2). Other authors confirm that liver biopsy followed by RFA was related to a significant increase in tumor seeding (P=0.004) (2). In literature these factors are lead to tumor cell seeding following diagnostic procedures: subcapsular lesion, low degree of differentiation, alpha fetoprotein elevated level, tumor diameter >5 cm (3,4).
In our case these factors were not found except for the tumor diameter. Our patient underwent liver biopsy followed by radical surgical resection but it is impossible define the cause of tumor cell seeding. - The time between the surgery and the first relapse. In literature this time is shorter; in a large series of 1,314 patients undergone RFA followed or not by liver biopsy was 37 months (3).
- Further muscle metastasis after one year from radical surgery of cutaneous metastasis which is also caused by tumor cell seeding of the abdominal wall during surgery and/or diagnostic procedures.
Conclusions
The spread of HCC to the soft tissues of the abdominal wall is possible and more frequently following liver biopsy.
In the follow-up of patients who underwent surgical resection or diagnostic and therapeutic procedures for HCC should be considered the possibility of abdominal wall metastasis even after many years, particularly in the cases with favorable evolution.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Rowe LR, Mulvihill SJ, Emerson L, et al. Subcutaneous tumor seeding following needle core biopsy of hepatocellular carcinoma. Diagn Cytopathol 2007;35:717-21. [PubMed]
- Stigliano R, Marelli L, Yu D, et al. Seeding following percutaneous diagnostic and therapeutic approaches for hepatocellular carcinoma. What is the risk and the outcome? Seeding risk for percutaneous approach of HCC. Cancer Treat Rev 2007;33:437-47. [PubMed]
- Livraghi T, Lazzaroni S, Meloni F, et al. Risk of tumour seeding after percutaneous radiofrequency ablation for hepatocellular carcinoma. Br J Surg 2005;92:856-8. [PubMed]
- Imamura J, Tateishi R, Shiina S, et al. Neoplastic seeding after radiofrequency ablation for hepatocellular carcinoma. Am J Gastroenterol 2008;103:3057-62. [PubMed]


