Posterior reversible leukoencephalopathy syndrome secondary to hepatic transarterial chemoembolization with doxorubicin drug eluting beads
Introduction
Uveal melanoma (UM) is a rare, yet let lethal malignancy that has an age-adjusted incidence of approximately 5.1 per one million (1). The most common cause of death in UM patients is secondary to metastases, of which liver is the most common site (2). UM patients with liver metastases have a poor prognosis, with medial survival between 2-7 months despite aggressive therapy (3). There is a paucity of standardized treatment options for UM patients with liver metastases, however transarterial chemoembolization (TACE) directed at UM liver metastases can be performed with several different chemotherapeutic agents and drug delivery systems, with drug eluting beads (DEBs) accumulating significant data in recent years. Delivering chemotherapeutic agents such as doxorubicin via DEBs (DEBDOX, Biocompatibles UK Limited, Surrey, UK) is aimed at reducing potentially harmful systemic toxicity by targeting specific hepatic metastases through slow release of medication.
Case report
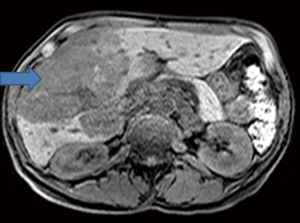
A 56-year-old female diagnosed with UM with liver metastasis was placed on local TACE treatment. She received three TACE treatments with Carmustine, and one TACE with DEBDOX. An MRI done after these cycles showed persistence of extensive liver metastasis despite the above mentioned therapy (Figure 1). She was therefore treated with a second cycle of TACE-DEBDOX one month later. Eighteen hours after TACE-DEBDOX, the patient experienced expressive aphasia, bilateral blurry vision, dysarthria and dysmetria. Abdominal exam revealed mild hepatomegaly and upper abdominal tenderness without guarding or rigidity. Her blood pressure (BP) had been slowly trending up after the TACE with a peak of 180/113 (mean arterial pressure =135 mmHg) 12 hours after the procedure; this was treated with intravenous metoprolol. Laboratory investigations revealed an elevated AST (309 IU/L) and ALT (199 IU/L) with a normal total bilirubin of 0.3 mg/dL.
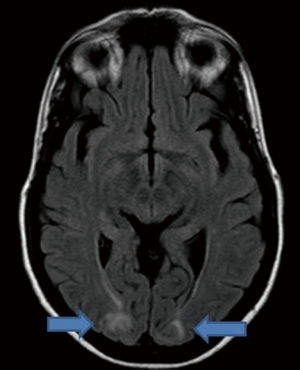
Brain MRI showed a hyper intense signal in the subcortical white matter of the bilateral occipital lobes, consistent with posterior reversible encephalopathy syndrome (PRES) (Figure 2). Since her PRES was attributed to significantly elevated BP as a result of chemotherapy, aggressive control of her hypertension was initiated. Reduction of the mean arterial pressure to goal resulted in resolution of her symptoms within 24 hours. The patient did well and was discharged from the hospital.
Discussion
PRES, initially reported by Hinchey et al. in 1996 (4), is both a clinical and a radiologic diagnosis. While the pathogenesis of PRES is not entirely understood, proposed mechanisms include cerebral blood flow dysregulation leading to hyperperfusion, cerebral ischemia, and increased endothelial cell permeability resulting in cerebral edema (5). This syndrome includes neurologic symptoms such as visual changes, seizures, headaches, altered mental status and paresis that can develop acutely or over several days (5). Elevated BP is seen in ~75% of patients with PRES (5). Classic findings include symmetric edema of focal regions of white matter, seen most commonly in the parietooccipital lobes on T2 MRI imaging. Most patients improve quickly with BP treatment and have resolution of neurologic symptoms within two weeks.
Our case is the first report of PRES secondary to TACE-DEBDOX in a patient with liver metastases from UM. There is only one prior case reported of PRES secondary to TACE-DEBDOX reported in a breast cancer patient (6). PRES has been associated with systemic chemotherapy, including doxorubicin (7); however there is significantly less data and experience with local administration through TACE-DEBDOX. Since elevated BP is a known complication of TACE (8,9), the procedure itself could make these patients more susceptible to the side effects of chemotherapeutics such as doxorubicin, even if they are locally administered. As our patient underwent five TACE procedures, two of which involved DEBDOX, there may be a role for cumulative effects on the cerebral endothelial cell permeability and blood flow regulation.
Due to the poor prognosis and limited lifespan in this type of patient, it is possible that complications such as PRES have been underreported. Considering how frequent liver metastases are in UM and the increasing use of TACE-DEBDOX in these patients, we offer this case to assert that these patients should be closely monitored for new complications such as PRES.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Singh AD, Turell ME, Topham AK. Uveal melanoma: trends in incidence, treatment, and survival. Ophthalmology 2011;118:1881-5. [PubMed]
- Woodman SE. Metastatic uveal melanoma: biology and emerging treatments. Cancer J 2012;18:148-52. [PubMed]
- Barbazetto IA, Lee TC, Rollins IS, et al. Treatment of choroidal melanoma using photodynamic therapy. Am J Ophthalmol 2003;135:898-9. [PubMed]
- Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med 1996;334:494-500. [PubMed]
- Bartynski WS. Posterior reversible encephalopathy syndrome, part 1: fundamental imaging and clinical features. AJNR Am J Neuroradiol 2008;29:1036-42. [PubMed]
- Pawar PS, Noviawaty I, Zaidat OO. Unusual case of intra-arterial doxorubicin chemoembolization-associated posterior reversible encephalopathy syndrome. Neurologist 2012;18:49-50. [PubMed]
- Edwards MJ, Walker R, Vinnicombe S, et al. Reversible posterior leukoencephalopathy syndrome following CHOP chemotherapy for diffuse large B-cell lymphoma. Ann Oncol 2001;12:1327-9. [PubMed]
- Basile A, Carrafiello G, Ierardi AM, et al. Quality-improvement guidelines for hepatic transarterial chemoembolization. Cardiovasc Intervent Radiol 2012;35:765-74. [PubMed]
- Tasneem AA, Abbas Z, Luck NH, et al. Adverse events following transarterial chemoembolization for hepatocellular carcinoma and factors predicting such events. J Pak Med Assoc 2013;63:239-44. [PubMed]


