Endoscopic stenting should be advocated in patients with stage IV colorectal cancer presenting with acute obstruction
Introduction
In patients with metastatic colorectal cancers presenting with acute large bowel obstruction, there is the need to alleviate the obstruction, whilst bearing in mind that disease load and response to chemotherapy often determines their prognosis (1). The timing of chemotherapy administration is largely dependent on how early the patient can recover from the insult of the acute presentation. In recent years, endoscopic stenting has emerged as an alternative approach to patients presenting with such obstructed cancers, and needs to be considered in the light of the above considerations.
Endoscopic stenting enables prompt relief of the obstruction and should enable earlier commencement of chemotherapy (2,3). However, its complications include failure of the stent which would require immediate surgery to relieve the obstruction. Earlier studies have reported that emergency surgery following an episode of failed stenting may be associated with worse complications than upfront emergency surgery (4,5). Morbidities following major surgery for colonic obstruction are significant, while less extirpative surgeries such as defunctioning stoma have implications on the patients’ quality of life (6).
We undertook this study to compare the outcomes between endoscopic stenting and upfront emergency surgery in patients with metastatic colorectal cancers presenting with acute large bowel obstruction.
Methods
A retrospective review of all patients with metastatic colorectal carcinoma presenting with acute large bowel obstruction from January 2007 to June 2014 was performed. Only those who underwent emergency surgery or endoscopic stenting were included for the purpose of this study. The study was reviewed and approved by the institutional review board.
In our institution, a computed tomographic (CT) scan is typically performed within 12 hours of admission in all suitable patients presenting with features suggestive of colonic obstruction. Patients presenting with a guarded abdomen and were haemodynamically unstable were sent straight to the operating theatre instead.
Once the diagnosis of metastatic colorectal cancer causing large bowel obstruction was confirmed, the immediate aim was to alleviate the obstruction. This was performed via endoscopic stenting or emergency surgery. These two approaches form the main arms of comparison in our study. The decision to undergo either approach made at the clinical discretion of the consultant colorectal surgeon.
For endoscopic stenting, technical success was defined as the successful placement and deployment of the stent, while clinical success was defined as the presence of colonic decompression within 48 hours of successful placement of the stent, with resolution of the symptoms of large bowel obstruction.
Apart from patient demographics, extent of disease, type of procedure performed, the severity of the post-procedural complications is graded according to the classification proposed by Clavien and colleagues (7-9). Grade III and above complications were defined as severe. The dates of commencement of subsequent chemotherapy and the duration of survival were also documented. The study was analyzed with an intention to treat basis.
Categorical and continuous variables were analysed using the Fisher’s exact test and Mann Whitney U test, respectively. The overall survival probability was estimated using the Kaplan-Meier method. All analyses were performed using the Statistical Package for the Social Sciences version 18.0 (SPSS, Chicago, Illinois, USA) and P values of <0.05 were considered statistically significant.
Results
During the study period, 66 patients with metastatic colorectal cancers presenting with large bowel obstruction underwent either attempted stenting or emergency surgery to relieve the obstruction (Table 1). Twenty-six (39.4%) patients underwent immediate surgery with no attempt at endoscopic stenting. The remaining 40 (60.6%) patients had endoscopic stenting attempted, of which 29 (72.5%) were successful. All patients who achieved technical success also attained clinical success with resolution of their symptoms following the procedure. The 11 (27.5%) patients who failed endoscopic stenting underwent immediate surgery to relieve the obstruction. The commonest site of the obstruction for the stenting group was at the sigmoid colon (n=26, 65%). The majority of the metastases were seen in the liver (n=46, 69.7%).
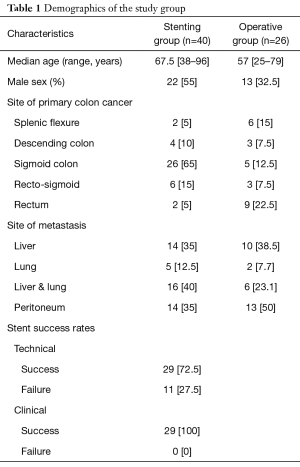
Full table
Post-procedural outcomes
Amongst the 26 patients who underwent emergency open surgery, an anterior resection was performed in 5 (19.2%) patients. Nine of these patients did not have any resection performed, with 6 of them having a defunctioning loop stoma created while 3 patients underwent a bypass procedure. Two patients from this group died on their index admission. One patient with an ileo-descending bypass experienced a massive acute myocardial infarction a few hours after the operation and passed away. The second patient died from septic shock and disseminated intravascular coagulopathy (DIVC).
In the 29 patients who were successfully stented, 14 underwent elective surgery at a median duration of 18.7 (range, 1.3–99.1) weeks. The majority of these surgeries were segmental resection of the malignancy, with 4 having defunctioning stomas and 1 undergoing a bypass procedure. Two patients required emergency surgeries when they developed stent complications 1 and 2 months after the stents were inserted. Stent-related perforation of the tumor occurred in both patients and emergency surgery was performed to remove the affected segment. One passed away from the subsequent septic shock. Table S1 illustrates the surgeries performed in this study group. In the remaining 13 patients, 7 declined surgery post-stenting and opted for palliative management while 6 patients did not follow-up after they were discharged.
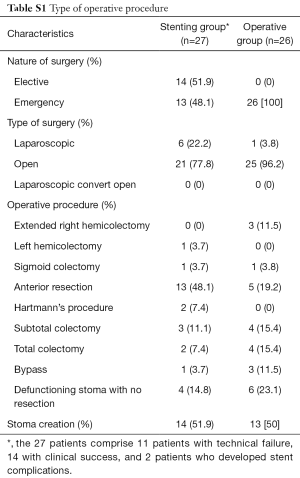
Full table
The group of patients who failed the stenting procedure and underwent emergency surgery were 23 times more likely to develop severe complications compared to the group who were successfully stented [odds ratio (OR), 23.3; 95% confidence interval (CI), 2.29–250.00, P=0.004] (Table 2). Comparing patients who had emergency surgery following failed stenting and those who had immediate surgery, there was no statistical significant difference, although worse outcome in the failed stenting group was also observed (P=0.09). Patients who underwent emergency surgery upfront had a longer median length of stay compared to those patients who had a successful endoscopic stenting procedure (P=0.003) (Table S2).
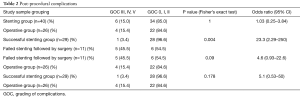
Full table
Full table
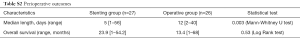
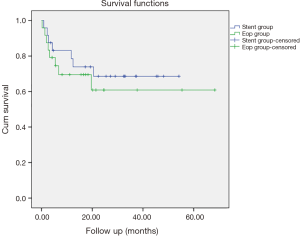
Commencement of palliative chemotherapy
The number of patients who received palliative chemotherapy was comparable in both the stenting and operative groups (59.3% and 61.5%). The group of patients who were stented received chemotherapy earlier (median: 4.3; 1–6.7 weeks) than those who underwent immediate surgery upfront (median: 7; 1.3–84 weeks) (P=0.02) (Tables 3,4). Both groups had comparable disease specific mortality rates (33.3% vs. 34.6%) though overall survival was longer in the group that was stented, albeit it being statistically insignificant (23.9 vs. 13.4 months, P=0.076) (Figure 1).

Full table
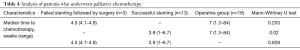
Full table
Discussion
Endoscopic stenting is an alternative to surgery in the management of patients with acute intestinal obstruction from stage IV colorectal cancer. Success rates of 70% to 90% have been reported (10-12). Some of the advantages include lesser morbidity from an elective procedure, less extensive surgical resection, avoidance of a stoma (13-17), possibility of a laparoscopic procedure to be performed (18,19) and a shorter hospitalization stay (6). These were also observed in our study.
The importance of chemotherapy after surgery in metastatic colorectal cancers cannot be understated (20-24). Not only does it prolong the median survival, it also increases the possibility of downstaging previously unresectable metastatic disease (25). To allow these patients the chance to have better long-term outcome, the ability to administer chemotherapy within a certain therapeutic window is important, beyond which, the benefits are questionable.
Patients who had successful stenting had the best outcomes. Interestingly, patients who failed stenting and required emergency surgery did not fare worse when compared with these patients who had upfront emergency surgery. The authors acknowledge that factors such as the angulation of the tumour to the lumen and the experience of the endoscopist are predictive of the success of the procedure and must be taken into consideration before wholesale adoption of endoscopic stenting. Moreover, the possibility of the stent giving rise to complications while the patient is undergoing chemotherapy is a genuine concern. Stent related perforation and migration can be encountered and managing these complications during their chemotherapy cycle can be associated with disastrous outcomes.
Our findings translated to earlier commencement of chemotherapy in the patients with successful stenting, and no delay in the commencement of chemotherapy between patients who failed stenting and who had upfront emergency surgery. This suggests that endoscopic stenting may be considered in stage IV colorectal cancer patients with acute large bowel obstruction, barring any signs of clinical peritonism or contraindication to endoscopic stenting.
More importantly, numerous recent studies have confirmed the significant improvement in the quality of life in stage IV colorectal cancers who were successfully stented for their malignant obstruction. A randomized controlled trial performed by Young et al. showed that stenting in patients with obstructed stage IV disease was associated with better quality of life outcomes when compared to baseline at 1 week, and at 12 months (P=0.001 and P=0.01), without worse clinical outcomes in terms of 30-day mortality and median overall survival (26). This concurs with earlier non-randomized studies which have shown improved overall quality of life, as well as quality of life relating to gastrointestinal symptoms in patients who underwent stenting instead of emergency surgical decompression (27).
Our study shows that stenting enables these stage IV patients to undergo chemotherapy earlier than those who underwent upfront surgery, even though both were within a 12 weeks therapeutic window (28). Our study, however, did not demonstrate any survival benefit between the two groups. Limitations to our study include the small sample size, as well as the potential selection bias which arose due to the decision for stenting or emergency upfront surgery being made at the discretion of the consultant colorectal surgeon. As a result, there was heterogeneity in our comparison groups, such as in the proportion of patients with a rectal lesion that underwent stenting versus upfront surgery.
Conclusions
Endoscopic stenting is an option in patients with metastatic colorectal cancers presenting with acute large bowel obstruction. Patients who have undergone successful stenting commence chemotherapy earlier than those with upfront surgery without stenting. Patients who fail stenting and require emergency surgery do not fare worse than patients who undergo upfront surgery without stenting.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical statement: The study was approved by the National Healthcare Group Domain Specific Review Board (NHG DSRB). NHG DSRB Reference number: 2012/00707 and informed consent was taken from all the patients.
References
- Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg 1994;81:1270-6. [Crossref] [PubMed]
- Abbott S, Eglinton TW, Ma Y, et al. Predictors of outcome in palliative colonic stent placement for malignant obstruction. Br J Surg 2014;101:121-6. [Crossref] [PubMed]
- Tan CJ, Dasari BV, Gardiner K. Systematic review and meta-analysis of randomized clinical trials of self-expanding metallic stents as a bridge to surgery versus emergency surgery for malignant left-sided large bowel obstruction. Br J Surg 2012;99:469-76. [Crossref] [PubMed]
- Lim TZ, Chan D, Tan KK. Patients who failed endoscopic stenting for left-sided malignant colorectal obstruction suffered the worst outcomes. Int J Colorectal Dis 2014;29:1267-73. [Crossref] [PubMed]
- Liang J, Church JM, Stocchi L, et al. Should bypass or stoma creation be undertaken for unresectable stage IV colorectal carcinoma? ANZ J Surg 2014;84:275-9. [Crossref] [PubMed]
- Tan KK, Sim R. Surgery for obstructed colorectal malignancy in an Asian population: predictors of morbidity and comparison between left- and right-sided cancers. J Gastrointest Surg 2010;14:295-302. [Crossref] [PubMed]
- Clavien PA, Sanabria JR, Mentha G, et al. Recent results of elective open cholecystectomy in a North American and a European center. Comparison of complications and risk factors. Ann Surg 1992;216:618-26. [Crossref] [PubMed]
- Clavien PA, Camargo CA Jr, Croxford R, et al. Definition and classification of negative outcomes in solid organ transplantation. Application in liver transplantation. Ann Surg 1994;220:109-20. [Crossref] [PubMed]
- Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 2004;240:205-13. [Crossref] [PubMed]
- Camunez F, Echenagusia A, Simo G, et al. Malignant colorectal obstruction treated by means of self-expanding metallic stents: effectiveness before surgery and in palliation. Radiology 2000;216:492-7. [Crossref] [PubMed]
- Sebastian S, Johnston S, Geoghegan T, et al. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol 2004;99:2051-7. [Crossref] [PubMed]
- Keranen I, Lepisto A, Udd M, et al. Stenting for malignant colorectal obstruction: a single-center experience with 101 patients. Surg Endosc 2012;26:423-30. [Crossref] [PubMed]
- Phillips RK, Hittinger R, Fry JS, et al. Malignant large bowel obstruction. Br J Surg 1985;72:296-302. [Crossref] [PubMed]
- Anderson JH, Hole D, McArdle CS. Elective versus emergency surgery for patients with colorectal cancer. Br J Surg 1992;79:706-9. [Crossref] [PubMed]
- Ascanelli S, Navarra G, Tonini G, et al. Early and late outcome after surgery for colorectal cancer: elective versus emergency surgery. Tumori 2003;89:36-41. [Crossref] [PubMed]
- Alvarez JA, Baldonedo RF, Bear IG, et al. Presentation, treatment, and multivariate analysis of risk factors for obstructive and perforative colorectal carcinoma. Am J Surg 2005;190:376-82. [Crossref] [PubMed]
- Sjo OH, Larsen S, Lunde OC, et al. Short term outcome after emergency and elective surgery for colon cancer. Colorectal Dis 2009;11:733-9. [Crossref] [PubMed]
- Lee HJ, Park SJ, Cheon JH, et al. What is the necessity of endoscopist for successful endoscopic stenting in patients with malignant colorectal obstruction? Int J Colorectal Dis 2015;30:119-25. [Crossref] [PubMed]
- Lee JH, Yoon JY, Park SJ, et al. The learning curve for colorectal stent insertion for the treatment of malignant colorectal obstruction. Gut Liver 2012;6:328-33. [Crossref] [PubMed]
- Kemmochi T, Egawa T, Mihara K, et al. Neoadjuvant chemotherapy with capecitabine plus oxaliplatin and bevacizumab for the treatment of patients with resectable metastatic colorectal cancer. Gan To Kagaku Ryoho 2013;40:1629-31. [PubMed]
- Misiakos EP, Karidis NP, Kouraklis G. Current treatment for colorectal liver metastases. World J Gastroenterol 2011;17:4067-75. [Crossref] [PubMed]
- Kleespies A, Fuessl KE, Seeliger H, et al. Determinants of morbidity and survival after elective non-curative resection of stage IV colon and rectal cancer. Int J Colorectal Dis 2009;24:1097-109. [Crossref] [PubMed]
- Giuliante F, Ardito F, Vellone M, et al. Role of the surgeon as a variable in long-term survival after liver resection for colorectal metastases. J Surg Oncol 2009;100:538-45. [Crossref] [PubMed]
- Wei AC, Greig PD, Grant D, et al. Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol 2006;13:668-76. [Crossref] [PubMed]
- Dienstmann R, Salazar R, Tabernero J. Personalizing colon cancer adjuvant therapy: selecting optimal treatments for individual patients. J Clin Oncol 2015;33:1787-96. [Crossref] [PubMed]
- Young CJ, De-Loyde KJ, Young JM, et al. Improving Quality of Life for People with Incurable Large-Bowel Obstruction: Randomized Control Trial of Colonic Stent Insertion. Dis Colon Rectum 2015;58:838-49. [Crossref] [PubMed]
- Nagula S, Ishill N, Nash C, et al. Quality of life and symptom control after stent placement or surgical palliation of malignant colorectal obstruction. J Am Coll Surg 2010;210:45-53. [Crossref] [PubMed]
- Dos Santos LV, Faria TM, Lima AB, et al. Timing of adjuvant chemotherapy in colorectal cancer. Colorectal Dis 2016;18:871-6. [Crossref] [PubMed]


