Colorectal lymphoma in Mexico: clinico-pathological and survival analysis
Introduction
Lymphomas are the most frequent malignant tumors in the lymph nodes, although a substantial number occur at extranodal sites. (1) Extranodal lymphomas are more frequently located in the gastrointestinal tract, lungs, axial skeleton and skin (2). Gastrointestinal lymphomas are rare and they represent between 1–4% of all malignant gastrointestinal neoplasms (3), and less than 1% of colorectal malignances (4). In the gastrointestinal tract, 10–20% are present in the colorectum (5). The age of presentation has a bimodal distribution, with a peak of frequency before 15 years of age, and another between the fifth and sixth decade of life (6).
In view of the recent outcomes when treating this disease utilizing combined therapeutic modalities (7), it has become necessary to promptly identify the symptoms patients present with this type of neoplasm in order to facilitate an early diagnosis and to define the best treatment.
The median survival of the reported cases ranges from 24 to 36 months (4), but some authors have reported an improvement of up to 36 to 53 months with the use of adjuvant chemotherapy (8).
In Mexico and Latin America, there are few data regarding the frequency of this condition, so we consider it necessary to establish an approximate frequency of the disease, and to identify the clinico-pathological characteristics of these patients in order to increase their detection and improve their prognoses.
Methods
A retrospective cross-sectional study was carried out on patients from a third-level hospital (Instituto Nacional de Cancerología de México). From the pathology files, all consecutive cases of colorectal tumors from January 01, 2006 to December 31, 2016 were reviewed. A primary colorectal lymphoma (PCL) was defined following Dowson et al.’s (9) criteria as a case of a histopathologically confirmed lymphoma that presented in the colon or rectum without any evidence of synchronous affection at the extra-colorectal sites and without a history of lymphoma in another localization, and normal blood cell counts, and, finally, we accepted cases that showed lymph node involvement at the drainage site of the colorectal lesion.
The clinical pathological variables recorded from the clinical and pathological records were age, sex, a personal history of systemic arterial hypertension, diabetes, obesity, constipation, digestive bleeding, diarrhea, body mass index, abdominal distension, date of diagnosis, date of last follow-up, treatment, B symptoms, tumor location, tumor size, number of lesions, depth of invasion and outcome of the patient. For the outcome, the patients’ condition at the time of their last visit is considered, thus placing them in one of the following categories: free of disease, died from the disease, alive with the disease and died from another cause.
To analyze the data, we performed descriptive statistics with frequencies expressed as numbers, medians with interquartile range and inferential statistics, contrasting between groups using a Chi square or Fisher’s exact test for the categorical variables, and a Mann-Whitney U test for the numerical variables, with a level of significance P<0.05. A survival analysis was performed using the Kaplan-Meier method. A multivariate analysis was performed using the Cox proportional hazards model with a stepwise forward selection. All the P values were two-sided, with the hazard ratios at 95% confidence intervals.
Results
We retrieved 1,229 cases of colorectal neoplasms; of these, 1,083 (88.1%) were carcinomas, 56 (4.5%) were neuroendocrine neoplasms, 40 (3.3%), were gastrointestinal stromal tumors (GISTs), 6 (0.49%) were sarcomas and 44 (3.6%) were lymphomas, but only 18 (1.5% of the total) were considered to be PCL.
The data of the 18 cases of PCL are summarized in Tables 1 and 2. Ten cases (55.6%) presented in men, with a median age of 57 years (interquartile range, 43.5–66.25 years). As shown in Table 1, diffuse large B-cell lymphoma (DLBCL) was the most common subtype with 55.6% of cases, followed by mantle cell lymphoma (16.7%), plasmablastic and Burkitt lymphomas (11.1% for each), and follicular lymphoma (5.6%).
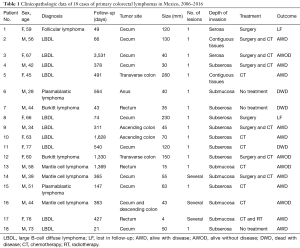
Full table

Full table
The most common location was the cecum, with 10 cases (55.6%), followed by the rectum with 3 (16.7%), the ascending and transverse colon with 2 cases each (11.1%), and 1 case in the anus. Most of the tumors (83.4%) presented as unique polypoid tumors. The median size was 52.5 mm (interquartile range, 38.75–122.5 mm), with 50% of tumors invading the entire wall depth until the subserous adipose tissue, whereas 27.8% presented in the submucosa, but 22.2% extended to the serosa and contiguous tissues.
The most prevalent symptom was abdominal pain (61.1%), followed by weight loss (50%), constipation (44.4%), gastrointestinal bleeding (44.4% corresponding to 8 patients, of which 7 presented as rectorragia or melena, and only 1 case presented with fecal occult blood), “B” symptoms (33.3%), abdominal distension (27.8%), diarrhea (22.2%) and hyporexia (11.1%).
The patients’ personal backgrounds showed that 27.8% were diabetic, 5 (27.8%) had a background of cancer (familial), 4 (22.2%) had an HIV infection, 2 (11.1%) had systemic arterial hypertension and two were obese. The median body mass index was 23.67 (interquartile range, 21.15–27.37).
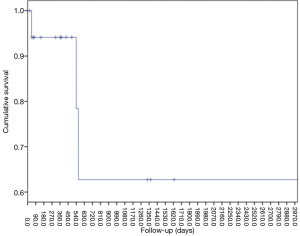
With regard to the outcome, the patients were followed up at a median of 371.5 days (interquartile range, 72–755.5 days), 6 cases (33%) received initial surgery followed by chemotherapy, 7 cases (39%) received only chemotherapy, two cases received only surgery and three cases did not receive treatment. At the final visit, 3 patients (16.7%) had died of disease and 9 patients (50%) were alive with the disease, while only 4 (22.2%) were alive and free of the disease. Two cases had been lost at the follow-up. The 2-year disease-specific survival rate in our series was 62.7% (Figure 1), with a mean survival rate of 79.7 months.
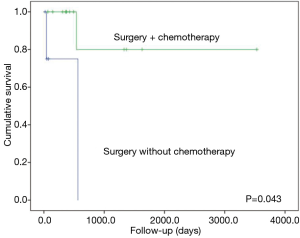
The only factors associated with improved overall survival in the univariate analysis were the use of surgery followed by chemotherapy (P=0.043, Figure 2) and an HIV-negative status (P=0.043). Age, sex, surgery, subtype, symptoms, weight loss, BMI, obesity and tumor size were not significantly associated with survival.
In the multivariate analysis none of the factors was an independent risk factor for decreased survival.
Discussion
PCL is a very rare disease; in our series it corresponded to 1.46% of the primary colorectal neoplasms. From 18 cases, 55.6% presented in men, the median age was 57 years, all the cases were B-cell lymphoma, eight cases received surgery, seven cases received chemotherapy and three cases did not receive treatment. The factors associated with poor prognosis in the univariant analysis were an HIV-positive status and non-surgical treatment.
PCL represents from 0.1% to 0.6% of colorectal malignances (10-13), but in our institution we found a higher frequency (1.4%), perhaps due to the fact that our institution is a national cancer center, with a concentration of rare or difficult cases. The median age in our series was in agreement with the published literature in Caucasian populations (6-10), but higher than in Asian populations, where the median age ranges from 34.1 to 51 years (13,14). According to published studies, our cases were more prevalent in men and, interestingly, four patients had an HIV infection. This finding was only found in one case out of the 43 patients reported by Drolet et al. (10). In addition, Tevlin et al. (6) in their series of 11 patients, two presented immunosuppression secondary to transplantation.
Regarding the lymphoma subtypes, most of the reported PCLs were of B-cell lineage, ranging from 82% to 100%, where only the Asian series had an occurrence of T cell lymphomas (13,14). In a SEER-based analysis performed by Cai et al. (12) in the U.S., they found a similar proportion of B-cell vs. T-cell lymphomas (53% and 47%, respectively), although they studied cases in adults and children; other series including children also demonstrated the occurrence of T cell lymphomas (13), a fact that appears to be rare in adults. Between the cell subtypes, the most frequent is DLBCL, ranging from 45% to 74% (10-13), and our data are according to this subtype. The second most prevalent subtypes are variegated between the series. The most common location of PCL is the cecum, followed by the rectum (around 60% and 20%, respectively), and the most prevalent symptom is abdominal pain (6,10-14). Our results agree with these findings.
Almost all patients with PCL reported in the literature underwent a surgical resection (3,4,8-14), and the median survival in these series was generally low, ranging from 24 to 36 months. In most series, the majority of patients received adjuvant systemic chemotherapy, whose use has been associated with improved outcomes reaching a 2-year survival rate of around 60% (10,14) and a 5-year survival rate of 53–57% (12-14). However, in one of the largest series, and precisely in Mexican patients, Avilés et al. described an overall survival rate of 83% at 10 years (15). Our findings agree with most series with a 2-year disease specific survival rate of 62.7% with a mean survival rate of 79.7 months. These results suggest that an aggressively treated colorectal lymphoma could improve the prognosis.
Conclusions
In conclusion, most patients present with nonspecific symptoms, which often leads to delays in diagnosis and an advanced stage at presentation. The majority of patients have DLBCL. We found cases associated with immunosuppression (HIV infection). The treatment of colorectal lymphoma generally consists of surgery followed by systemic chemotherapy, and this treatment is the best approach.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Instituto Nacional de Cancerología (NO. 17/139) and written informed consent was not necessary because the retrospective/observational nature of the study and data does not contain identifying information of the patients.
References
- American Cancer Society. Cancer Facts and Figures. Atlanta, GA: American Cancer Society, 2005.
- Zucca E, Roggero E, Bertoni F, et al. Primary extranodal non-Hodgkin’s lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol 1997;8:727-37. [Crossref] [PubMed]
- Doolabh N, Anthony T, Simmang C, et al. Primary colonic lymphoma. J Surg Oncol 2000;74:257-62. [Crossref] [PubMed]
- Fan CW, Changchien CR, Wang JY, et al. Primary colorectal lymphoma. Dis Colon Rectum 2000;43:1277-82. [Crossref] [PubMed]
- She WH, Day W, Lau PY, et al. Primary colorectal lymphoma: case series and literature review. Asian J Surg 2011;34:111-4. [Crossref] [PubMed]
- Tevlin R, Larkin JO, Hyland JM, et al. Primary colorectal lymphoma - A single centre experience. Surgeon 2015;13:151-5. [Crossref] [PubMed]
- Blackledge G, Bush H, Dodge OG, et al. A study of gastro-intestinal lymphoma. Clin Oncol 1979;5:209-19. [PubMed]
- Jinnai D, Iwasa Z, Watanuki T. Malignant lymphoma of the large intestine--operative results in Japan. Jpn J Surg 1983;13:331-6. [Crossref] [PubMed]
- Dawson IM, Cornes JS, Morson BC. Primary malignant lymphoid tumors of the intestinal tract. Report of 37 cases with a study of factors influencing prognosis. Br J Surg 1961;49:80-9. [Crossref] [PubMed]
- Drolet S, Maclean AR, Stewart DA, et al. Primary colorectal lymphoma – Clinical outcomes in a Population-Based Series. J Gastrointest Surg 2011;15:1851-7. [Crossref] [PubMed]
- Musallam KM, Hatoum HA, Barada K, et al. Primary colorectal lymphoma. Med Oncol 2010;27:249-54. [Crossref] [PubMed]
- Cai YB, Chen HY, He JJ, et al. The role of surgical intervention in primary colorectal lymphoma: A SEER population-based analysis. Oncotarget 2016;7:72263-75. [Crossref] [PubMed]
- Hwang WS, Yao JC, Cheng SS, et al. Primary colorectal lymphoma in Taiwan. Cancer 1992;70:575-80. [Crossref] [PubMed]
- Kim YH, Lee JH, Yang SK, et al. Primary colon lymphoma in Korea: a KASID (Korean Association for the Study of Intestinal Diseases) Study. Dig Dis Sci 2005;50:2243-7. [Crossref] [PubMed]
- Avilés A, Neri N, Huerta-Guzmán J. Large bowel lymphoma: an analysis of prognostic factors and therapy in 53 patients. J Surg Oncol 2002;80:111-5. [Crossref] [PubMed]


