Defining the distal margin of rectal cancer for surgical planning
Introduction
Rectal cancer is a common but serious disease for which the mortality rate is high. Despite major advances in surgical, radiologic, and oncologic treatments, the management of rectal cancer remains difficult, with a high local recurrence rate of up to 33% (1). Local recurrence is related to the surgeon’s skill and experience. Because of the risk of local recurrence and the associated poor prognosis, appropriate surgical resection is required. Patients’ quality of life is another issue, and for this reason, sphincter-sparing surgery has become a desirable option; it results in fewer complications than those associated with abdominoperineal resection (2).
The tumor location and the distal tumor margin are important factors upon which the surgical plan for patients with rectal cancer is based. Accurate measurement of the distal tumor margin is essential in planning the surgical procedure, even sphincter-saving resection. However, in the major rectal cancer trials, there has been no standard definition of the distal tumor margin in terms of the anal landmark used for measurement (3).
The National Cancer Institute consensus group recommends use of the anal verge (AV) in measuring the distal tumor margin (4). The AV is the outer margin of the anal canal and has, for decades, been recognized as an important anatomical landmark, especially since double contrast barium enema (BE) came into widespread use as the standard examination for colorectal cancer. The European Society of Gastrointestinal and Abdominal Radiology recommends use of the anorectal ring (ARR) as the landmark (5). The ARR is a muscular structure at the junction between the anal canal and the rectum and can be thought of as the top of the puborectalis muscle. It may be the best landmark because it is well defined by magnetic resonance imaging (MRI) and is not affected by the length of the anal canal.
In Asia, BE is still commonly used to evaluate both tumor volume and tumor location in patients with rectal cancer. However, in Western countries, preoperative assessment of rectal cancer has shifted toward MRI because it serves as an essential tool for investigating the relations between the tumor, the sphincter, and the levator ani muscle (6). Traditionally, rectal cancers located less than 5 cm from the AV or less than 2 cm from the ARR have been treated by abdominoperineal resection (7). Because a few centimeters can amount to a large difference for patients who desire a sphincter-saving procedure, determining the exact level of the tumor in the rectum is crucial in deciding upon the appropriate surgical procedure. An additional factor that influences measurement of the distal tumor margin and the distance between the tumor and the anal landmark is the imaging modality used. Neither the landmarks nor the imaging modality applied have been investigated in sufficient detail.
We conducted a retrospective study to evaluate whether a difference exists between BE and MRI in depiction of the level of the tumor in patients with rectal cancer. Included in our evaluation was an assessment of whether image-based measurement of the distal tumor margin should be to the AV or to the ARR.
Methods
Study patients
Included in the study were 52 patients (34 men, 18 women) with primary rectal cancer who underwent sphincter-saving resection between April 2014 and March 2015 and for whom both BE and MRI had been performed preoperatively. Median age of these patients was 67 (range, 45–90) years, and median body mass index was 21.5 (15.1–28.7). All patients provided written informed consent for the surgical procedure.
BE, MRI, and measurements for surgical planning
BE was performed as a standard double contrast study under fluoroscopic guidance, by which we monitored progression of the barium column, colon distension, and mucosal coating. The following spot and overhead radiographs were obtained: anteroposterior, posteroanterior, and lateral views of the rectum. MRI was performed with a 1.5-tesla magnet (GE Healthcare Japan, Tokyo, Japan) and axial T1-, T2-, and diffusion-weighted images were obtained through the pelvis as well as sagittal 3D Cube T2-weighted sequences at the level of the tumor in the rectum. All T1- and T2-weighted sequences were turbo spin echo sequences. The distance from the distal end of the tumor at the rectal wall to the AV and then to the ARR was measured on both BE and magnetic resonance (MR) images. All measurements were recorded in centimeters.
Statistical analysis
Distances from the distal margin of the cancer to the AV and the ARR were measured for all patients individually, and mean (SD) and median (range) values were calculated for the total patients. Wilcoxon matched-pairs analysis was applied to differences in measured distances between imaging modalities. A P value of ≤0.05 was considered statistically significant. Bland-Altman plots were constructed to show the difference between the BE- and MRI-based measurements against the mean of the two measurements for each patient. Pearson correlation coefficients were calculated, and proportional bias between the two methods was estimated with a test of non-correlation.
Results
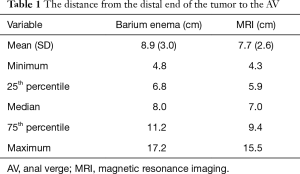
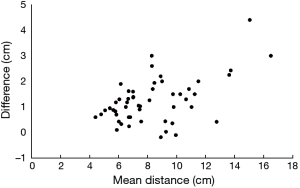
As shown on Table 1, mean distance from the distal end of the tumor to the AV was 8.9 (3.0) cm (median, 8.0 cm; range, 4.8–17.2 cm) on BE radiographs and 7.7 (2.6) cm (median, 7.0 cm; range, 4.3–15.5 cm) on MR images. The maximum difference between the BE-based and MRI-based distances to the AV was 4.7 cm, with a mean distance of 1.2 cm, and this difference was significant (P=0.013). Differences between the BE- and MRI-based measurements varied, as shown on the Bland-Altman plot in Figure 1. The plot also shows significant proportional bias: as the distance to the AV increased, the difference between the BE- and MRI-based measurements increased.
Full table
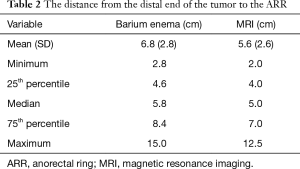
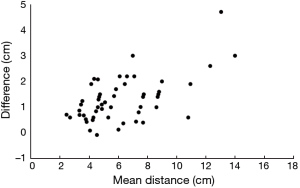
As shown on Table 2, mean distance to the ARR was 6.8 (2.8) cm (median, 5.8 cm; range, 2.8–15.0) cm on BE radiographs and 5.6 (2.6) cm (median, 5.0 cm; range, 2.0–12.5 cm) on MR images. This difference was not significant (P=0.070). Differences between these BE- and MRI-based measurements varied, as shown on the Bland-Altman plot in Figure 2, and a proportional bias was again evident: as the distance to the ARR increased, the difference between the BE- and MRI-based measurements increased. The mean difference from the distal tumor margin to the ARR was, like that to the AV, 1.2 (median 1.1; range, −0.8–4.4) cm, and the difference in measurements, whether to the AV or to the ARR, was not significant (P=0.74).
Full table
Discussion
Studies conducted in Japan have documented 98–100% correspondence between the location of the tumor as detected on BE radiographs and the location of the tumor determined at the time of surgery. The reported correspondence when MRI is used is 75–83%. However, the precise difference between measurements determined by means of the two modalities was not described (8). We found an average difference of 1.2 cm in our total patient group. When the distance met the standard criteria for choosing a sphincter-preserving procedure, i.e., less than 5 cm to the AV or less than 2 cm to the ARR, the mean differences were 0.78 and 0.87 cm, respectively. The depth of extramural tumor spread and involvement of the mesorectal fat and mesorectal fascia are important factors when it comes to treatment planning. MRI is an excellent tool for depicting the tumor and the mesorectal fat by showing the contrast between them and also showing relations between the tumor, the sphincter, and the levator ani muscle. Reported agreement between MRI and pathologic T staging has ranged from 66% to 94% (9,10). MRI is often preferred because it contributes to both tumor detection and preoperative staging of the rectal cancer without radiation exposure, which poses a slight carcinogenic risk. BE remains an important complementary modality for evaluating the colon when intestinal stenosis prevents colonoscopy, and, over the past 40 years, BE has been widely used in Asia, including Japan, as the most cost-effective screening tool. BE is believed to be safer than colonoscopy, and it shows the shape of the colon more precisely than does MRI (6). In cases of rectal cancer, a distal resection margin greater than 2 cm is considered optimal for avoiding local recurrence. The anal canal is approximately 3–4 cm in length; thus, rectal cancers located less than 5 cm from the AV are not generally considered for sphincter-saving resection (11). Therefore, the distance from the distal end of the tumor to the AV is an important factor in determining whether sphincter-sparing surgery can be performed. If the distance is inadequate, patients must undergo standard abdominoperineal resection, i.e., removal of the rectum with the anal sphincter complex, before creation of an abdominal colostomy. Complete tumor resection that spares the anal sphincters serves to preserve patients’ quality of life.
Accurate measurement of the distal tumor margin is essential in planning the surgical procedure, but there is no standard definition that accounts for the imaging modality used. Ferri et al. (12) described measuring the distance from the distal tumor margin to the ARR on MR images to assess whether sphincter-sparing resection with an adequate tumor margin is feasible in their patients. They reported that invasion of the anal sphincter was correctly identified by means of MRI in 87% of their patients.
In our study, we evaluated and compared two imaging modalities for measurements upon which to base a decision to perform sphincter-preserving resection. We believe that when BE is performed, air pumped into the colon to achieve a double contrast effect is responsible for the difference we found between BE- and MRI-based measurements. We documented an average difference of 1.2 cm, which hitherto had not been reported. Whether the AV or ARR was used as the landmark, the results were the same.
We also found that the difference between MRI- and BE-based measurements increased as the distance from the AV increased. The maximum difference was 4.7 cm to the AV and 4.4 cm to the ARR, and these values are enough to warrant a change in the surgical plan from abdominoperineal resection to sphincter-saving resection. In fact, the tumor in 8 (15.3%) of our patients was less than 5 cm from the AV upon MRI-based measurement. On BE radiographs, however, the tumor was more than 5 cm from the AV in five of these eight patients. All eight patients were treated by sphincter-saving resection, some of whom might have undergone abdominoperineal resection if we had not relied on the MRI-based measurements.
Our study results appear to be of clinical importance. The difference between modalities in the resulting measurements is a critical factor upon which surgical decisions should be made. Rectal cancers initially determined on BE radiographs to be less than 5 cm from the AV might actually be indicated for sphincter-preserving resection.
MRI is being used increasingly for preoperative evaluation of rectal cancer. However, the distance from the distal tumor margin to the chosen anal landmark, which is a key factor in the feasibility of sphincter-sparing surgery, may be underestimated by MRI-based measurement. Clinicians should bear in mind that BE can more precisely locate the tumor within the rectum.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Moriya Y. Treatment strategy for locally recurrent rectal cancer. Jpn J Clin Oncol 2006;36:127-31. [Crossref] [PubMed]
- Ghieda U, Hassanen O, Eltomey MA. MRI of rectal carcinoma: Preoperative staging and planning of sphincter-sparing surgery. Egypt J Radiol Nucl Med 2014;45:1-5. [Crossref]
- Keller DS, Paspulati R, Kjellmo A, et al. MRI-defined height of rectal tumours. Br J Surg 2014;101:127-32. [Crossref] [PubMed]
- National Institutes of Health. National Cancer Institute. Rectal Cancer Treatment (PDQ®)–Health Professional Version. Available online: http://www.cancer.gov/types/colorectal/hp/rectal-treatment-pdq
- Beets-Tan RG, Lambregts DM, Maas M, et al. Magnetic resonance imaging for the clinical management of rectal cancer patients: recommendations from the 2012 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 2013;23:2522-31. [Crossref] [PubMed]
- Murono K, Kawai K, Tsuno NH, et al. Barium enema and CT volumetry for predicting pathologic response to preoperative chemoradiotherapy in rectal cancer patients. Dis Colon Rectum 2014;57:715-24. [Crossref] [PubMed]
- Lichliter WE. Techniques in total mesorectal excision surgery. Clin Colon Rectal Surg 2015;28:21-7. [Crossref] [PubMed]
- Koshiduka S, Yamanoha K. Usefulness of the double contrast barium enema in the anorectal region. J Jap Soc Gastrointest Image 2015;10:55-8.
- Brown G, Radcliffe AG, Newcombe RG, et al. Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg 2003;90:355-64. [Crossref] [PubMed]
- Videhult P, Smedh K, Lundin P, et al. Magnetic resonance imaging for preoperative staging of rectal cancer in clinical practice: high accuracy in predicting circumferential margin with clinical benefit. Colorectal Dis 2007;9:412-9. [Crossref] [PubMed]
- Ota DM, Jacobs L, Kuvshinoff B. Rectal cancer: the sphincter-sparing approach. Surg Clin North Am 2002;82:983-93. [Crossref] [PubMed]
- Ferri M, Laghi A, Mingazzini P, et al. Pre-operative assessment of extramural invasion and sphincteral involvement in rectal cancer by magnetic resonance imaging with phased-array coil. Colorectal Dis 2005;7:387-93. [Crossref] [PubMed]


